Libby Welch / Alamy Stock Photo
Prescription charges did not figure large in the 2017 general election campaign but the argument over whether charges should be abolished outright in England or reintroduced in the home nations was certainly a feature — and one that is set to get more discussion over coming months as a new report highlights the hidden cost of prescription charges.
The report, ‘Still paying the price: prescription charges and people with long term conditions’, details how in this age of austerity, working-age people on low incomes are rationing their medicines because they cannot afford to fill all their prescriptions[1]
.
The report’s findings are reflected in figures released by the National Rheumatoid Arthritis Society (NRAS), which reveals that nearly a third (31%) of people with rheumatoid arthritis (RA) who have been issued a prescription by their GP have not collected it because of the cost. More than half of those people said that not taking their medicines had resulted in a direct and noticeably negative impact on their health.
According to NRAS figures, 76% of those surveyed are not aware of the NHS low income scheme, and 50% do not have a Prescription Prepayment Certificate as they felt it was not worth obtaining one or it was too expensive for a fluctuating condition.
Nearly 700,000 people in the UK have RA, costing the NHS approximately £560m per year[2]
. The National Audit Office estimates that the total cost of RA to the UK economy is £4.8bn per year.
Ailsa Bosworth, chief executive of NRAS says: “The fact that so many people living with this disease are failing to get the help their GPs prescribe in terms of medicine is a travesty.
“Everyone, regardless of their medical condition, should receive the medication they need to manage their health and improve their daily life.”
Controversial from the outset, prescription charges were introduced in 1952, abolished in 1965 and reintroduced in 1968 with a system of exemptions that persists in modified form today. The charge itself has risen from 20p in 1979 to the current price of £8.60 per item.
Scotland, Wales and Northern Ireland abolished prescription charges in 2011, 2007 and 2010, respectively, but in England they remain, albeit for around only 10% of the population.
It seems there are two main issues. One is the perceived unfairness of the English charging structure that sees patients with certain long-term conditions qualify for free prescriptions while others do not[3]
. A cancer diagnosis qualifies patients to apply for an exemption card but asthma does not, for example.
Austerity generating bigger NHS bill
The second issue centres on austerity. Should charges be reintroduced in Wales, Scotland and Northern Ireland to help generate income (or contain costs) for the NHS? Or is the squeeze on wages and the rising cost of prescriptions leading to fewer people filling their prescriptions because they cannot afford the £8.60 charge — creating unmet health needs and ultimately generating a bigger NHS bill further down the line?
The Prescribing Charges Coalition (PCC) has argued for years that the burden of prescription charges in England is borne by working-age people on low incomes living with long-term conditions. Prepayment certificates, says the coalition, are poorly understood, poorly publicised and at any rate are not affordable[4]
.
As part of its report, the coalition surveyed more than 5,600 people living with long-term conditions, including 4,200 people who pay their own prescription charges. Three in ten of these self-payers admitted skipping prescriptions or reducing their medications. For many of them, cost was a key factor. They were getting sick as a result, with three in five needing to take time off work and one-third needing to visit their GP.
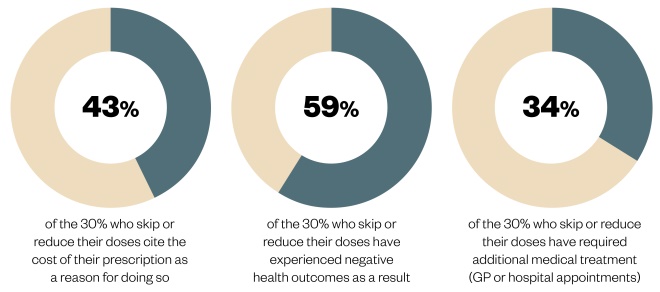
Figure 1: Effects of non-adherence
Source: Prescription Charges Coalition (PCC)
Among those patients with long-term conditions surveyed in England, 30% of those who pay for their prescriptions sometimes or often skip or reduce recommended doses of medication, resulting in negative health outcomes or additional treatment
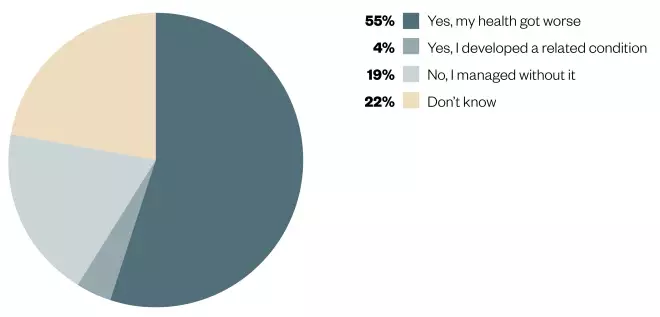
Figure 2: Effects of non-adherence due to prescription charges
Source: Prescription Charges Coalition (PCC)
Out of the 30% who reported reducing or skipping doses of their medication, 59% stated that either their health deteriorated or that they had developed a related condition as a result
Laura Cockram, head of policy and campaigning at Parkinson’s UK (which co-chairs the PCC) says: “We have heard distressing and alarming experiences from people who are facing impossible choices over whether they should eat, heat their home or pay for essential medications to treat life-threatening conditions.
“The situation is dangerous and goes against the very principle of our NHS.”

Courtesy of Parkinson’s UK
Laura Cockram, head of policy and campaigning at Parkinson’s UK says: “We have heard distressing and alarming experiences from people who are facing impossible choices over whether they should eat, heat their home or pay for essential medications”
She points out that the charges are draining vital resources, costing the NHS more in the long term, owing to people’s need to access GP and hospital care when they cannot afford their medication.
The PCC estimates it would cost £360m–£430m to provide free prescriptions to working-age people with long-term conditions and argues that this is less than the hidden cost of them not taking medication because they cannot afford it.
The Royal Pharmaceutical Society (to which this journal belongs) also wants to see an end to all prescription charges, not just because they are unfair and a disincentive to maintaining good health but also because of the time and administrative burden involved in the system[5]
.
Spokesperson Neal Patel says: “Pharmacists want to spend time helping people get the most out of their medicines, not collecting prescription charges and checking exemptions to fees. The current exemption system is outdated, arbitrary and unfair, and the main burden falls on those with long-term conditions such as HIV, asthma and multiple sclerosis who have to pay for prescriptions to stay well.”
Prescription costs place a particular squeeze on the finances of those who are in work on modest incomes, who sometimes cannot afford prescription medicines, a price that is ultimately paid in preventable hospital admissions, wasted NHS time and avoidable sick leave.
Cost of free prescriptions
In Scotland, Northern Ireland and Wales, removing prescription charges was presented as an investment in the health of the population and a way to increase fairness. In Northern Ireland, for example, the then health minister Michael McGimpsey said on the introduction of free prescriptions for all: “It is an economic investment, as people will be able to get back to work earlier if they have the right medication. It is also an investment in people, at a time when they need it most”[6]
.
Nicola Sturgeon, health minister in Scotland in 2011 when charges were abolished, claimed charges were a “tax on ill health”.
Today, Andrew Evans, the Welsh Government’s chief pharmacist, defends free prescriptions on similar grounds. He says: “The free prescription policy in Wales is a long-term investment to improve people’s health. Providing people with the medication they need helps to keep them well and out of hospital, reducing the overall cost to the NHS.”
And yet, the question of whether charges should be reintroduced keeps coming up as new data show ever-rising numbers of prescriptions. But, say pharmacists, there is precious little evidence that removing charges is driving this increase.
Recent data from Wales provides a good case study. Welsh Government data released in May 2017 show that community prescribing in Wales tops the UK league table with 25.9 items per head of population compared with 21.9 in Northern Ireland, 20.2 in England and 19.1 in Scotland[7]
.
Overall, the number of prescription items dispensed in the community increased from 79.5 million in 2015 to 80.3 million in 2016 (up by 1%) although the net ingredient cost of all prescriptions dispensed in the community decreased by 2.7% since 2015, to £578m in 2016.
Despite what a cursory glance at the numbers might suggest, Evans says the data do not demonstrate a link between rising prescription rates and the abolition of prescription charges in Wales in 2007. Wales has a higher proportion of over-65s and a higher prevalence of chronic disease, both factors that drive prescribing growth nationally.
Fewer prescriptions in no-charge areas
He points out that the rate of growth at 1% was the lowest for many years. He says: “The rate of increase in GP prescribing in Wales is lower than in England. Between 2007, when we removed prescription charges, and 2015, the number of prescriptions dispensed in England increased by 36% compared with an increase of only 28% in Wales.”
There is no evidence that non-adherence or medicine waste is greater in Wales, he adds.
Evans says the latest data do not present a case for re-examining the free prescription policy in Wales and is backed by All Wales Chief Pharmacists Committee, chaired by Judith Vincent who is clinical director for pharmacy at Abertawe Bro Morgannwg Health Board.

Source: Nick Treharne
Judith Vincent, clinical director for pharmacy at Abertawe Bro Morgannwg Health Board says that the reasons why Wales is prescribing higher numbers of prescriptions per head of population are multifactorial and complex
She says: “The reasons [why Wales is prescribing higher numbers of prescriptions per head of population] are multifactorial and complex. There is no straight answer that says free prescribing generates greater volumes of prescriptions.”
The BMA in Wales also defends the free prescription policy. Dr David Bailey, deputy chair of the Welsh GP Committee, says: “The main reason for the free prescription policy is that Wales has poorer health and wealth than other parts of the UK and that leads to higher prescriptions.”

Courtesy of David Bailey
Dr David Bailey, deputy chair of the Welsh GP Committee, says: “The main reason for the free prescription policy is that Wales has poorer health and wealth than other parts of the UK and that leads to higher prescriptions”
It would be fairer to compare prescribing rates in Wales to those in North East England rather than England as a whole, he adds.
Berwyn Owen, chief pharmacist in Betsi Cadwaladr Health Board, agrees: “The policy within Wales around free prescriptions is to ensure access to medicines to manage complex needs for everyone.”
He says the long-standing difference in prescribing rates between England and Wales has been consistent since at least 1999 and is partly explained by differences in deprivation.

Source: Nick Treharne
Berwyn Owen, chief pharmacist in Betsi Cadwaladr Health Board, says that the policy within Wales on free prescriptions is to ensure access to medicines to manage complex needs for everyone
He adds: “The recent Auditor General’s report also acknowledges that there is some evidence that the average interval between prescriptions in Wales may be shorter than in other parts of the UK, linked to national guidance on the use of a 28-day prescribing interval for repeat medicines, this may have the effect of artificially inflating the number of prescription items per head of population[8]
.”
The PCC also agrees that the data do not provide a case for reintroducing charges.
Emma Webb, of Parkinson’s UK and co-chair of the PCC, says the rate of prescribing increase in Wales has slowed since the abolition of charges, from a yearly average of 4.5% in the years 2000–2006 to 2.4% from 2008–2016[9]
,[10]
. Scotland, which abolished charges in 2011, has the lowest prescribing rate.
She says: “There is no indication here that high levels of dispensing in Wales relates to the absence of prescription charges in the country… We can also see from the data that the number of prescriptions dispensed per head remains lower in Scotland than any other part of the UK, despite Scotland having scrapped prescription charges in 2011. The data prove that it is wrong to assume that free prescriptions have an impact on demand for treatment.”
Evans points out that any re-introduction of charges would require the development of a new, fairer system. To maintain such a system would require a costly framework for determining who should not be charged, who may be exempt from charges and who may be entitled to full or part remission of charges, he says.
“The costs associated with administering this fairer system and then safeguarding that system against misuse would significantly reduce any potential income derived from the re-introduction of a charging regime. It would also negate the very real health benefits we believe Welsh citizens gain by removing the ability to pay as a key consideration when an individual takes their prescription for dispensing.”
It is an argument that is set to run and run, although one that has precious little political leverage in England. The PCC hopes that their new research will provide some.
Politics of prescription charges
The issue of prescription charges did come up a few times in the last general election. The Liberal Democrats’ manifesto stopped short of calling for prescriptions charges to be abolished in England but pledged to “review the rules for exemption from prescription charges to ensure they are fair to those with long-term conditions and disabilities[11]
.”
The Green Party went a step further and announced a policy to abolish all prescription charges. The policy of charging, said Green Party leader Caroline Lucas, was forcing some people to choose between food and medication, which was not acceptable.
The situation in Scotland was rather different. Scottish Conservatives have been against the free prescription policy since its introduction in 2011 and pledged to reintroduce charges during last year’s Holyrood election campaign, saying free prescriptions had cost the Scottish NHS £60m.
Come the 2017 general election, however, the Scottish Conservative leader Ruth Davidson acknowledged the popularity of the free prescription policy, dropped her opposition to it and pledged instead to examine the use of “low-value prescriptions” from GPs.
Meanwhile in Wales, the Welsh Conservatives continued with their line that people who can afford to pay for prescriptions should do so, pointing towards rising prescription rates in Wales.
It was a non-issue for the Conservative Party in England, which directed The Pharmaceutical Journal to the Department of Health as this is “government policy”.
NHS prescription charges generated £523m last year and in England, the appetite is for introducing more charges for NHS patients — not abolishing them[12]
. A Department of Health spokesperson says: “We have made sure that people with long-term conditions can get access to affordable prescriptions. That is why there are several prescription charge exemptions in place, and 90% of items prescribed are free on the NHS in England.”

Courtesy of Parkinson’s UK
Emma Webb, of Parkinson’s UK and co-chair of the PCC, says the rate of prescribing increase in Wales has slowed since the abolition of charges, from a yearly average of 4.5% in the years 2000–2006 to 2.4% from 2008–2016
But Webb issues a salutary warning: “With inflation reaching its highest point in four years and a worsening squeeze on wages, living costs are higher than ever. This is increasing the likelihood of people across England, who rely on regular medication to manage long-term conditions, being unable to afford their prescriptions.
“Next year will mark 50 years since the creation of the medical exemption list for prescription charges in England, which has barely been updated since 1968. We believe it is grossly unfair that some conditions are exempt from all charges, while people with other long-term conditions are required to pay in order to stay well. It is the government’s duty to support everyone with a long-term condition to access the medication they need. We urge them to correct this historic injustice.”
References
[1] Still Paying the Price: Prescription charges and people with long term conditions. Report by the Prescription Charges Coalition June 2017. Available at: https://www.parkinsons.org.uk/sites/default/files/still_paying_the_price_june_2017.pdf (accessed July 2017)
[2] National Rheumatoid Arthritis Society. Key facts. Available at: http://www.nras.org.uk/for-journalists (accessed July 2017)
[3] NHS in England. Help with health costs. Available at: http://www.nhs.uk/NHSEngland/Healthcosts/Pages/Prescriptioncosts.aspx (accessed July 2017)
[4] Paying the Price: Prescription charges and people with long term conditions. A report by the Prescription Charges Coalition. 2013. Available at: http://www.prescriptionchargescoalition.org.uk/uploads/1/2/7/5/12754304/paying_the_price_report.pdf (accessed July 2017)
[5] Dajani S. The prescription charge system is illogical, unfair and morally indefensible. Pharm J 24 Feb 2015. doi: 10.1211/PJ.2015.20067910
[6] Northern Ireland Assembly. Prescriptions: Costs and charges in the UK and Republic of Ireland. Research and Information Service Briefing Note. Available at: http://www.niassembly.gov.uk/globalassets/documents/raise/publications/2014/general/6114.pdf (accessed July 2017)
[7] Welsh Government. Prescriptions dispensed in the community. May 2017. Available at: http://gov.wales/statistics-and-research/prescriptions-dispensed-community/?lang=en (accessed July 2017)
[8] Auditor General for Wales. Managing medicines in primary and secondary care. December 2016. Available at: https://www.wao.gov.uk/system/files/publications/Medicines-management-2016-english.pdf (accessed July 2017)
[9] Calculations based on figures in Chart 2 for the years 2000–2006. Available at: http://gov.wales/docs/statistics/2017/170524-prescriptions-dispensed-community-2016-en.pdf (accessed July 2017)
[10] Calculations based on figures in Chart 2 for the years 2008–2016. Available at: http://gov.wales/docs/statistics/2017/170524-prescriptions-dispensed-community-2016-en.pdf (accessed July 2017)
[11] Liberal Democrat election manifesto 2017. Available at: http://www.libdems.org.uk/health (accessed July 2017)
[12] The Prescription charge and other NHS charges. House of Commons Briefing paper number 07227, 16 March 2017. Available at: http://researchbriefings.parliament.uk/ResearchBriefing/Summary/CBP-7227 (accessed July 2017)
You may also be interested in

Government proposes raising qualifying age for free NHS prescriptions to 66 years

Labour government would axe prescription charges, says shadow health secretary
