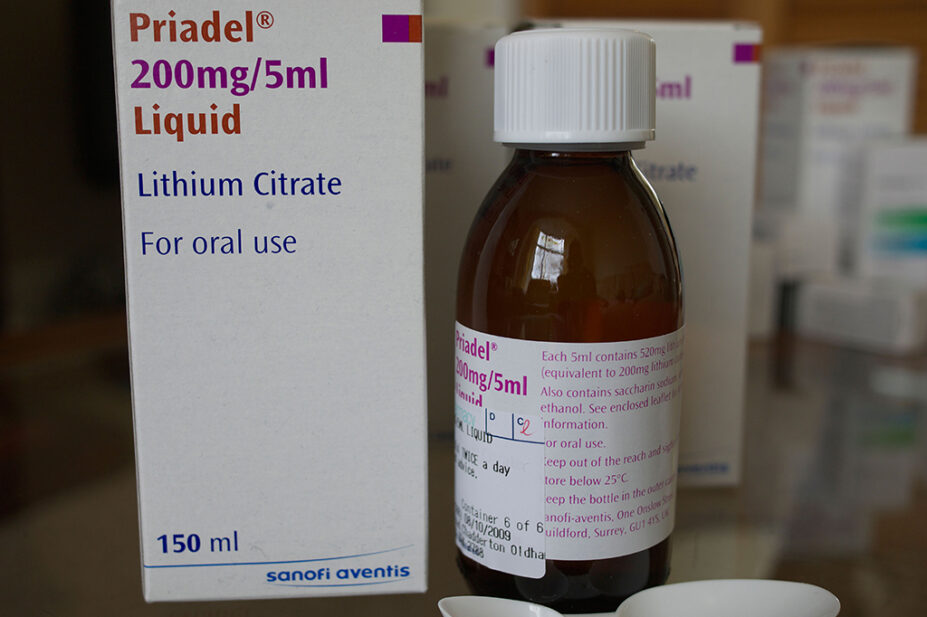
jozef mikietyn / Alamy Stock Photo
More than one third of patients taking lithium are not aware of the warning signs of toxicity when taking the drug, a community pharmacy-led safety audit has found.
Patients were audited as part of the 2019/2020 Pharmacy Quality Scheme (PQS), which required community pharmacy contractors to ask patients taking lithium, methotrexate, amiodarone or phenobarbital a series of questions based on current safety guidance.
The audit was designed primarily to investigate the safety of prescribing for lithium, with contractors asked to audit all patients taking lithium over a three-month consecutive period between September 2019 and February 2020.
However, if pharmacies had not dispensed lithium in the previous three months, they were asked instead to audit people taking methotrexate, amiodarone or phenobarbital.
Some 10,673 pharmacy contractors took part in the audit, which covered a total of 40,419 patients.
Of the 21,883 patients taking lithium who participated in the audit, 34% were unable to describe the signs of lithium toxicity and 29% did not know how to prevent toxicity by ensuring plenty of fluid intake.
Symptoms of toxicity include diarrhoea, vomiting, stomach pains and weakness, and can be fatal if severe.
As a result, the audit report, published on 20 March 2023, recommends pharmacy teams “be proactive in counselling on the signs and symptoms of toxicity of high-risk medicines and advise how to reduce adverse reactions”.
The results also showed that 19% of patients prescribed lithium reported not having their weight measured in the past 6 months, while 18% of patients did not know what to do if they missed a dose of lithium.
According to the National Institute for Health and Care Excellence (NICE), patients taking lithium should have their weight or body mass index measured every six months. NICE also recommends patients have their plasma lithium levels monitored every three to six months.
According to the audit, 95% of patients prescribed lithium had their plasma lithium levels monitored in the past three to six months.
“The majority of patients confirmed that they received the appropriate blood monitoring, but there was a concerning minority who had not, all of whom should be referred to their GP practice,” the audit report said.
The report added that pharmacy contractors provided additional counselling and advice a total of 23,957 times during the audit, in response to patients whose answers to the audit questions suggested this was required.
Thorrun Govind, chair of the Royal Pharmaceutical Society’s English Pharmacy Board, said the audit’s findings “demonstrate the important role that pharmacists play as health educators, informing patients and their carers of the signs of medicines toxicity”.
“Community pharmacy was able to identify a concerning number of patients without appropriate blood monitoring,” she said.
“Addressing referral pathways and access to records could allow pharmacists the ability to reduce these risks further.”
Recommendations for community pharmacists for patients taking lithium
- Patients who report being overdue blood monitoring should be referred to their GP practice;
- Pharmacy teams should be proactive in counselling on the signs and symptoms of toxicity of high-risk medicines and advise how to reduce adverse reactions;
- It is good practice to record details such as the date and time of blood monitoring results and therapeutic drug levels on the patient medication record;
- Pharmacy teams should routinely discuss how to maintain a healthy lifestyle with patients at the point of handing out these medicines;
- Community pharmacy teams should ensure all patients have access to information and advice so they can fully understand how to take the medication. Not all patients have equal awareness, understanding and access to primary care and pharmacy teams have an important role in ensuring that individually tailored advice is provided. Pharmacy teams should be mindful of communication preferences for patients with disabilities or when English is not their first language, as outlined in the accessible information standard.
Source: Community Pharmacy Quality Scheme 2019/20 high risk medicines audit report


