Key points
- The use of ‘psychoactive pharmaceuticals’ and ‘pharming’ are increasingly reported phenomena involving the non-medical use of prescription (e.g. pain relievers, tranquilisers, stimulants, sedatives) and OTC drugs (e.g. loperamide, promethazine, antitussive cough syrups), either on their own or in combination with other licit or illicit substances, for recreational purposes.
- A range of medications have emerged as misused and diverted, or are known anecdotally to be used, or already described through the literature or pharmacovigilance datasets, as well as recorded by drug users’ online websites reporting new trends and experimentations of drug abuse.
- Drug use habits and availability may have changed as a result of the COVID-19 pandemic, causing a shift in behaviours relating to both prescription and OTC medicines.
- Pharmacists should play a key role in preventing and reducing drug abuse and be involved in evidence-based actions to detect, understand and prevent drug diversion activities and drug misuse adverse effects.
Source: Shutterstock.com
Pharmacists have an important role to play in preventing and reducing abuse of prescription and over-the-counter medicines
Introduction
In recent years, drug abuse scenarios have evolved owing to the appearance of novel psychoactive substances (NPSs) and the recreational use of pharmaceuticals[1],[2],[3],[4]
. Misuse of prescription drugs is a growing health problem, involving not only specific drug-related risks, but also the context in which they are consumed (e.g. the concomitant abuse of other substances with synergistic effects, psychiatric diagnoses and social circumstances)[4],[5],[6],[7],[8]
.
Therefore, side effects, drug interactions and individual variation in responses (owing to existing comorbidities [such as a mental disorder, renal or hepatic dysfunction, systemic diseases] and previous substance abuse or dependence) might be associated with a range of severe adverse drug reactions (ADRs), including seizures, arrhythmias, respiratory arrest and fatalities[2],[9],[10],[11]
. In this context, ‘pharming’ is a new, worldwide phenomenon involving the non-medical use of prescription (e.g. pain relievers, tranquilisers, stimulants, sedatives) and over-the-counter (OTC) drugs (e.g. those containing dextromethorphan and promethazine)[2],[7],[12],[13],[14],[15]
.
According to data from the United Nations Office on Drugs and Crime (UNODC), the prevalence of prescription drug misuse and related fatalities is increasing worldwide[16],[17],[18]
. Vulnerable groups at higher risk of misusing medications are adolescents and young adults; women; older adults; and healthcare professionals[19]
. Other at-risk groups include people with mental illnesses, inmates and individuals suffering from acute or chronic pain, who might abuse opiate medications[17]
. A range of factors are thought to contribute to the non-medical use of prescription/OTC drugs, such as:
- The perception of prescription drugs as more socially acceptable;
- Less stigmatising;
- Safer than the intake of illicit substances, as well as their likely lack of detection in standard drug screens[13]
.
This article aims to undertake a comprehensive review of the relevant literature describing the drugs primarily associated with potential diversion, typical patterns of their misuse and harms associated with medicine abuse; report factors that might influence and exacerbate diversion in the current COVID-19 crisis; and consider how pharmacists can reduce and prevent substance abuse.
Material and methods
A literature search was performed on PubMed, Medline and Web-of-Science in May 2020 and covered the past 20 years. We used combinations of the following search terms [Title/Abstract]: ‘prescription drug’, ‘non-prescription drug’, ‘over-the-counter drug’, ‘misuse’, ‘abuse’, ‘non-medical use’, ‘addiction’ and ‘dependence’. Additional searches were then undertaken based on identified medicines, and these included ‘gabapentinoid’, ‘antidepressants’, ‘antipsychotics’, ‘Z-drugs’, ‘dextromethorphan’, ‘antihistamine’, ‘loperamide’, ‘benzydamine’, ‘pseudoephedrine’ and ‘scopolamine’.
Finally, authors performed further secondary searches by using the reference listing of all eligible papers. All titles/abstracts were examined, and full texts of potentially relevant papers obtained. Relevant works were chosen to obtain a full representation of the available literature on the selected topic. Experimental and observational studies; post-marketing surveillance reports; case reports; case series; and fatalities reports were included. The exclusion criteria included: non-original researches (e.g. review, commentary, editorial, book chapter, letter to the editor); non-full-text articles (e.g. meeting abstract); works in a language other than English; animal/in vitro studies; and articles that did not cover the abuse/misuse/dependence of the selected drugs.
Opioids and benzodiazepines are traditionally misused and, even though mostly controlled through regulation, are still diverted and associated with risky behaviours and higher overdose risk[18]
. The emergence of potent new, ‘designer’ benzodiazepines or new, synthetic opioids on the drug market is a reason for continued concern[20],[21]
. These medicines were excluded from this review as these categories require additional insight that is beyond the scope of this work. Image and performance-enhancing drugs were excluded from consideration in this review because their typical pattern of use is quite different from a typical recreational value (e.g. aesthetic use, competitive bodybuilding)[22],[23]
. Similarly, cognitive enhancers were not considered in this review because their primary use is to maintain wakefulness, improve recall and enhance executive functions[22],[24]
.
Definitions
‘Abuse’ was specifically defined as the intentional, non-therapeutic use by a patient or consumer of a product, OTC or prescription medicine, for a perceived reward or desired non-therapeutic effect including, but not limited to, getting ‘high’ (euphoria)[25]
.
‘Misuse’ was defined as the intentional use, by a patient or consumer of a product, OTC or prescription medicine, for a therapeutic purpose other than as prescribed or not in accordance with the authorised product information[25]
. ‘Drug misuse’ is used to distinguish improper or unhealthy use from the use of medicine as prescribed or alcohol in moderation[19]
. These include the use of drugs to produce pleasure, alleviate stress, and/or alter or avoid reality[19]
.
‘Addiction’ refers to a chronic, relapsing disorder characterised by compulsive drug seeking, continued use despite harmful consequences, and long-lasting changes in the brain[19]
.
‘Dependence’ refers to a maladaptive pattern of substance use leading to clinically significant impairment or distress[26]
. It is manifested by three or more of the following criteria, occurring at any time in the same 12-month period:
i) Tolerance;
ii) Withdrawal;
iii) Taking the substance often in larger amounts or over a longer period than was intended;
iv) Having a persistent desire or unsuccessful efforts to cut down or control substance use[26]
.
Physical dependence developed as a result of physiological adaptation in response to repeated drug use, manifested by withdrawal signs and symptoms after abrupt discontinuation or a significant dose reduction of a drug. Psychological dependence refers to a state in which individuals have impaired control over drug use based on the rewarding properties of the drug (ability to produce positive sensations that increase the likelihood of drug use) or the psychological distress produced in the absence of the drug[26]
. In 2013, the American Psychiatric Association (APA) updated the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), replacing the categories of substance abuse and substance dependence with the unique category of substance use disorder (SUD)[27]
.
Publications and findings
A total of n=314 publications were identified; after removing duplicates (n=9), and applying the exclusion criteria, a total of n=74 papers were retrieved and analysed. The findings are described in detail, organised in relation to the specific drug/group of drugs (see Table and supplement[1],[7],[9],[12],[28],[29],[30],[31],[32],[33],[34],[35],[36],[37],[38],[39],[40],[41],[42],[43],[44],[45],[46],[47],[48]
).
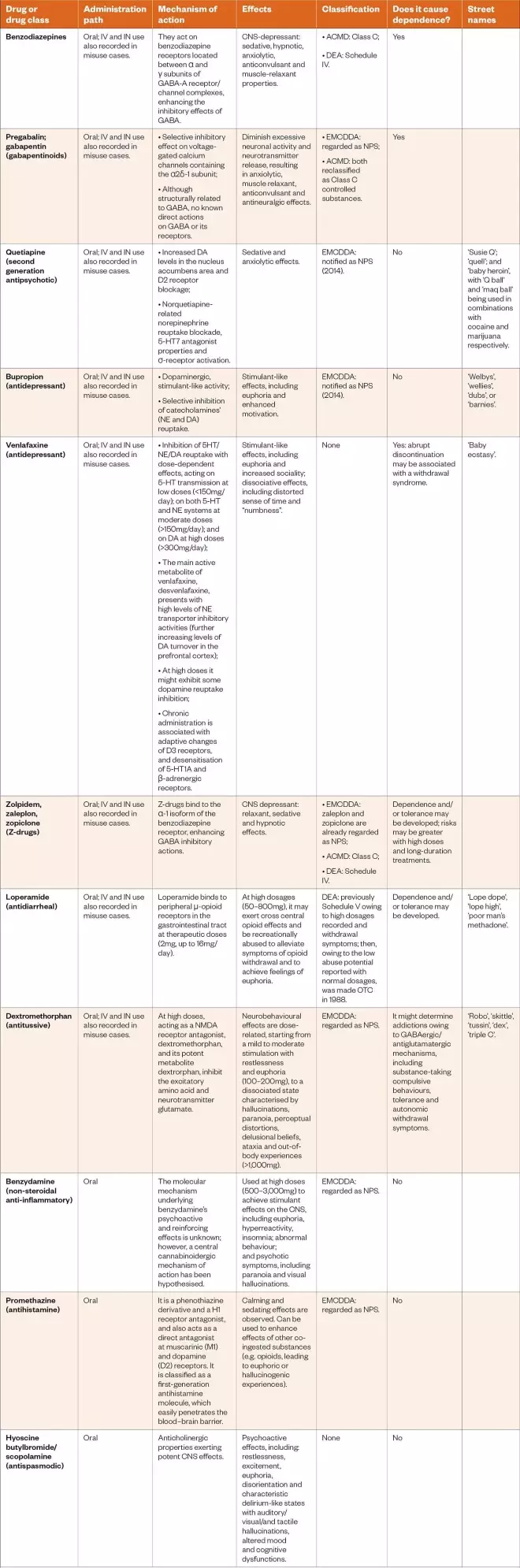
Table: Drug classification and the main characteristics relevant to pharmacists and other healthcare professionals
ACMD: Advisory Council on the Misuse of Drugs; DEA: Drug Enforcement Administration; DA: dopamine; EMCDDA: European Monitoring Centre for Drugs and Drug Addiction; GABA: gamma-amino-butyric acid; H: histamine; IN: intranasal; IV: intravenous; CNS: central nervous system; NE: norepinephrine; NPS: new psychoactive substance; OTC: over-the-counter; 5-HT: serotonin
Sources: Curr Opin Pediatr
[7]
, Psychol Med
[9]
, Subst Abuse Rehabil
[
12]
, Addict Behav
[28]
, Eur Neuropsychopharmacol
[29]
, J Clin Psychopharmacol
[30]
, Subst Abuse Rehabil
[31]
, Hum Psychopharmacol
[32]
, Subst Use Misuse
[33]
, Basic Clin Pharmacol
[34]
, Eur J Pediatr
[35]
, Basic Clin Pharmacol Toxicol
[36]
, J Psychoactive Drugs
[37]
, Braz J Psychiatry
[38]
, Addiction
[39]
, South Med J
[40]
,
PLoS One
[41]
, CNS Neurosci Ther
[42]
, Riv Psichiatr
[43]
, Cambridge University Press
[44]
, Am J Addict
[45]
, J Addict Med
[46]
, Subst Use Misuse
[47]
, Health Policy
[48]
Download the full PDF version of the table here.
Prescription drugs misuse
Prescription drug abuse has become a concerning modern-day epidemic[49],[50],[51]
. This is especially true among young adults and adolescents, where their use has surpassed all use of illicit drugs, with the exception of marijuana[52],[53]
. Traditionally, concern has centered on opioids, benzodiazepines and stimulants, but other widely prescribed drugs may be misused, abused or diverted for non-medical purposes[54]
. Young people take prescription drugs for recreational purposes (e.g. to get ‘high’); to relieve anxiety or relax; or to improve academic performance[5],[7],[8],[55]
. Drugs might be acquired from friends or relatives, directly prescribed by a doctor, obtained from a drug dealer or via the internet[2],[56],[57]
. Although there is little nationwide data on the prevalence of prescription drug abuse among young people in the UK, there are an increasing number of reports to suggest the problem is growing[16]
.
Quetiapine
According to the literature, quetiapine appears to be the most documented second-generation antipsychotic being abused because of its sedative, relaxant and anxiolytic characteristics[58],[59]
. High rates of quetiapine-related ambulance attendances/emergency department visits have been reported: data from the Drug Abuse Warning Network (DAWN) for prevalence of emergency department (ED) visits among the US general population involving quetiapine showed an increase between 2005 and 2011, from 35,581 ED visits to 67,497[60]
. Similar data regarding increasing quetiapine rates of ambulance attendances have been recorded in Australia, and associated with concurrent heroin and opioid replacement therapy toxicity, history of heroin and alcohol misuse, and mood disorders[61]
.
Moreover, drug-seeking behaviours, such as an illicit drug provision, and an increase in quetiapine availability on the black market, have been registered[62]
. Prison inmates, psychiatric outpatients, users with a history of drug misuse and opioid addicts represent the most at-risk of misusing populations[30],[47]
. Finally, intranasal and intravenous routes of consumption have been described[63]
.
Gabapentinoids
Gabapentin and pregabalin are approved treatments for epilepsy and neuropathic pain disorders[44],[64],[65]
. Both have increasingly been reported for their misuse potential; however, pregabalin is considered to have a higher abuse potential owing to its rapid absorption, faster onset of action and higher potency[29],[42],[66],[67]
. Death, physical dependence, and the propensity to cause depression of the central nervous system (CNS), especially when used in combination with opioids and sedatives, are harms identified for both gabapentinoids[42]
. The principal population at risk for addiction are those with other current or past SUD, mostly opioid and polydrug users[29],[42],[66],[67]
. Opioid users often misuse pregabalin to self-treat physical pain, to achieve a desired psychoactive effect (e.g. potentiate the effects of heroin/cocaine), and combat opioid withdrawal symptoms[42],[66],[68],[69],[70]
.
Moreover, rates of pregabalin misuse-related ambulance attendances have increased markedly over the past ten years (e.g. in Australia from 0.28 cases per 100,000 population in the first half of 2012 to 3.32 cases per 100,000 in the second half of 2017)[71]
. Therefore, pregabalin and gabapentin were found to have the potential for misuse, addiction and overdose[29],[42],[66],[67]
. In 2018, after safety warnings following an increase in deaths related to their use, the Advisory Council on the Misuse of Drugs recommended that both are controlled under the Misuse of Drugs Act 1971 as Class C substances, and scheduled under the Misuse of Drugs Regulations 2001 as Schedule 3, so as not to preclude legitimate use on prescription (see Table)[72]
.
Z-drugs
The Z-drugs (zolpidem, zaleplon, zopiclone), so-called hypnotic drugs, were introduced in the 1980s for the short-term treatment of insomnia[44]
. It was believed that they possessed a favourable and safer profile compared with benzodiazepines, because of their receptor selectivity and improved pharmacokinetic properties[73]
. Their significant hypnotic effects involve both a sleep latency reduction and a sleep quality improvement through an increased γ-aminobutyric acid (GABA) transmission at the same GABA-type A receptor as benzodiazepines.
In recent years, concern has grown for their safety because of abuse and dependence issues[9],[36]
, drug-assisted sexual assaults and dangerous sleep behaviours (e.g. sleep eating, sleep driving and sleepwalking). Problematic use of hypnotic drugs has been described in male and young recreational users of high-dose drugs. They are often abused with other licit/illicit drugs via intranasal/intravenous administration[74]
.
A second abusing population was studied, and comprised long-term users, including patients with comorbidities of mood/neurotic disorders and SUDs, and older people using Z-drug hypnotics to treat insomnia, who were then unable to cut down the dosages needed to manage withdrawal symptoms[75],[76]
. Zolpidem and zopiclone presented with the same dependence risk, but zopiclone was most indicated in being sold on the black market and in overdose adverse drug reactions[9],[77]
. Similarly to benzodiazepines, since 2013, Z-drugs have been controlled as Class C and Schedule 4 substances under the Misuse of Drugs Act and Regulations, respectively[78],[79]
.
Bupropion
Among antidepressants, the dopaminergic, stimulant-like activities of bupropion may explain its possible recreational value[4]
. It is a second-generation antidepressant acting as a selective inhibitor of catecholamine (i.e. noradrenaline and dopamine) reuptake[44]
. In the UK, it is licensed as smoking cessation treatment only[80]
. A 14-year retrospective review showed that 975 single substance bupropion cases were reported to the National Poison Data System (NPDS), with “intentional abuse” as the coded reason for exposure in individuals aged 13 and older[46]
.
The prevalence of abuse increased by 75% from 2000 to 2012, and mostly involved adolescents and young adults, who reported clinical effects of tachycardia, seizures and agitation/irritability[46]
. Its recreational use by oral/nasal/intravenous routes has been reported, with people misusing the drug to get a ‘high’ similar to that obtained through other stimulants, such as cocaine (see Table)[31],[81],[82],[83],[84]
.
Venlafaxine
Venlafaxine is an antidepressant in the serotonin-norepinephrine reuptake inhibitor class[44]
. Its recreational use is related to its reuptake inhibition, with dose-dependent effects on selective serotonin (5-HT) transmission at low doses (<150mg/day); on both 5-HT and norepinephrine systems at moderate doses (>150mg/day); and on dopamine at high doses (>300mg/day)[41]
. Large venlafaxine dosages might be consumed to produce amphetamine/ecstasy-like effects[31],[32]
. Euphoria and increased sociality, as well as dissociative effects, including distorted sense of time and “numbness”, have been described[31],[32]
. Patients with prior SUD (e.g. opioid abuse/dependence) appeared to be more vulnerable to venlafaxine misuse[41],[85]
.
Fatalities have been reported relating to numerous overdose cases, with associated symptoms of tachycardia, seizures, coma and serotonin syndrome; moreover, dependence issues following long-term use have been described[4],[41],[86]
. A retrospective review of venlafaxine exposures reported to the NPDS from 2000 to 2016 described 752 intentional-abuse venlafaxine exposures of the total of 85,621, with prevalence decreasing from 107/10,000 venlafaxine exposures in 2000 to 59.3/10,000 in 2016[87]
. The median age was 23 years and 50% were female[87]
. Primary route was ingestion (90.8%), with 4.7% using venlafaxine via inhalation/intranasal administration. The most frequent clinical effects reported were tachycardia (33.9%), drowsiness (20.7%) and agitation (11.5%)[87]
. The decrease in intentional abuse exposures in the study was explained by authors through several reasons, including underreporting or a possible decrease in the prevalence of venlafaxine abuse as patients shift to other agents, but changes in prescribing patterns for venlafaxine were excluded[87]
.
Over-the-counter drugs misuse
The potential for misuse of OTC medications that have not previously been deemed to have a diversion potential has been reported worldwide[41],[88],[89]
. Their abuse appears facilitated by their accessibility, low cost, decreased perception of the potential for harm and growing social acceptability[2],[7],[12],[15],[90]
. In contrast to prescribed and illicit drugs, medications available for individuals to purchase legally without prescription have been perceived to be relatively safe[2],[7],[12],[90]
.
They are typically purchased not only from pharmacies, but also from non-medical outlets (e.g. online illicit websites and the darknet). The internet can be used to obtain them without restrictions (e.g. prescription drugs might be obtained without a prescription)[90]
. Apart from OTC products that can be misused, such as some codeine or dextromethorphan-containing cough syrups, and decongestants (e.g. pseudoephedrine), other medicines have been found to be misused[2],[7],[12],[90]
. Alcohol and illicit drug use are highly associated with the abuse of OTC medications[2],[7]
.
Loperamide
Loperamide is a common anti-diarrhoeal drug, that binds to µ-opioid receptors in the gastrointestinal tract, decreasing peristalsis and increasing sphincter tone[41]
. At therapeutic doses (e.g. 2mg, with a maximum dosage of 16mg), loperamide does not exert cross central opioid effects; however, at high dosages (e.g. 50–800mg), it might be recreationally abused to achieve a euphoric state, which is informally referred to as “lope high”[40]
. It might be used to manage and cope with opioid withdrawal symptoms[7],[40],[91],[92]
.
Loperamide toxicity involves gastrointestinal (e.g. nausea, vomiting, constipation), CNS (e.g. respiratory depression, altered mental status, miosis) and cardiovascular effects (e.g. ventricular dysrhythmias and electrocardiogram alterations, such as prolonged QT, QRS widening and torsades de pointes), which might be fatal[41],[93],[94],[95],[96],[97],[98],[99],[100],[101]
. Consistently, loperamide exposures reported to the NPDS indicated intentional misuse and abuse. There was a 91% increase in reported exposures from 2010 to 2015, with a total of 201 and 383 exposures in 2010 and 2015, respectively, and a rate of around 38 cases per year[102]
, most of them involving single-agent loperamide abuse and cardiotoxicity[102],[103]
.
Since September 2019, the Food and Drug Administration (FDA) has limited loperamide package sizes to reduce inappropriate use[104]
. Few pharmacies currently regulate its sale, and no regulations exist to prevent purchasing at non-pharmacy online outlets[105]
. Interested pharmacies can implement policies to reduce excessive access and prevent harm. However, collateral purchasing at other retail stores or pharmacies may still occur[105]
.
Dextromethorphan
As an analogue of codeine and a semisynthetic morphine derivative, dextromethorphan is a component of many cough and cold medicines. At therapeutic doses, dextromethorphan produces minimal analgesic and antitussive effects. At high doses, acting as a N-methyl-D-aspartate receptor antagonist, it produces the hallucinogenic and dissociative effects that are recreationally sought. Neurobehavioural effects are dose-related, ranging from a mild to moderate stimulation with restlessness and euphoria (at 100–200mg doses), to a dissociated state characterised by hallucinations, paranoia, perceptual distortions, delusional beliefs, ataxia and out-of-body experiences at doses higher than 1,000mg. These experiences are referred to as ‘robo-ing’, ‘robo-copping’ or ‘robo-tripping’ (see Table)[7],[45],[48],[106],[107],[108]
.
Benzydamine
BZY acts as an analgesic and antipyretic, and is used for the topical treatment of inflammations of the oral and vaginal mucosae. BZY has been reported to be misused in several countries, including Brazil, Italy, Romania, Poland and Turkey, at high doses (i.e. 500–3,000mg) to reach stimulant effects on the CNS (e.g. euphoria, hyperreactivity, insomnia, abnormal behaviour, and psychotic symptoms, including paranoia and visual hallucinations)[109],[110],[111],[112],[113],[114],[115]
. BZY diversion issues might involve young people and the concomitant use of alcohol/cannabis[38],[39],[43]
.
Even though the molecular mechanism underlying the psychoactive and reinforcing effects of BZY is still unknown, a central cannabinoidergic mechanism of action has been hypothesised (see Table)[48],[116]
. Informal self-reports, hosted by internet drug fora and social networks, have contributed to the diffusion of BZY abuse, providing information about routes of administration, dosages and substance preparation from commercial products, as well as advice about other psychotropic substances to be used in combination with BZY to both enhance its pleasurable effects and dampen undesired ones[38],[39],[43]
.
Antihistamine drugs
Promethazine
As a histamine (H)1 receptor antagonist, promethazine is commonly used for symptomatic relief from nausea and vomiting, allergic conditions, motion sickness and the common cold. Often available with codeine in common cough suppressants, its abuse potential appears related to its calming and sedating effect, and enhancement of other coâ€ingested substances, such as benzodiazepines and opioids[34],[48],[117]
.
The abuse of promethazine mixed with a soft drink and candy, with some variants, including purple-coloured alcohol (‘purple drank’), has become popular among young people for its euphoric effects and easy accessibility[12],[28],[37]
. Despite being preferred to other substances, such as benzodiazepines, for the treatment of anxiety and sleep disorders in substance-dependent patients, promethazine has been reported to be misused among people with a SUD or an opioid dependence as a substitute for another drug (e.g. if the desired drug is unavailable or too costly) or to augment the effects of inadequate opioid dosing (i.e. to delay the onset of opioid withdrawal) (see Table)[118],[119],[120],[121]
.
Chlorphenamine
As a first generation H1-receptor antagonist, chlorphenamine is used as a cheap sleep aid or anxiolytic[13]
. Chlorphenamine has potent antimuscarinic properties, and its abuse has been related to pleasurable feelings such as euphoria, which reinforces the repetitive use of the drug and the possibility of developing drug dependence, but might also cause psychotic symptoms in predisposed individuals (e.g. people with mental illnesses or individuals concomitantly abusing other drugs)[122]
.
Together with dextromethorphan in cough and cold suppressants, or simultaneously consumed with serotoninergic drugs, it might cause significant serotonin toxicity[107],[123],[124],[125]
. A fatality has been registered involving chlorphenamine used concomitantly with an opioid[126]
. The abuse of chlorphenamine has been described by data collected from the Texas Poison Center Network Toxic Exposure Surveillance System, and its intended use or abuse appears to be increasing, particularly among young people[127]
.
Diphenhydramine
Diphenhydramine is an OTC drug acting on peripheral and central H1 receptors, causing reduction of allergic symptoms and sedation, respectively[128]
. The abuse of diphenhydramine appears related to multiple potential mechanisms of action, including a potent competitive antagonism on muscarinic receptors, causing sinus tachycardia, xerostomia, mydriasis, blurred vision, ileus, urinary retention, CNS depression, agitation, hyperactivity or psychosis[107],[128]
.
At high dosage and concomitantly assumed together with other drugs (e.g. alcohol, cannabis and stimulants), diphenhydramine can have a stimulatory effect in children and young adults, such as elevated mood, increased energy levels and mild euphoria, instead of the sedating properties seen in adults[128]
. Increased dopaminergic neurotransmission in the mesolimbic pathway is thought to cause rewarding properties and drug-seeking behaviour[107],[128]
. There are no examples of at-risk groups that are prone to this misuse.
Hyoscine butylbromide
Also known as scopolamine butylbromide, hyoscine butylbromide is a plant-derived anticholinergic agent, commonly used as an antispasmodic drug[35]
. A dose of 10mg or more is used to control intestinal and other smooth muscle spasms, for the symptomatic relief of irritable bowel syndrome and as a premedication in anaesthesia[35]
. Its use and abuse as a psychoactive substance has previously been reported among young people, who obtain it from proprietary products (e.g. Buscopan [Sanofi])[35]
.
At supratherapeutic dosages (from 1.2mg as a single dose, while the recommended dose for adults is one to two tablets of 0.3mg as a single dose), it exerts potent CNS effects, including restlessness, excitement, euphoria, disorientation, irritability and characteristic delirium-like states with auditory, visual and tactile hallucinations, altered mood, insomnia and cognitive dysfunctions[33],[35],[129]
. An advisory warning was issued in 2016 by the European Monitoring Centre for Drugs and Drug Addiction regarding 17 intoxications involving cocaine containing scopolamine, although it has not been formally notified as an NPS (see Table)[130],[131]
.
Discussion
The non-medical use of prescription drugs and OTC medications for recreational purposes is a global health concern because of the unpredictable effects of some drugs used in abnormal dosages and unlicensed administration, but also owing to the possibility of their diversion in the context of polydrug misuse[13]
. It is particularly concerning that drugs that have not been considered as being potentially abused, such as loperamide, might be diverted at high dosages, and possibly cause serious cardiotoxic effects and fatalities[102],[103]
.
Abuse of drugs during the COVID-19 pandemic
The COVID-19 outbreak has challenged public health policies owing to additional concerns relating to drug users and people with SUDs[132],[133]
. Individuals in this vulnerable category might be exposed to additional risks, such as physical problems (e.g. hepatic/renal dysfunctions, neuropathies, obesity, cardiovascular diseases), psychological comorbidities (e.g. mood and anxiety disorders, psychoses); homelessness; incarceration; economic difficulties; and other socioeconomic issues deriving from drug addiction[133],[134],[135],[136],[137],[138]
. Moreover, the COVID-19 pandemic is impacting drug markets. There have been reports of supply shortages of numerous drugs (e.g. opioids) at the street level; price increases for consumers on the black market; and reductions in purity[133],[134],[139]
. These issues, in combination with a general economic loss, can encourage shifts to more risky drug-using behaviours, such as the:
- Use of domestically produced substances;
- Use of prescription/OTC drugs;
- Mixing with cheaper drugs (such as ‘street benzos’) and synthetic cannabinoids[139]
.
Access to drug services is disrupted by quarantine, social distancing and other restrictive measures adopted to stop the spread of COVID-19[133],[134],[135],[137],[140]
. In addition, community pharmacies are being challenged by staff shortages, service disorganisation and self-isolation, meaning that the recent crisis creates an urgent requirement for expanded drug service provision, to protect vulnerable populations and minimise additional burdens on the health system[133],[137],[141]
.
Pharmacists’ role in drug abuse prevention, education and assistance
As more users turn from street drugs to prescription/OTC products, pharmacists must increase their vigilance when supplying medicines, and be aware of medicines’ potential to end up on the black market[57]
. Pharmacists have long taken responsibility for assuming an important role in substance abuse prevention and education, and they are enhancing their services during and after the pandemic to support their patients[142]
. As healthcare providers, they should participate in, or contribute to, the development of specific prevention and assistance programmes within healthcare organisations or public services[143],[144]
. They should also avoid potentially risky prescribing practices (e.g. prescribing larger quantities of pain medication than is clinically needed), and collaborate with outpatient and ambulatory care providers to prevent substance abuse following discharge.
Pharmacists should engage in open communication to provide reassurance to patients and develop a trusting relationship, especially in vulnerable populations who might be less confident in communicating diversion and misuse issues to healthcare professionals. Pharmacists might be able to help identify patients who may have problems related to substance abuse, and refer them to the appropriate service (e.g. mental or addiction services)[145],[146],[147],[148]
. Additionally, pharmacists should be involved in ensuring safe and effective medication-use systems, including the development of the pharmacotherapeutic elements of drug detoxification protocols and organisational responsibilities for medication supply, distribution and control[145]
.
Implication for practice
Pharmacists can prevent and control drug diversion behaviours, thereby reducing the negative impacts of their misuse by:
- Giving clear information about the effects medications may have, providing advice about any possible drug interactions;
- Making drug records that might prevent consultations with multiple doctors and subsequent duplicate prescriptions (‘doctor shopping’) for a drug with misuse potential.
It is vital that pharmacists ensure the continuity of care for people who use drugs and people with drug use disorders by facilitating access to community maintenance programmes (e.g. provision of methadone or buprenorphine to opioid users)[149],[150]
. Harm-avoiding interventions could be adopted, including guidance for facilitating controlled substance prescribing[132],[137],[151]
. Telehealth, for monitoring drug-dependent patients while providing access to virtual support groups through online meetings during the pandemic, could also be put in place[132],[141],[152]
.
In the context of a trusted pharmacist–patient relationship, pharmacists should inform at-risk individuals of drug dosages and drug interactions, and counsel them on harmful combinations among medications, as well as interactions between medications and alcohol or other illicit substances[153]
. The use of drug combinations, including several CNS-depressants (e.g. benzodiazepines, opioids, gabapentinoids), together with OTC products, alcohol or other illicit substances should be discouraged[18],[154],[155]
.
Finally, clinicians and pharmacists should be aware of potential pressures from patients to prescribe more drugs than needed; of excessive sales of prescription/OTC products, which might be diverted and abused; and of the risk of eventual aggression towards pharmacy staff[156]
. Developing multidisciplinary support platforms, including both health and social support, could help reduce mental distress owing to misinformation among users, as could teaching problem-solving strategies to cope with drug abuse (e.g. the management of stress to prevent relapses during the pandemic)[157]
. Telemental health might provide users with prevention interventions, through telepsychiatry, digital platforms, dedicated hotlines and mental health apps[158],[159],[160]
.
Conclusion
The abuse of prescription and OTC drugs has become of increasing public concern across the globe. The current drug scenarios are greatly challenging healthcare providers and pharmacists, particularly during the COVID-19 pandemic. These healthcare professionals are recommended to be vigilant and develop strategies to ensure continuity of care for people who use drugs and people with drug use disorders, and prevent possible medicines misuse and diversion.
Author details
Stefania Chiappini is an MD, psychiatrist and a PhD student; Amira Guirguis is a PhD, MPharm; John Martin Corkery is a BA Hons, MSc; and Fabrizio Schifano is an MD, psychiatrist, and chair in clinical pharmacology and therapeutics. All work within the Psychopharmacology, Drug Misuse and Novel Psychoactive Substances Research Unit at the School of Life and Medical Sciences, University of Hertfordshire, UK. Amira Guirguis is also a senior lecturer and MPharm programme director at Swansea University Medical School, Institute of Life Sciences.
Corresponding author: Stefania Chiappini, stefaniachiappini9@gmail.com
Financial disclosure and conflict of interest statement
Fabrizio Schifano was a member of the UK Advisory Council on the Misuse of Drugs (ACMD) from 2011 to 2019; he is currently an EMA Advisory Board (psychiatry) member. John Martin Corkery is a member of the ACMD’s Novel Psychoactive Substances and Technical Committees. The authors have no other relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript.
References
[1] Graddy R, Buresh ME & Rastegar DA. New and emerging illicit psychoactive substances. Med Clin North Am 2018;102(4):697–714. doi: 10.1016/j.mcna.2018.02.010
[2] Hughes GF, McElnay JC, Hughes CM & McKenna P. Abuse/misuse of non-prescription drugs. Pharm World Sci 1999;21(6):251–255. doi: 10.1023/a:1008788726842
[3] Schifano F. Recent changes in drug abuse scenarios: the new/novel psychoactive substances (NPS) phenomenon. Brain Sci 2018;13;8(12)pii:E221. doi: 10.3390/brainsci8120221
[4] Schifano F, Chiappini S, Corkery JM & Guirguis A. Abuse of prescription drugs in the context of novel psychoactive substances (NPS): a systematic review. Brain Sci 2018;22;8(4)pii:E73. doi: 10.3390/brainsci8040073
[5] Chiappini S & Schifano F. What about “pharming”? Issues regarding the misuse of prescription and over-the-counter drugs. Brain Sci 2020;10,736. doi: 10.3390/brainsci10100736
[6] Lessenger JE & Feinberg SD. Abuse of prescription and over-the-counter medications. J Am Board Fam Med 2008;21:45–54. doi: 10.3122/jabfm.2008.01.070071
[7] Levine DA. “Pharming”: the abuse of prescription and over-the-counter drugs in teens. Curr Opin Pediatr 2007;19(3):270–274. doi: 10.1097/MOP.0b013e32814b09cf
[8] Wood D. Drug diversion. Aust Prescr 2015;38:164–166. doi: 10.18773/austprescr.2015.058
[9] Schifano F, Napoletano F, Chiappini S et al. New emerging psychoactive substances and associated psychopathological consequences. Psychol Med 2019;22:1–13. doi: 10.1017/S0033291719001727
[10] McCabe SE, Veliz PT, Dickinson K et al. Trajectories of prescription drug misuse during the transition from late adolescence into adulthood in the USA: a national longitudinal multicohort study. Lancet Psychiatry 2019;6(10):840–850. doi: 10.1016/S2215-0366(19)30299-8
[11] Scherbaum N, Schifano F & Bonnet U. New psychoactive substances (NPS): a challenge for the addiction treatment services. Pharmacopsychiatry 2017;50(3):116–122. doi: 10.1055/s-0043-102059
[12] Burns JM & Boyer EW. Antitussives and substance abuse. Subst Abuse Rehabil 2013;4:75–82. doi: 10.2147/SAR.S36761
[13] Cooper RJ. Over-the-counter medicine abuse: a review of the literature. J Subst Use 2013;18(2):82–107. doi: 10.3109/14659891.2011.615002
[14] Jouanjus E, Falcou A, Deheul S et al. Detecting the diverted use of psychoactive drugs by adolescents and young adults: a pilot study. Pharmacoepidemiol Drug Saf 2018;27:1286–1292. doi: 10.1002/pds.4624
[15] McCarthy M. Prescription drug abuse up sharply in the USA. Lancet 2007;369:1505–1506. doi: 10.1016/S0140-6736(07)60690-4
[16] Advisory Council on the Misuse of Drugs. Diversion and illicit supply of medicines. 2016. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/580296/Meds_report-_final_report_15_December_LU__2_.pdf (accessed November 2020)
[17] United Nations Office on Drugs and Crime. The non-medical use of prescription drugs. Policy direction issues. 2011. Available at: http://www.unodc.org/docs/youthnet/Final_Prescription_Drugs_Paper.pdf (accessed November 2020)
[18] United Nations Office on Drugs and Crime. World drug report 2019. 2019. Available at: https://wdr.unodc.org/wdr2019/ (accessed November 2020)
[19] National Institute on Drug Abuse. Drug misuse and addiction. 2020. Available at: https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/drug-misuse-addiction (accessed November 2020)
[20] Arillotta D, Schifano F, Napoletano F et al. Novel opioids: systematic web crawling within the e-psychonauts’ scenario. Front Neurosci 2020;18;14:149. doi: 10.3389/fnins.2020.00149
[21] Orsolini L, Corkery JM, Chiappini S et al. New/designer benzodiazepines: an analysis of the literature and psychonauts’ trip reports. Curr Neuropharmacol 2020;18(9)809–837. doi: 10.2174/1570159X18666200110121333
[22] Corazza O & Roman-Urrestarazu A. Handbook of Novel Psychoactive Substances: What Clinicians Should Know about NPS. New York: Routledge; 2018.
[23] Wilens TE & Kaminski TA. Prescription stimulants: from cognitive enhancement to misuse. Pediatr Clin North Am 2019;66(6):1109–1120. doi: 10.1016/j.pcl.2019.08.006
[24] Corazza O, Bersani FS, Brunoro R et al. The diffusion of performance and image-enhancing drugs (PIEDs) on the internet: the abuse of the cognitive enhancer piracetam. Subst Use Misuse 2014;49(14):1849–1856. doi: 10.3109/10826084.2014.912232
[25] Medical Dictionary for Regulatory Activities (MedDRA) Version 21. 2018. Available at: https://www.meddra.org/sites/default/files/guidance/file/smq_intguide_21_0_english.pdf (accessed November 2020)
[26] American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition (DSM-IV). Washington DC: American Psychiatric Association; 1994.
[27] American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Fifth Edition (DSM-5). Washington DC: American Psychiatric Association; 2013.
[28] Agnich LE, Stogner JM, Miller BL & Marcum CD. Purple drank prevalence and characteristics of misusers of codeine cough syrup mixtures. Addict Behav 2013;38(9):2445–2449. doi: 10.1016/j.addbeh.2013.03.020
[29] Bonnet U & Scherbaum N. How addictive are gabapentin and pregabalin? A systematic review. Eur Neuropsychopharmacol 2017;27(12):1185–1215. doi: 10.1016/j.euroneuro.2017.08.430
[30] Chiappini S & Schifano F. Is there a potential of misuse for quetiapine? Literature review and analysis of the European Medicines Agency/European Medicines Agency adverse drug reactions database. J Clin Psychopharmacol 2018;38(1):72–79. doi: 10.1097/JCP.0000000000000814
[31] Evans EA & Sullivan MA. Abuse and misuse of antidepressants. Subst Abuse Rehabil 2014;5:107–120. doi: 10.2147/SAR.S37917
[32] Francesconi G, Orsolini L, Papanti D et al. Venlafaxine as the ‘baby ecstasy’? Literature overview and analysis of web-based misusers’ experiences. Hum Psychopharmacol 2015;30: 255–261. doi: 10.1002/hup.2476
[33] Jalali F, Afshari R & Babaei A. Smoking crushed hyoscine/scopolamine tablets as drug abuse. Subst Use Misuse 2014;49(7):793–797. doi: 10.3109/10826084.2014.880178
[34] Jensen LL, Rømsing J & Dalhoff K. A Danish survey of antihistamine use and poisoning patterns. Basic Clin Pharmacol 2017;120:64–70. doi: 10.1111/bcpt.12632
[35] Kummer S, Rickert A, Daldrup T & Mayatepek E. Abuse of the over-the-counter antispasmodic butylscopolamine for the home synthesis of psychoactive scopolamine. Eur J Pediatr 2016;175(7):1019–1021. doi: 10.1007/s00431-015-2683-5
[36] Lähteenmäki R, Neuvonen PJ, Puustinen J et al. Withdrawal from long-term use of zopiclone, zolpidem and temazepam may improve perceived sleep and quality of life in older adults with primary insomnia. Basic Clin Pharmacol Toxicol 2019;124(3):330–340. doi: 10.1111/bcpt.13144
[37] Miuli A, Stigliano G, Lalli A et al. “Purple drank” (codeine and promethazine cough syrup): a systematic review of a social phenomenon with medical implications. J Psychoactive Drugs 2020;1–10. doi: 10.1080/02791072.2020.1797250
[38] Opaleye ES, Noto AR, Sanchez Zv et al. Recreational use of benzydamine as a hallucinogen among street youth in Brazil. Braz J Psychiatry 2009;31(3):208–213. doi: 10.1590/s1516-44462009000300005
[39] Opaleye ES, Sanchez ZM, Moura YG et al. An anti-inflammatory as a recreational drug in Brazil. Addiction 2011;106(1):225. doi: 10.1111/j.1360-0443.2010.03196.x
[40] Reeves RR, Ladner ME, Perry CL et al. Abuse of medications that theoretically are without abuse potential. South Med J 2015;108(3):151–157. doi: 10.14423/SMJ.0000000000000256
[41] Schifano F & Chiappini S. Is there such a thing as a ‘lope’ dope? Analysis of loperamide-related European Medicines Agency (EMA) pharmacovigilance database reports. PLoS One 2018;13(10):e0204443. doi: 10.1371/journal.pone.0204443
[42] Schifano F & Chiappini S. Pregabalin: a range of misuseâ€related unanswered questions. CNS Neurosci Ther 2019;25:659–660. doi: 10.1111/cns.13115
[43] Schifano F, Corazza O, Marchi A et al. Analysis of online reports on the potential misuse of benzidamine. Riv Psichiatr 2013;48(3):182–186. doi: 10.1708/1292.14286
[44] Stahl SM & Grady MM. Stahl’s Essential Psychopharmacology: Prescriber’s Guide. Cambridge: Cambridge University Press; 2017.
[45] Stanciu CN, Penders TM & Rouse EM. Recreational use of dextromethorphan, “robotripping”: a brief review. Am J Addict 2016;25(5):374–377. doi: 10.1111/ajad.12389
[46] Stassinos GL & Klein-Schwartz W. Bupropion “abuse” reported to US poison centers. J Addict Med 2016;10(5):357–362. doi: 10.1097/ADM.0000000000000249
[47] Vento AE, Kotzalidis GD, Cacciotti M et al. Quetiapine abuse fourteen years later: where are we now? A systematic review. Subst Use Misuse 2020;55(2):304–313. doi: 10.1080/10826084.2019.1668013
[48] Zaprutko T, Koligat D, Michalak M et al. Misuse of OTC drugs in Poland. Health Policy 2016;120(8):875–881. doi: 10.1016/j.healthpol.2016.06.008
[49] Hernandez SH & Nelson LS. Prescription drug abuse: insight into the epidemic. Clin Pharmacol Ther 2010;88(3):307–317. doi: 10.1038/clpt.2010.154
[50] Lipari RN, Williams M & Van Horn SL. Why do adults misuse prescription drugs? In: The CBHSQ report. Rockville (MD): substance abuse and mental health services administration (US). 2017. PMID: 28968046
[51] McCabe SE, Cranford JA & West BT. Trends in prescription drug abuse and dependence, co-occurrence with other substance use disorders, and treatment utilization: results from two national surveys. Addict Behav 2008;33(10):1297–1305. doi: 10.1016/j.addbeh.2008.06.005
[52] Fortuna RJ, Robbins BW, Caiola E et al. Prescribing of controlled medications to adolescents and young adults in the United States. Pediatrics 2010;126(6):1108–1116. doi: 10.1542/peds.2010-0791
[53] Kelly BC, Wells BE, Leclair A et al. Prescription drug misuse among young adults: looking across youth cultures. Drug Alcohol Rev 2013;32(3):288–294. doi: 10.1111/dar.12016
[54] D’Souza RS & Eldrige JS. Prescription drug monitoring program. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2020.
[55] Jouanjus E, Guernec G, Lapeyreâ€Mestre M & the French Addictovigilance Network. Medical prescriptions falsified by the patients: a 12â€year national monitoring to assess prescription drug diversion. Fundam Clin Pharmacol 2018;32(3):306–322. doi: 10.1111/fcp.12356
[56] Soussan C, Andersson M & Kjellgren A. The diverse reasons for using novel psychoactive substances: a qualitative study of the users’ own perspectives. Int J Drug Policy 2018;52:71–78. doi: 10.1016/j.drugpo.2017.11.003
[57] Sukkar E & Osborne K. Pharmacists can help prevent misuse of prescription drugs by young people. Pharm J 2017;298:7902. doi: 10.1211/PJ.2017.20202998
[58] Evoy KE, Teng C, Encarnacion VG et al. Comparison of quetiapine abuse and misuse reports to the FDA adverse event reporting system with other second-generation antipsychotics. Subst Abuse 2019;13:1178221819844205. doi: 10.1177/1178221819844205
[59] Klein L, Bangh S & Cole JB. Intentional recreational abuse of quetiapine compared to other second-generation antipsychotics. West J Emerg Med 2017;18(2):243–250. doi: 10.5811/westjem.2016.10.32322
[60] Mattson ME, Albright VA, Yoon J & Council CL. Emergency department visits involving misuse and abuse of the antipsychotic quetiapine: results from the Drug Abuse Warning Network (DAWN). Subst Abuse 2015;9:39–46. doi: 10.4137/SART.S22233
[61] Heilbronn C, Lloyd B, McElwee P et al. Trends in quetiapine use and non-fatal quetiapine-related ambulance attendances. Drug Alcohol Rev 2013;32(4):405–411. doi: 10.1111/dar.12028
[62] Kim S, Lee G, Kim E et al. Quetiapine misuse and abuse: is it an atypical paradigm of drug seeking behavior? J Res Pharm Pract 2017;6(1):12–15. doi: 10.4103/2279-042X.200987
[63] Reeves RR & Brister JC. Additional evidence of the abuse potential of quetiapine. South Med J 2007;100(8):834–836. doi: 10.1097/SMJ.0b013e3180f62d53
[64] Electronic medicines compendium. Gabapentin. 2020. Available at: https://www.medicines.org.uk/emc/product/2362/smpc (accessed November 2020)
[65] Electronic medicines compendium. Pregabalin. 2020. Available at: https://www.medicines.org.uk/emc/product/1761/smpc (accessed November 2020)
[66] Chiappini S & Schifano F. A decade of gabapentinoid misuse: an analysis of the European Medicines Agency’s ‘suspected adverse drug reactions’ database. CNS Drugs 2016;30(7):647–654. doi: 10.1007/s40263-016-0359-y
[67] Schifano F. Misuse and abuse of pregabalin and gabapentin: cause for concern? CNS Drugs 2014;28(6):491–496. doi: 10.1007/s40263-014-0164-4
[68] Al-Husseini A, Wazaify M & Van Hout MC. Pregabalin misuse and abuse in Jordan: a qualitative study of user experiences. Int J Ment Health Addict 2018;16(3):642–654. doi: 10.1007/s11469-017-9813-4
[69] Baird CR, Fox P & Colvin LA. Gabapentinoid abuse in order to potentiate the effect of methadone: a survey among substance misusers. Eur Addict Res 2014;20(3):115–118. doi: 10.1159/000355268
[70] Buttram ME & Kurtz SP. Preliminary evidence of pregabalin misuse among prescription and/or illicit opioid (mis)users. J Psychoactive Drugs 2020;52(2):172–175. doi: 10.1080/02791072.2020.1734695
[71] Crossin R, Scott D, Arunogiri S et al. Pregabalin misuse-related ambulance attendances in Victoria, 2012–2017: characteristics of patients and attendances. Med J Aust 2019;210(2):75–79. doi: 10.5694/mja2.12036
[72] Advisory Council on the Misuse of Drugs. Addendum to advice on the anticonvulsant drugs pregabalin and gabapentin. 2018. Available at: https://www.gov.uk/government/publications/advice-on-the-anticonvulsant-drugs-pregabalin-and-gabapentin/addendum-to-advice-on-the-anticonvulsant-drugs-pregabalin-and-gabapentin-october-2018 (accessed November 2020)
[73] Gunja N. The clinical and forensic toxicology of Z-drugs. J Med Toxicol 2013;9(2):155–162. doi: 10.1007/s13181-013-0292-0
[74] Hockenhull J, Black JC, Haynes CM et al. Nonmedical use of benzodiazepines and Z-drugs in the UK. Br J Clin Pharmacol 2020. doi: 10.1111/bcp.14397
[75] Griffiths RR & Johnson MW. Relative abuse liability of hypnotic drugs: a conceptual framework and algorithm for differentiating among compounds. J Clin Psychiatry 2005;66 Suppl 9:31–41. PMID: 16336040
[76] Rousselet M, Feuillet F, Gerardin M et al. The French addictovigilance network clinical assessment: Z-drugs, true false twins. Expert Opin Drug Saf 2017;16(9):1063–1069. doi: 10.1080/14740338.2017.1346084
[77] Jaffe JH, Bloor R, Crome I et al. A postmarketing study of relative abuse liability of hypnotic sedative drugs. Addiction 2004;99:165–173. doi: 10.1111/j.1360-0443.2003.00631.x
[78] Advisory Council on the Misuse of Drugs. Advice on the control of Z-drugs (zaleplon, zolpidem and zopiclone). 2013. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/237037/ACMD_advice_Z_drugs.pdf (accessed November 2020)
[79] Marsden J, White M, Annand F et al. Medicines associated with dependence or withdrawal: a mixed-methods public health review and national database study in England. Lancet Psychiatry 2019;6(11):935–950. doi: 10.1016/S2215-0366(19)30331-1
[80] Electronic medicines compendium. Zyban 150mg prolonged release tablets. 2019. Available at: https://www.medicines.org.uk/emc/medicine/2948/ (accessed November 2020)
[81] Hu LY, Lu T & Chen YT. Have we underestimated the possibility of bupropion sustained-release addiction? Aust N Z J Psychiatry 2016;50,925–926. doi: 10.1177/0004867416632928
[82] McCormick J. Recreational bupropion abuse in a teenager. Br J Clin Pharmacol 2002;53(2):214. doi: 10.1046/j.0306-5251.2001.01538.x
[83] Reeves RR & Ladner ME. Additional evidence of the abuse potential of bupropion. J Clin Pyschopharmacol 2013;33,584–585. doi: 10.1097/JCP.0b013e318295fe2f
[84] Stall N, Godwin J& Juurlink D. Bupropion abuse and overdose. CMAJ 2014;186(13):1015. doi: 10.1503/cmaj.131534
[85] Namdari B. Venlafaxine abuse in a patient with schizophrenia and prior history of substance dependence: a case report. J Addict Dis 2013;32(4):393–395. doi: 10.1080/10550887.2013.849974
[86] Bosse GM, Spiller HA & Collins AM. A fatal case of venlafaxine overdose. J Med Toxicol 2008;4(1):18–20. doi: 10.1007/BF03160945
[87] Leonard JB & Klein-Schwartz W. Characterization of intentional-abuse venlafaxine exposures reported to poison control centers in the United States. Am J Drug Alcohol Abuse 2019;45(4):421–426. doi: 10.1080/00952990.2019.1599382
[88] Benotsch EG, Koester S, Martin AM et al. Intentional misuse of over-the-counter medications, mental health, and polysubstance use in young adults. J Community Health 2014;39(4):688–695. doi: 10.1007/s10900-013-9811-9
[89] Le VT, Norris Turner A, McDaniel A et al. Nonmedical use of over-the-counter medications is significantly associated with nonmedical use of prescription drugs among university students. J Am Coll Health 2018;66(1):1–8. doi: 10.1080/07448481.2017.1356312
[90] Cooper RJ. ‘I can’t be an addict. I am.’ Over-the-counter medicine abuse: a qualitative study. BMJ Open 2013;3(6):e002913. doi: 10.1136/bmjopen-2013-002913
[91] MacDonald R, Heiner J, Villarreal J & Strote J. Loperamide dependence and abuse. BMJ Case Rep 2015;2015:bcr2015209705. doi: 10.1136/bcr-2015-209705
[92] Powell JW & Presnell SE. Loperamide as a potential drug of abuse and misuse: fatal overdoses at the Medical University of South Carolina. J Forensic Sci 2019;64(6):1726–1730. doi: 10.1111/1556-4029.14115
[93] Ali M, Mujahid A, Bulathsinghala CP & Surani S. Cardiac arrhythmia secondary to loperamide abuse and toxicity. Cureus 2020;12(2):e6936. doi: 10.7759/cureus.6936
[94] Antoniou T & Juurlink DN. Loperamide abuse. CMAJ 2017;189(23):E803. doi: 10.1503/cmaj.161421
[95] Atoot A, Sholem S, Khaddash I & Zuberi J. Transient brugada pattern induced by loperamide abuse. Cureus 2020;12(5):e8037. doi: 10.7759/cureus.8037
[96] Katz KD, Cannon RD, Cook MD et al. Loperamide-induced torsades de pointes: a case series. J Emerg Med 2017;53(3):339–344. doi: 10.1016/j.jemermed.2017.04.027
[97] Marraffa JM, Holland MG, Sullivan RW et al. Cardiac conduction disturbance after loperamide abuse. Clin Toxicol (Phila) 2014;52(9):952–957. doi: 10.3109/15563650.2014.969371
[98] Nattel S. An emerging malignant arrhythmia epidemic due to loperamide abuse: underlying mechanisms and clinical relevance. JACC Clin Electrophysiol 2016;2(7):790–792. doi: 10.1016/j.jacep.2016.10.009
[99] Rasla S, Parikh P, Hoffmeister P et al. Unexpected serious cardiac arrhythmias in the setting of loperamide abuse. R I Med J (2013). 2017;100(4):33–36. PMID: 28375418
[100] Stefek B, Wolfe LT & Cohen M. Brugada syndrome associated with adolescent loperamide abuse. Pediatrics 2018;142(4):e20181423. doi: 10.1542/peds.2018-1423
[101] Wightman RS, Hoffman RS, Howland MA et al. Not your regular high: cardiac dysrhythmias caused by loperamide. Clin Toxicol (Phila) 2016;54(5):454–458. doi: 10.3109/15563650.2016.1159310
[102] Vakkalanka JP, Charlton NP & Holstege CP. Epidemiologic trends in loperamide abuse and misuse. Ann Emerg Med 2017;69(1):73–78. doi: 10.1016/j.annemergmed.2016.08.444
[103] Eggleston W, Marraffa JM, Stork CM et al. Notes from the field: cardiac dysrhythmias after loperamide abuse — New York, 2008–2016. MMWR Morb Mortal Wkly Rep 2016;65(45):1276–1277. doi: 10.15585/mmwr.mm6545a7
[104] Food and Drug Administration. FDA limits packaging for anti-diarrhea medicine loperamide (Imodium) to encourage safe use. 2019. Available at: https://www.fda.gov/drugs/drug-safety-and-availability/fda-limits-packaging-anti-diarrhea-medicine-loperamide-imodium-encourage-safe-use (accessed November 2020)
[105] Feldman R & Everton E. National assessment of pharmacist awareness of loperamide abuse and ability to restrict sale if abuse is suspected. J Am Pharm Assoc. 2020;S1544–3191(20)30264-8. doi: 10.1016/j.japh.2020.05.021
[106] Martinak B, Bolis RA, Black JR et al. Dextromethorphan in cough syrup: the poor man’s psychosis. Psychopharmacol Bull 2017;47(4):59–63. PMID: 28936010
[107] Sansgiry SS, Bhansali AH, Bapat SS & Xu Q. Abuse of over-the-counter medicines: a pharmacist’s perspective. Integr Pharm Res Pract. 2017;6:1–6. doi: 10.2147/IPRP.S103494
[108] Schwartz RH. Adolescent abuse of dextromethorphan. Clin Pediatr (Phila) 2005;44(7):565–568. doi: 10.1177/000992280504400702
[109] Acar YA, Kalkan M, Cetin R et al. Acute psychotic symptoms due to benzydamine hydrochloride abuse with alcohol. Case Rep Psychiatry 2014;290365. doi: 10.1155/2014/290365
[110] Anand JS, Lukasik-GlÄ™bocka M & Korolkiewicz RP. Recreational abuse with benzydamine hydrochloride (tantum rosa). Clin Toxicol 2007;45(2):198–199. doi: 10.1080/15563650600981210
[111] Ballesteros S, Ramón MF & MartÃnez-Arrieta R. Ingestions of benzydamine-containing vaginal preparations. Clin Toxicol (Phila) 2009;47(2):145–149. doi: 10.1080/15563650801938670
[112] Can B, Oz I, Ozer H & Simsek T. Hallucinations after ingesting a high dose of benzydamine hydrochloride. Clin Psychopharmacol Neurosci 2016;14(4):407–408. doi: 10.9758/cpn.2016.14.4.407
[113] DoÄŸan M, Yılmaz C, Çaksen H & Güven AS. A case of benzydamine HCL intoxication. East J Med 2006;11(1):26–28. Available at: https://eastjmed.org/jvi.aspx?pdir=ejm&plng=eng&un=EJM-65807&look4= (accessed November 2020)
[114] Gürü M, Åžafak Y, Cengiz GF & Kuru E, Örsel S. Chronic psychosis related to benzydamine hydrochloride abuse. Neurocase 2019;25(3–4):156–158. doi: 10.1080/13554794.2019.1617318
[115] Rotolo MC, Pellegrini M, Solimini R et al. ‘Smart drugs’, the new drugs on the web: two cases of acute intoxication. Biochim Clin 2014;38(3):268–271. Available at: https://www.researchgate.net/publication/281928450_Smart_drugs_the_new_drugs_on_the_web_Two_cases_of_acute_intoxication (accessed November 2020)
[116] Avvisati R, Meringolo M, Stendardo E et al. Intravenous self-administration of benzydamine, a non-steroidal anti-inflammatory drug with a central cannabinoidergic mechanism of action. Addict Biol 2018;23(2):610–619. doi: 10.1111/adb.12516
[117] Tsay ME, Procopio G, Anderson BD & Klein-Schwartz W. Abuse and intentional misuse of promethazine reported to US poison centers: 2002 to 2012. J Addict Med 2015;9(3):233–237. doi: 10.1097/ADM.0000000000000124
[118] Chiappini S, Corkery JM, Schifano F & Guirguis A. Beyond the purple drank. Study of promethazine abuse according to the European Medicines Agency (EMA) adverse drug reactions (ADR) reports. J Psychopharmacol 2020; In press.
[119] Clatts M, Giang Le M, Goldsamt L & Colón-López V. Nonmedical use of promethazine hydrochloride among heroin injectors in Vietnam: unrecognized risks and unintended consequences. Subst Use Misuse 2010;45(4):515–527. doi: 10.3109/10826080903452520
[120] Lynch KL, Shapiro BJ, Coffa D et al. Promethazine use among chronic pain patients. Drug Alcohol Depend 2015;150:92–97. doi: 10.1016/j.drugalcdep.2015.02.023
[121] Shapiro BJ, Lynch KL, Toochinda T et al. Promethazine misuse among methadone maintenance patients and community-based injection drug users. J Addict Med 2013;7(2):96–101. doi: 10.1097/ADM.0b013e31827f9b43
[122] Banerji S & Anderson IB. Abuse of coricidin HBP cough & cold tablets: episodes recorded by a poison center. Am J Health Syst Pharm 2001;58(19):1811–1814. doi: 10.1093/ajhp/58.19.1811
[123] Dickerson DL, Schaepper MA, Peterson MD & Ashworth MD. Coricidin HBP abuse: patient characteristics and psychiatric manifestations as recorded in an inpatient psychiatric unit. J Addict Dis 2008;27(1):25–32. doi: 10.1300/J069v27n01_03
[124] Kirages TJ, Sulé HP & Mycyk MB. Severe manifestations of coricidin intoxication. Am J Emerg Med 2003;21(6):473–475. doi: 10.1016/s0735-6757(03)00168-2
[125] Monte AA, Chuang R & Bodme M. Dextromethorphan, chlorphenamine and serotonin toxicity: case report and systematic literature review. Br J Clin Pharmacol 2010;70:6:794–798. doi: 10.1111/j.1365-2125.2010.03747.x
[126] Kinoshita H, Tanaka N, Jamal M et al. A fatal case due to cough syrup abuse. Soud Lek 2012;57(4):69–70. PMID: 23121038
[127] Baker SD & Borys DJ. A possible trend suggesting increased abuse from coricidin exposures reported to the Texas Poison Network: comparing 1998 to 1999. Vet Hum Toxicol 2002;44(3):169–171. PMID: 12046973
[128] Saran JS, Barbano RL, Schult R et al. Chronic diphenhydramine abuse and withdrawal. A diagnostic challenge. Neurol Clin Pract 2017;7(5):439–441. doi: 10.1212/CPJ.0000000000000304
[129] Cheng SW, Hu WH, Hung DZ & Yang DY. Anticholinergic poisoning from a large dose of Scopolia extract. Vet Hum Toxicol 2002;44(4):222–223. PMID: 12136971
[130] Ham S, Tae KK, Kim K et al. Drug abuse and psychosis: new insights into drug-induced psychosis. Exp Neurobiol 2017;26(1):11–24. doi: 10.5607/en.2017.26.1.11
[131] Lakstygal AM, Kolesnikova TO, Khatsko SL et al. DARK classics in chemical neuroscience: atropine, scopolamine, and other anticholinergic deliriant hallucinogens. ACS Chem Neurosci 2019;10(5):2144–2159. doi: 10.1021/acschemneuro.8b00615
[132] Enforcement Administration. COVID-19 information page. 2020. Available at: www.deadiversion.usdoj.gov/coronavirus.html (accessed November 2020)
[133] European Monitoring Centre for Drug and Drug Addiction. The implications of COVID-19 for people who use drugs (PWUD) and drug service providers. 2020. Available at: http://www.emcdda.europa.eu/publications/topic-overviews/covid-19-and-people-who-use-drugs_en (accessed November 2020)
[134] Chiappini S, Guirguis A, John A et al. COVID-19: the hidden impact on mental health and drug addiction. Front Psychiatry 2020;11:767. doi: 10.3389/fpsyt.2020.00767
[135] Department of Health and Social Care and Public Health England. COVID-19: guidance for commissioners and providers of services for people who use drugs or alcohol. 2020. Available at: https://www.gov.uk/government/publications/covid-19-guidance-for-commissioners-and-providers-of-services-for-people-who-use-drugs-or-alcohol/covid-19-guidance-for-commissioners-and-providers-of-services-for-people-who-use-drugs-or-alcohol (accessed November 2020)
[136] Pfefferbaum B & North CS. Mental health and the covid-19 pandemic. NEJM 2020;383(6):510–512. doi: 10.1056/NEJMp2008017
[137] Volkow ND. Collision of the COVID-19 and addiction epidemics. Ann Intern Med 2020. doi: 10.7326/M20-1212
[138] Zhu S, Wu Y, Zhu CY et al. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain Behav Immun 2020;pii:S0889–1591(20)30601-2. doi: 10.1016/j.bbi.2020.04.045
[139] United Nations. COVID-19 causes some illegal drug prices to surge, as supplies are disrupted worldwide. 2020. Available at: https://news.un.org/en/story/2020/05/1063512 (accessed November 2020)
[140] Volkow ND. Coping with the collision of public health crises: COVID-19 and substance use disorders. 2020. Available at: https://directorsblog.nih.gov/2020/04/21/coping-with-the-collision-of-public-health-crises-covid-19-and-substance-use-disorders/ (accessed November 2020)
[141] Green TC, Bratberg J & Finnell DS. Opioid use disorder and the COVID 19 pandemic: a call to sustain regulatory easements and further expand access to treatment. Subst Abus 2020;41(2):147–149. doi: 10.1080/08897077.2020.1752351
[142] Hogue MD, Hogue HB, Lander RD et al. The nontraditional role of pharmacists after Hurricane Katrina: process description and lessons learned. Public Health Rep 2009;124(2):217–223. doi: 10.1177/003335490912400209
[143] Substance Abuse and Mental Health Services Administration. COVID-19 and opioid treatment programs. 2020. https://www.samhsa.gov/sites/default/files/sample-otp-covid-19-faqs.pdf (accessed November 2020)
[144] Wazaify M, Hughes CM & McElnay JC. The implementation of a harm minimisation model for the identification and treatment of over-the-counter drug misuse and abuse in community pharmacies in Northern Ireland. Patient Educ Couns 2006;64(1–3):136–141. doi: 10.1016/j.pec.2005.12.008
[145] American Society of Health-System Pharmacists. ASHP statement on the pharmacist’s role in substance abuse prevention, education, and assistance. Am J Health-Syst Pharm 2016;73:e267–270. doi: 10.2146/sp140002
[146] Cooper RJ. Surveillance and uncertainty: community pharmacy responses to over the counter medicine abuse. Health Soc Care Community 2013;21(3):254–262. doi: 10.1111/hsc.12012
[147] Sheridan J, Manning V, Ridge G et al. Community pharmacies and the provision of opioid substitution services for drug misusers: changes in activity and attitudes of community pharmacists across England 1995–2005. Addiction 2007;102(11):1824–1830. doi: 10.1111/j.1360-0443.2007.02016.x
[148] Wagner AG & Guerra de Andrade A. Pharmacist professionals in the prevention of drug abuse: updating roles, and opportunities. Brazil J Pharmac Sciences 2010;46(1). doi: 10.1590/S1984-82502010000100003
[149] Becker WC & Fiellin DA. When epidemics collide: coronavirus disease 2019 (COVID-19) and the opioid crisis. Ann Intern Med 2020. doi: 10.7326/M20-1210
[150] Simeone R. Doctor shopping behavior and the diversion of prescription opioids. Subst Abuse 2017;11. doi: 10.1177/1178221817696077
[151] Levander XA & Wakeman SE. Covid-19 will worsen the opioid overdose crisis is we don’t prepare now. STAT. 2020. Available at: https://www.statnews.com/2020/03/17/covid-19-will-worsen- the-opioid-overdose-crisis-if-we-dont-prepare-now/ (accessed November 2020)
[152] World Health Organization. Alcohol and COVID-19: what you need to know. 2020. Available at: http://www.euro.who.int/__data/assets/pdf_file/0010/437608/Alcohol-and-COVID-19-what-you-need-to-know.pdf (accessed November 2020)
[153] Spoth R, Trudeau L, Shin C & Redmond C. Long-term effects of universal preventive interventions on prescription drug misuse. Addiction 2008;103(7):1160–1168. doi: 10.1111/j.1360-0443.2008.02160.x
[154] Chary M, Yi D & Manini AF. Candyflipping and other combinations: identifying drug–drug combinations from an online forum. Front Psychiatry 2018;9:135. doi: 10.3389/fpsyt.2018.00135
[155] Clinical Guidelines on Drug Misuse and Dependence Update 2017 Independent Expert Working Group. Drug misuse and dependence: UK guidelines on clinical management. Department of Health. 2017. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/673978/clinical_guidelines_2017.pdf (accessed November 2020)
[156] Crowley DM, Jones DE, Coffman DL & Greenberg MT. Can we build an efficient response to the prescription drug abuse epidemic? Assessing the cost effectiveness of universal prevention in the PROSPER trial. Prev Med 2014;62:71–77. doi: 10.1016/j.ypmed.2014.01.029
[157] Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr 2020;52:102066. doi: 10.1016/j.ajp.2020.102066
[158] Ransing R, Adiukwu F, Pereira-Sanchez V et al. Mental health interventions during the COVID-19 pandemic: a conceptual framework by early career psychiatrists. Asian J Psychiatry 2020;51:102085. doi: 10.1016/j.ajp.2020.102085
[159] Reger MA, Stanley IH & Joiner TE. Suicide mortality and coronavirus disease 2019 — a perfect storm? JAMA Psychiatry 2020. doi: 10.1001/jamapsychiatry.2020.1060
[160] Smith K, Ostinelli E & Cipriani A. Covid-19 and mental health: a transformational opportunity to apply an evidence-based approach to clinical practice and research. Evid Based Ment Health 2020;23:45–46. doi: 10.1136/ebmental-2020-300155


