Introduction
Worldwide, smoking remains the leading cause of preventable death. In 2004, in Great Britain, there were about 14 million regular cigarette smokers, with the prevalence in people aged 16 and above estimated at 26 per cent (28 per cent in men and 24 per cent in women).[1]
The prevalence for England is 25 per cent, for Scotland it is 31 per cent and for Wales it is 27 per cent.[1] In 2001, deaths attributable to smoking in the Wandsworth Primary Care Trust area were estimated at 360, accounting for 18 per cent of all deaths, and the total cost for smoking related illness in this PCT was estimated at £3,749,000.[2]
In the UK, about half of all smokers die prematurely of a smoking-related ailment, representing about 120,000 deaths each year.3 Thirty per cent of cancer deaths (84 per cent of lung cancer deaths) are caused by smoking.[3]
The decrease in life expectancy for regular smokers under the age of 35 years who do not subsequently quit has been estimated to be about eight years, with the annual cost to the NHS of treating patients with smoking-related disease being in the order of £1,500m.[4]
Nicotine is highly addictive; in terms of its addictive potential, it is comparable to cocaine, opiates and amphetamines.[5]
Nicotine replacement therapy (NRT) replaces the nicotine by other means of delivery other than cigarettes. It is available in several formulations and delivery systems, including transdermal patches, chewing gum, lozenges, sublingual tablets, inhalators and nasal sprays. It provides a background level of nicotine that reduces craving and withdrawal symptoms.[4]
It works by getting nicotine into the system without the tar, carbon monoxide and other poisonous chemicals associated with tobacco smoke.[6]
Without the other poisons found in tobacco smoke, nicotine probably has only a small, independent effect on the health of a smoker.[6]
Community pharmacists are ideally placed to provide advice on smoking cessation, and their easy accessibility can encourage people to ask a pharmacist for health advice instead of waiting for a doctor’s appointment.[3]
Since NRT is one of the clinical services already being provided by community pharmacists, this survey aims to investigate its current provision by community pharmacists in Wandsworth PCT. Information generated by the survey will help to recommend ways through which the untapped potential of community pharmacies could be further developed to improve the present level of service.
Method
The study was a descriptive, cross-sectional survey, and generated both quantitative and qualitative data. The sample comprised all 62 community pharmacists working in Wandsworth, London, in January 2005, identified from the PCT’s pharmacy list.[7]
There was no existing questionnaire that addressed the aims of the study, so a new questionnaire was designed that would take around 15 minutes to complete. The items included in the questionnaire were selected based on National Institute for Health and Clinical Excellence guidance, government policies on smoking cessation, and the personal experiences of two of the present authors (GR and MA), both practising GPs. The questionnaire asked about the current provision of NRT by community pharmacists and the level of their involvement. Questions were generally required “yes”, “no” or “don’t know” answers, but each question also had space for further comments or suggestions. Comments were specifically invited on funding or other difficulties encountered, to determine suggestions for service improvement. Questions asked about both negative and positive aspects of the programme. The questionnaire was piloted for content, clarity and format of the questions on a group of 10 community pharmacists working in London, but outside Wandsworth, and no substantive amendments were found to be required.
A postal survey was chosen to save time and cost, and minimise interviewer bias.[8]
Pharmacy addresses were obtained from the NHS website7 and self-addressed envelopes were used to improve the response rate. Non-respondents were sent a second questionnaire in the first instance and, if that failed, were followed up by telephone.
The Wandsworth Research Ethics Committee exempted the study from full ethics committee application and approval. Following the recommendation of the chairman of the committee, the prescribing lead for Wandsworth PCT was notified of, and gave written approval for, the study.
Data were coded, entered into a data set, and verified. Descriptive analyses were conducted, describing frequencies of responses. Free text comments were reviewed and presented thematically.
Results
Of the 62 mailed questionnaires, an initial 18 responses were received. After three weeks, reminders resulted in an additional eight. Telephone calls generated 18 telephone-completed questionnaires, of which one was excluded because insufficient information was provided. One completed questionnaire was received afterwards by mail, bringing the total questionnaires returned to 44, a response rate of 71 per cent (44/62).
Pharmacists’ characteristics
Twenty-five men (57 per cent) and 19 women (43 per cent) responded to the survey. The mean age of respondents was 41 years (SD 11, range 24–65), and the mean time since qualification in the UK was 18 years. Eighteen respondents (41 per cent) were working as pharmacy directors, 16 (36 per cent) as pharmacy managers, five (11 per cent) as locum pharmacists, one (2 per cent) as a relief pharmacist; four (9 per cent) identified themselves as simply “pharmacist”.
NRT-related activities
Thirty-eight respondents (86 per cent) were involved in the management of patients using NRT. The different forms of NRT provided by respondents included participating in a PCT-run scheme for pharmacists (32, 74 per cent), offering over-the-counter advice on NRT (29, 78 per cent) and collaborating with a local practice in a shared care scheme (four, 13 per cent). The NRT programme was PCT-funded for 30 (79 per cent) of these respondents.
Of the six subjects not involved in the management of patients for NRT, among the reasons given for this were that one person was waiting to do NRT training with the local PCT and one person had not yet been accredited by the PCT. For the six subjects involved in an NRT programme which was not PCT-funded, funding came mainly from patients, GPs, the Tooting Health Initiative and the pharmacists themselves.
Two questions ascertained the amount of information pharmacists had regarding the NRT programme. First, pharmacists were asked to indicate how essential it was that patients stop smoking before starting NRT. Twenty-four respondents (56 per cent) said “always”, 10 (23 per cent) “usually”, six (14 per cent) “sometimes” and three (7 per cent) “never”. The second question asked whether the need to provide good four-week quit rates was distorting the NRT programme, given that most pharmacy-based NRT schemes are PCT-funded and “star ratings” depend on four-week quit figures. (The star rating system is a set of Department of Health data indicators by which the performance of health organisations is assessed.[9]
) Eighteen respondents (45 per cent) agreed, 11 (28 per cent) disagreed, and the remaining 11 (28 per cent) did not know.
Problems
Potential problems with the present NRT programme were listed and pharmacists asked to identify the main difficulties; responses are shown in Table 1. Lack of pharmacists’ freedom to prescribe NRT was the highest-ranking difficulty, mentioned by 33 respondents (75 per cent), followed by high drop out rates (26, 61 per cent). Respondents were also asked to suggest any other perceived difficulties. Only one respondent suggested the development of patient group directions (PGDs): “PGDs need to be developed for pharmacists as the current system of referring back to GPs make life harder for clients in terms of time, availability etc.” Delays in getting prescriptions on time and lack of a private counselling area were also identified as difficulties.
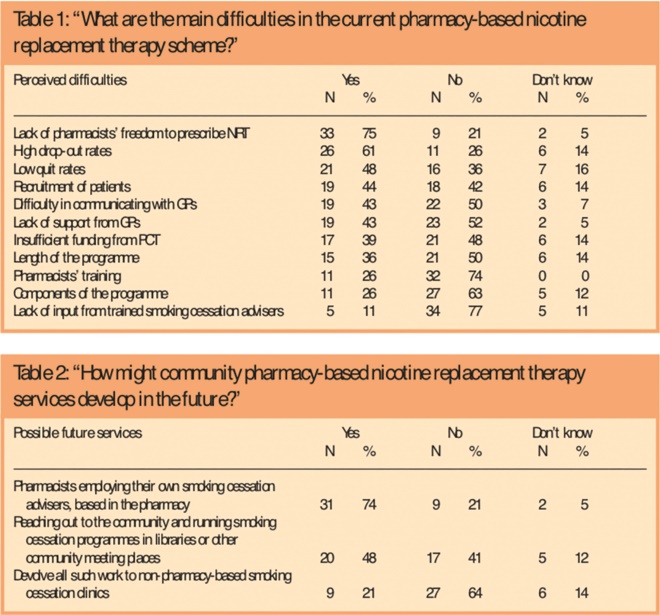
Tables 1 and 2
Solutions
We asked pharmacists to suggest how to overcome these difficulties. Key responses included training GPs to direct patients to trained pharmacists and training the other pharmacy staff (usually dispensers and health assistants) on NRT. Some were of the opinion that better funding could improve the service provided. In addition, many respondents thought that creating awareness of the NRT service provided by community pharmacists, giving prescribing rights to pharmacists, increasing the duration of treatment and improving communication between GPs and pharmacists were also needed.
Future developments
We asked respondents to indicate how community pharmacy-based NRT service might develop in the future. Their responses are presented in Table 2. Other suggestions made included the extension of smoking cessation programmes to schools and day centres.
CHD risks assessment
Finally, pharmacists were asked if they would be willing to determine the blood pressure and cholesterol measurements of patients and use this to perform a coronary heart disease (CHD) risk calculation, using the charts at the back of the BNF. Forty respondents (93 per cent) said “yes”, one (2 per cent) said “no” and two (5 per cent) did not know.
Discussion
Most respondents (86 per cent) were involved in the provision of NRT services. Several problems emerged in the provision of NRT. Lack of pharmacists’ freedom to prescribe NRT, the recruitment of patients, high drop out rates and low quit rates were identified as the main difficulties in the current pharmacy-based NRT schemes.
Most NRT provision (71 per cent) was PCT-funded with the remainder funded from a variety of sources. In some cases, services were funded by the GP or Tooting Health Initiative. We had no further information about other external funding available to support pharmacist-led smoking interventions.
Not all respondents (44 per cent) considered it always essential that patients stop smoking before starting NRT. The new message is that if people cannot stop completely they should use NRT and try to cut their cigarette consumption by at least half over a targeted period (usually six weeks).[10] This approach has been shown to increase the chances of stopping in the longer term.[10]
Perhaps surprisingly, almost all the pharmacists (93 per cent) were willing to perform CHD risk calculation. Clearly, this would result in an expansion of the role of community pharmacy, involving pharmacists in a more comprehensive health promotion assessment and opening up the way for more broadly based interventions.
Of all the difficulties listed by respondents, lack of pharmacists’ freedom to prescribe NRT was the highest-ranking difficulty, being mentioned by 75 per cent of the respondents. Supporting all pharmacists to have prescribing rights for NRT, independent of them being trained as pharmacist prescribers (which they can now do, albeit after a long training course)[11]
will go a long way to improve the quality of NRT services being provided to patients.
Strengths and limitations
The response rate (71 per cent) is relatively high for this type of survey, adding credibility to the results and making the findings more likely to be generalisable to this PCT. Further, most respondents (86 per cent) were in permanent positions and working as pharmacy directors, pharmacy managers or as pharmacists. However, there were several limitations in this study. The sample size was relatively small, consisting of 44 usable questionnaires. Our survey was unable to provide information about how generalisable the findings might be to other areas of London or other PCTs. Finally, there is the possibility that a telephone interview, used after the first written reminder, might have introduced interviewer bias into the study.
How findings match with previous research
As in our own survey, a recent study noted that pharmacists felt knowledgeable and prepared to provide counselling, suggesting that professional educational needs were not hampering the provision of NRT.[12]
Nevertheless, one study has shown that pharmacists’ actions in providing counselling did not always coincide with the clinical practice guidelines.[13]
The suggestion from some respondents on the need to improve communication with GPs was consistent with a US study which also emphasised the need for a multidisciplinary approach to smoking cessation.[14]
Similarly, another study contended that partnerships between prescribers and pharmacists could improve access to and success with prescription smoking cessation therapies.[15]
The inclusion of collaborative practice opportunities in the Practice Acts of many states in the US enable increased participation by pharmacists in the provision of smoking cessation services, by ensuring adequate funding and offering management protocols to guide the intervention.15 Adopting such a strategy in the UK would greatly help to generate pharmacists’ interest in the provision of smoking cessation and other similar services.
At the same time, the NRT services provided by community pharmacists in Wandsworth showed low quit rates and high drop out rates. This was not really surprising, since the stop smoking services provided by community pharmacists involve simply dispensing NRT against prescriptions or recommending NRT over the counter, without providing behavioural support to smokers, or using any motivational interviewing or assessment of a smoker’s position in the stages of change.[16]
Others have pointed out that an inability to identify patients who smoke was a significant barrier in providing effective smoking cessation services.[12]
We recommend that pharmacists be enabled to recruit their own patients for NRT, rather than being dependent upon GP referrals. Although lack of time has been noted by others as a hindrance to implementing NRT, none of our respondents mentioned this directly.[12],[17]
Possibly the use of automated dispensing will make an impact in community pharmacies by freeing time, just as it has done in some hospital pharmacies.[18],[19] The adoption of the recently developed remote supervision model[20]
could also be another way to release time for community pharmacists.
Implication for clinical practice and future research
The results of this study reveal some of the reasons why Wandsworth is currently failing to meet its Department of Health four-week quit target.[2]
By improving collaborative working between doctors and pharmacists, better funding of community pharmacies, continuous training of pharmacists and their staff on NRT and the use of new technologies, Wandsworth is likely to enhance its quit figures on smoking.
Conclusions
Pharmacists are in a strong position to help reduce the impact of smoking-related diseases and therefore reduce the burden of smoking-related morbidity.[21]
This is due to their knowledge of addiction and drugs, and the fact that they are more readily accessible than other health care professionals. Currently pharmacists remain heavily under-used and are often stuck in dispensaries and behind counters.
If community pharmacists are to be effective in reducing overall risk factors for CHD, including smoking, then there will be a need to encourage them to change their working practices. This could be done by developing a system for asking all patients about CHD risk factors and providing access to computerised CHD risk assessments, possibly empowering a technician to perform some of these duties.[22]
We consider that there is also the need to create time for pharmacists through the use of new technologies, better staffing levels, improved funding and minimising the paperwork involved. We recommend that pharmacists be given the freedom to prescribe NRT, whether or not they are trained as pharmacist prescribers.
Acknowledgements
We thank participating community pharmacists in Wandsworth, London. This work was initially a dissertation submitted by Chijioke Agomo as a course requirement of the MSc in health sciences (St George’s, University of London), 2005.
Chijioke Agomo, MSc, MRPharmS, is a locum community pharmacist in London. Gill Rowlands, MD, FRCGP, is director of the Institute of Primary Care and Public Health. Mark Ashworth, DM, MRCGP, is an honorary senior lecturer at King’s College London School of Medicine. Fiona Reid, MSc, is senior lecturer at St George’s department of community health sciences, London.
Correspondence to: Professor Gill Rowlands, Faculty of Health, London South Bank University, 103 Borough Road, London SE1 0AA (e-mail: rowlang2@lsbu.ac.uk)
References
[1] West R. Smoking: prevalence, mortality and cessation in Great Britain. 2005. Available at: www.bluelinewebdesign. co.uk/RobertWest/resources/smokingcessationgb.pdf (accessed 10 November 2006).
[2] Gilfillian V. A report on the Merton, Sutton and Wandsworth stop smoking service. 2004. Available at: www. wandsworth-pct. nhs.uk (accessed 10 November 2006).
[3] Bellingham C. A pharmacist’s role in smoking cessation. Pharmaceutical Journal 2000;265:858.
[4] National Institute for Clinical Excellence. Technology appraisal guidance no 38. Nicotine replacement therapy and bupropion for smoking cessation. London: NICE; 2002.
[5] Jain A. Treating nicotine addiction. BMJ 2003;327:1394–5.
[6] NHS Direct. NHS Direct Online Health Encyclopaedia – Smoking (quitting). Available at: www.nhsdirect.nhs.uk (accessed 7 November 2006)
[7] Pharmacies in Wandsworth Primary Care Trust. NHS in England. 2005. Available at: www.nhs.uk (accessed 10 November 2006).
[8] Bowling A. Research methods in health — investigating health and health services. Buckingham: Open University Press; 1997.
[9] East Surrey NHS Primary Care Trust. Board meeting. Available at: www.eastsurrey-pct.nhs.uk/pct/board/ 200509/enc08.pdf (accessed 7 November 2006).
[10] Armstrong M. Latest stop smoking guidance issued by PharmacyHealthLink. Pharmaceutical Journal. 2005;275:472.
[11] Independent prescribers may be ready for 2007 following Council’s approval of training curriculum. Pharmaceutical Journal. 2006;277:181.
[12] Aquilino ML, Farris KB, Zillich AJ, Lowe JB. Smoking-cessation services in Iowa community pharmacies. Pharmacotherapy 2003;23:666–73.
[13] Fiore MC. US public health service clinical practice guideline: treating tobacco use and dependence. Respiratory Care 2000;45:1200–62.
[14] Maguire TA, McElnay JC, Drummond A. A randomised controlled trial of a smoking cessation intervention based in community pharmacies. Addiction 2001;96:325–31.
[15] Williams DM, Newsom JF, Brock TP. An evaluation of smoking cessation-related activities by pharmacists. Journal of the American Pharmaceutical Association. 2000;40:366–70.
[16] Goldstein MG, MacDonald NA, Niaura R, DubeÌ C. Dissemination of physician-based smoking cessation interventions. In: Shopland DR, Burns DM, Cohen SJ, Kottke TE, Gritz ER (editors). Tobacco and the clinician — interventions for medical and dental practice (monograph 5). Maryland: National Cancer Institute; 1994, pp342–55.
[17] Couchenour RL, Denham AZ, Simpson KN, Lahoz MR, Carson DS. Smoking cessation activities in South Carolina community pharmacies. Journal of the American Pharmaceutical Association. 2000;40:828–31.
[18] Freeborn S. Automated dispensing — the impact on the workforce. Hospital Pharmacist 2000;7:238.
[19] Fitzpatrick R, Cooke P, Southall C, Kauldhar K, Waters P. Evaluation of an automated dispensing system in a hospital pharmacy dispensary. Pharmaceutical Journal 2005;274:763–5.
[20] Bellingham C. Remote supervision becomes a reality. Pharmaceutical Journal 2004;272:377–8.
[21] National Pharmacy Association. Chronic disease management — discussion document. Available at: www.npa.co.uk/pdf/cdisman.pdf (accessed 7 November 2006).
[22] Kennedy DT, Small RE. Development and implementation of a smoking cessation clinic in community pharmacy practice. Journal of the American Pharmaceutical Association. 2002;42:83–92.


