Science Photo Library
Inside tiny wells that are able to hold liquid around a third of the volume of a raindrop, scientists use human cells to examine the potential of a compound to become a drug. Thousands of these drug candidates can be tested each day for the desired biological activity in a process called high throughput screening. Although the compounds may work well on their molecular target, a problem often arises once testing moves inside the body, says Martin Garnett, drug delivery researcher at the University of Nottingham. “These drugs tend to be very hydrophobic and generally quite insoluble.” Insoluble drugs pose a challenge because they are not very well absorbed from the gastrointestinal tract, he explains.
Insolubility isn’t the only issue with getting drug candidates to work inside the body. Targeting of drugs to diseased cells, frequency of dosing and paediatric formulations also pose hurdles. Garnett says that the answer may lie in looking at drug delivery in a holistic way. “How does the body work? How can we get drugs across these barriers? I don’t think we understand diseases in terms of drug delivery and their pathophysiology in that context,” he says, adding that he has “a bit of a bee in the bonnet” about the historical lack of funding that this area of research has attracted.
Nonetheless, new drug delivery methods have started to emerge that aim to improve efficacy, reduce side effects and improve adherence and cost-effectiveness. “There is no shortage of examples of drugs which do not work very well … so, I think we will have plenty of work for years to come,” says Garnett.
Here we review four of the most exciting research efforts in drug delivery:
Nanoparticles
A patient with HIV in the UK usually takes two pills every day, for life — that is 730 pills a year. Although the pill burden for HIV patients has come down significantly, adherence is still an issue. Patients taking a single tablet regimen achieve 95% adherence around 25% of the time and patients on a two-tablet regimen only 17% of the time[1]
. For young children with HIV, adult formulations can also be less than ideal because they contain “harsh organic solvents”, says Andrew Owen, a molecular and clinical pharmacologist at the University of Liverpool. He believes nanotechnology could provide the solution.

Courtesy of Andrew Owen
Andrew Owen (right), a molecular and clinical pharmacologist at the University of Liverpool, is working to develop solid drug nanoparticles of HIV medicines that can improve safety for HIV-positive children and reduce the dosage needed in adults
Owen has been working to develop solid drug nanoparticles of HIV medicines that can improve safety for HIV-positive children. “Everyone agrees that giving children as young as three weeks old drugs that contain alcohol and polyethylene glycol — which is basically antifreeze — is a bad idea.” The main outcome of his paediatric work is a drug formulation of lopinavir that consists primarily of water rather than an organic solvent[1]
, he explains. Nanoparticle formulations of efavirenz and ritonavir have also been created.
To make the solid drug nanoparticle a process called spray drying is used, similar to freeze drying coffee. The drug, along with the excipients, is turned into particles in the nanometre scale. “It leaves a solid format of the excipients with the drug embedded — it’s like a blueberry muffin: the cake is the excipients and the blueberries are the drug,” says Owen. The nanoparticles are then put in suspension in water. Ordinarily, the drugs do not dissolve in water, which is why an organic solvent is used. However, the nanoparticle technique means a solvent is no longer required. “The drug is then indistinguishable from if it was in solution in water because the particles are so small — you take a drug that’s insoluble and basically make it soluble, that’s the benefit.” Garnett, drug delivery researcher at the University of Nottingham, says that this addresses one of the key problems in drug development — that many drugs are highly insoluble.
It leaves a solid format of the excipients with the drug embedded — it’s like a blueberry muffin: the cake is the excipients and the blueberries are the drug
In addition to the potential paediatric benefits, the nanoparticle formulations of lopinavir and efavirenz can dramatically reduce the dosage needed in adults. These formulations were recently tested in nine healthy volunteers, which revealed that only 50% of the standard dose of lopinavir and efavirenz was needed to achieve a therapeutic concentration[2]
. Owen believes this could lead to a reduction in side effects and has the bonus that “twice as many people could be treated with the existing drug supply”.
Owen says his team is not 100% certain of the mechanism of their nanoparticle formulation but they have “a fairly good idea”. In the mucous membrane of the intestine, there are nanoparticle-size pores and they think the particles get embedded in these, so the drug isn’t excreted in faeces. In addition, Peyer’s patches — immune cells that monitor the gut — pick up the particles and take them straight to the lymphatics. “We think it sets up a depot in the lymphatics and avoids first pass metabolism in the liver, maintaining a higher concentration,” says Owen.
One of the challenges is keeping up with changes in preferred drugs. However, Owen is part of an international consortium called OPTIMIZE, funded by the United States (US) Agency for International Development to develop safer and more affordable HIV treatment. With a grant of US$50m, the consortium is helping update the drugs in the formulations.
Pharmaceutical companies ViiV Healthcare — a global specialist HIV company formed in 2009 through a unique partnership between GSK and Pfizer — and Belgium-based Janssen, have also picked up the nanoparticles and are using them to develop a depot injection into the muscle, meaning one injection could provide HIV medications for up to 3 months. Whereas the paediatric and oral formulations are still years away from making it on to the market, the depot injections are in phase II and III clinical trials and might be available “within a year”, explains Owen. “It’s a very exciting area at the moment,” he adds.
The long-acting injectables deliver HIV solid drug nanoparticles directly into the muscle, steadily releasing the drugs over a period of months. ViiV reported in The Lancet in July 2017 that its long-acting preparation injected every four or eight weeks is as effective as daily oral therapy[3]
. “We think … you get infiltration by the immune system, which carries off some of the drug to form a depot in the lymph nodes, while a granuloma forms around the remaining drug in the muscle delaying its release,” says Owen, adding that the strategy could “go a long way to overcoming adherence issues”. But one of the hurdles is that the dose in the muscle is “pretty high — the volume aspect is a real challenge”.
The depot injection is being investigated both as a therapy and prophylaxis. “Effectively, it’s like a vaccine against HIV for all intents and purposes — you just need to top it up every few months.”
Microchip technology
Like a conductor leading an orchestra, timing is everything when it comes to the concert of hormones darting through our bodies each day. These chemical signals make up the endocrine system, which regulates everything from metabolism to bone density. Concentrations in the bloodstream peak and trough, producing a physiological effect in response to only tiny amounts.
Michael Cima, a material scientist and engineer at Massachusetts Institute of Technology (MIT), Boston, believes treatment of endocrine system disorders is the perfect testing ground for his new drug delivery system. Inspired by microchip technology, Cima has created an implantable electronic device that can be wirelessly programmed to release a dose of medication at a specific time each day.
Courtesy of Michael Cima
Michael Cima, a material scientist and engineer at Massachusetts Institute of Technology, Boston, has created an implantable electronic device that can be wirelessly programmed to release a dose of medication at a specific time each day
“The low-hanging fruit, where this therapy is needed, is the treatment of dysregulation of the endocrine system,” says Cima. For example, a lot of the side effects of the contraceptive hormone implant, such as breakthrough bleeding and bloating, are caused by the continuous release of hormones into the bloodstream, he says.
In the late 1990s, Cima was thinking about how to use electronics to improve drug delivery. “The idea sort of stemmed from pacemaker-type technology, but instead of delivering an electrical signal you deliver a drug.” So Cima and Robert Langer, a biomedical engineer at MIT, co-founded a company called Microchips Biotech and released a prototype in 1999, reported in Nature
[4]
.
The idea sort of stemmed from pacemaker-type technology, but instead of delivering an electrical signal you deliver a drug
Now, the researchers have completed their first human trial and in 2015 received a US$35m grant from Israeli multinational pharmaceutical company Teva to take the work forward. Results from the trial were published in 2012 and “proved that the device works”, says Cima[5]
. Eight women were given the implant containing human parathyroid hormone fragment for the prevention of osteoporosis. The study was primarily to assess safety, but biomarkers for bone regeneration were also measured to see if it was working. “It showed that not only could we deliver the drug … [but] based on the biomarkers, it was actually effective.”
“Interestingly, if you were to make a device that released the drug constantly … it would actually cause bone to resorb. It’s the daily spike of hormone that causes the body to generate more bone,” says Cima.
Standard treatment for osteoporosis involves a daily injection of parathyroid hormone for 18 months. Cima explains that treatment is prophylactic “so it’s hard for patients to feel motivated to inject themselves every day — a large proportion discontinue by month seven”. In contrast, the chip can “ensure compliance with these very expensive therapies”, says Cima.
Martin Garnett, drug delivery researcher at the University of Nottingham, says he thinks the main advantage of the chip is the possibility for better control of medication and disease management, but adds that its potential is probably limited to specific disease areas.

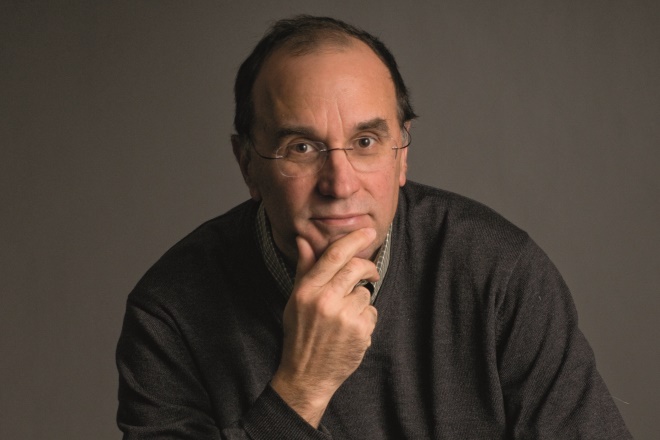
Courtesy of Martin Garnett
Martin Garnett, drug delivery researcher at the University of Nottingham, says he has a bit of a bee in his bonnet about the historical lack of funding that drug delivery research has attracted
In the clinical trial for osteoporosis, the chips were remotely programmed to release the drug once daily for up to 20 days and were left implanted for four months. Putting the device in involves a small surgical procedure to insert it underneath the skin and removal is the opposite, although it could just be turned off remotely instead, says Cima. “Women in the study had relatively large chip implants, but they didn’t notice it,” he adds.
Since completing the study, the group is working on making the chip “very small — about the size of the smallest pacemaker”. The current model is down to about 2.4cm by 2.9cm and the group is also working to increase the number of doses that can be loaded on to a chip. In the osteoporosis study, the chip contained 25 individual dose reservoirs, “we need to increase that to about 400 reservoirs”. Cima reckons it might be around six years before the chip makes it on to the market, but he says “with a chip we have the opportunity to mimic the natural release of hormones”.
Microneedle patches
No one likes injections, which is why researchers are currently giving the humble plaster a makeover. By attaching microneedles to a flexible sticker, drugs could soon be administered subcutaneously without even so much as a prick.
The tactic has recently been proven to work for the flu vaccination and, in the US, a team has taken this idea even further: the smart plaster. It releases drugs only when needed by monitoring the blood. “We wanted to develop a smart patch — the right dose at the right time,” says Zhen Gu, a biomedical engineer at University of North Carolina Chapel Hill, US. His team has developed a patch that responds to blood clotting factors by releasing heparin into the blood stream to prevent thrombosis, which can cause strokes and heart attacks and is one of the leading causes of death in the UK.

Courtesy of Zhen Gu
Zhen Gu (fourth from right) a biomedical engineer at University of North Carolina Chapel Hill, US, and his team, have developed a patch that responds to blood clotting factors by releasing heparin into the blood stream to prevent thrombosis
Current administration of heparin requires careful monitoring. “Too much causes bleeding and too little allows clotting,” says Gu. In comparison, the smart patch only releases the amount of heparin that’s needed.
To create the device, the team uses a protein linker to attach heparin to hyaluronic acid — a substance that occurs abundantly in the soft tissue of the body — to create a polymer. The polymer is then shaped into a series of tiny pointed needles which are attached to a plaster that is placed on the skin. Once applied, the microneedles penetrate the skin and if the protein linker is exposed to thrombin — an enzyme that triggers blood clotting — it is cleaved off. “So as the risk of forming clots increases, more heparin is released,” explains Gu.
In tests on mice, the device was more effective than injected heparin at preventing clotting[6]
. Mice were given either an injection of heparin, the smart patch or no treatment. Thrombin was then administered to trigger blood clotting. All the mice given the smart patch or the heparin injection survived, while the rest died. When an injection of thrombin was given 6 hours after administration of heparin, all the mice with the smart patch survived but only 80% of the mice given the heparin injection survived.
Next, the researchers plan to study the patch in larger animals to understand exactly how much heparin needs to be loaded on to a patch to protect humans. “For mice, the patch is around the size of one cent (0.75 inches in diameter), but for humans it will need to be a bit larger,” says Gu.
In the meantime, another research group has been developing a microneedle patch of its own that was successfully tested in humans recently. Gu calls it a “milestone for the transition of the microneedle patch to humans — it’s very exciting”.
The patch in question is a flu vaccine microneedle patch invented by Mark Prauznitz, a chemical and biomedical engineer at Georgia Institute of Technology, Atlanta, Georgia. The patch looks like the one created at Gu’s lab but lead author Nadine Rouphael, an infectious diseases researcher at Emory University, explains that the needles are made from the flu vaccine and that they “completely dissolve inside the skin”, which triggers an immune response. She says the patch might be useful for children or for patients who simply feel they don’t have the time to get vaccinated. It can be self-administered so could even be sent by mail to patients, adds Rouphael. She also believes the patch might be useful for vaccination against diseases such as polio, rubella and measles in developing countries. “The good thing about it is because it’s in a solid form, the vaccine is very stable outside the fridge — one year at 40 degrees [celsius], and it doesn’t generate sharps waste,” she says.
The good thing about it is because it’s in a solid form, the vaccine is very stable outside the fridge — 1 year at 40 degrees, and it doesn’t generate sharps waste
The recent flu trial included 100 patients and was primarily to test safety and tolerability[7]
. To administer the patch, it is placed on the wrist with pressure and peeled off after 20 minutes. The researchers found that pain was reported with half the frequency in the microneedle patch group compared with the intramuscular injection group. “It’s liked by patients,” says Rouphael.

Courtesy of Nadine Rouphael
Nadine Rouphael, an infectious diseases researcher at Emory University, is testing a flu vaccine microneedle patch, which she says can be self-administered and might be useful for children or for patients who feel they don’t have the time to get vaccinated
In addition, the patch appeared to be just as effective at stimulating the immune system. “It led to excellent immunological results,” says Rouphael. Bigger trials are needed before the patch hits the market but Rouphael is optimistic: “we haven’t seen any disadvantages so far”.
Ultrasound-guided delivery
High-frequency sound waves beamed into our bodies can penetrate to depths of up to 30cm. As the vibrations travel through the body, they are reflected at different rates depending on the type of tissue. This is the premise of ultrasound imaging. But now ultrasound is also being explored as a way to target drugs to tumours.
At Ulster University in Northern Ireland, researchers have developed microbubbles filled with oxygen and coated with a drug. The bubbles float through the bloodstream harbouring their cargo until they encounter the ultrasound beams and then they burst. “By positioning the ultrasound at the tumour, it allows you to selectively destruct the bubbles to make a targeted drug delivery vehicle,” says John Callan, a pharmaceutical scientist at Ulster University.
By positioning the ultrasound at the tumour, it allows you to selectively destruct the bubbles to make a targeted drug delivery vehicle
Callan’s team has worked in collaboration with Eleanor Stride, a biomedical engineer at Oxford University, and Mark Taylor, a pancreatic cancer surgeon. They chose to test the method on pancreatic cancer because it only has a 4% five-year survival rate, which has not changed in 40 years. “So in that context we said OK, how can we use our targeted delivery method to improve the effectiveness of pancreatic cancer treatment while at the same time spare healthy tissue and reduce side effects?” explains Callan.

Courtesy of John Callan
John Callan, a pharmaceutical scientist at Ulster University, and his team, are exploring ultrasound as a way to target drugs to tumours
The microbubbles have a lipid shell and contain a core of oxygen, and either have an ultrasound sensitiser drug attached to the surface or the chemotherapeutic agent 5-fluorouracil. The sensitiser drug, called rose bengal, is harmless on its own. But when it is activated by ultrasound it sets off a chain reaction in the oxygen gas that damages tumour tissue, a technique called sonodynamic therapy. Using a combination of microbubbles with rose bengal and those with 5-fluorouracil led to reductions in tumour size in mice, which were significantly better than treatment with the standard chemotherapeutic drug gemcitabine[8]
. The team has since tested microbubbles with gemcitabine attached instead of 5-fluorouracil, which Callan says allowed them to use a dose of the drug 100 times lower than standard gemcitabine, but with better results. Callan says “we are extremely excited about this technology and hope it will some day make a real difference to the outcome for pancreatic cancer patients”.
Fortunately, microbubbles are already approved for use in humans to improve visualisation on ultrasound. Callan is therefore confident that the collaboration will win approval for a human trial from the Medicines and Healthcare products Regulatory Agency. “It’s putting the microbubble together as a combined drug delivery and therapy package that’s the novel thing,” he explains.
In the US, the idea of using ultrasound-guided drug delivery is also attracting attention. A team at the Wyss Institute at Harvard University, Boston, Massachusetts, has developed a nanoparticle aggregate of doxorubicin to treat breast cancer. Netanel Korin, a biomedical engineer formerly at Wyss and now at the Israel Institute of Technology, says that the aggregate is “like a sand ball — but it doesn’t break apart in the body; it only breaks apart with ultrasound”. When this happens, the individual nanoparticles can infiltrate tissue and release the drug over time, explains Korin.
Martin Garnett, drug delivery researcher at the University of Nottingham, says that it is interesting that both projects use relatively large particles. This can mean a shorter half-life in the bloodstream, he says. He also explains that “if they manage to localise the carrier in the tumour however, the ultrasound will do its job”.
He adds that the technique at Wyss tries to address one of the problems with nanoparticle drug delivery — that less than 5% of the particles injected actually reach the tumour site and that drugs tend to leach out of individual nanoparticles. In contrast, the drug stays inside the aggregate and the release of the free nanoparticles can be concentrated at the tumour site, explains Anne-Laure Papa, a researcher at Wyss. The clinical benefits of the approach are similar to the project at Ulster. “We could use much less drug and still reduce tumour size — you can get a better response and without the side effects,” says Korin.
Studies in a mouse model of breast cancer have so far proved promising[9]
. Tumour size was reduced significantly more using the doxorubicin nanoparticle aggregates with ultrasound compared with non-aggregated nanoparticles or doxorubicin alone. To get an equivalent reduction in tumour size using doxorubicin, the dose had to be increased 20-fold, but this resulted in 40% of the mice dying from toxicity. “Our study is proof of principle,” says Korin, while Papa adds: “I can’t wait to see how we can develop the second generation.”
References
[1] Giardiello M, Liptrott NJ, McDonald TO et al. Accelerated oral nanomedicine discovery from miniaturized screening to clinical production exempliï¬ed by paediatric HIV nanotherapies. Nat Commun, online 21 October 2016. doi: 10.1038/ncomms13184
[2] Owen A. Human confirmation of oral dose reduction potential of nanoparticle ARV formulations. Conference on Retroviruses and Opportunistic Infections. Presented 14 February 2017. Available at: http://www.croiconference.org/sessions/human-confirmation-oral-dose-reduction-potential-nanoparticle-arv-formulations (accessed September 2017)
[3] Margolis DA, Gonzalez-Garcia J, Stellbrink H-J et al. Long-acting intramuscular cabotegravir and rilpivirine inadults with HIV-1 infection (LATTE-2): 96-week results of a randomised, open-label, phase 2b, non-inferiority trial. Lancet, online 24 July 2017. doi: 10.1016/S0140-6736(17)31917-7
[4] Santini J, Cima M & Langer R. A controlled-release microchip. Nature 1999;397:335–338. doi: 10.1038/16898
[5] Farra R, Sheppard N F, McCabe L et al. First-in-human testing of a wirelessly controlled drug delivery microchip. Sci Transl Med, online 16 February 2012. doi: 10.1126/scitranslmed.3003276
[6] Zhang Y, Yu J, Wang J et al. Thrombin-responsive transcutaneous patch for auto-anticoagulant regulation. Adv Mat, online 25 November 2016. doi: 10.1002/adma.201604043
[7] Rouphael N, Paine M, Mosley R et al. The safety, immunogenicity, and acceptability of inactivated influenza vaccine delivered by microneedle patch (TIV-MNP 2015): a randomised, partly blinded, placebo-controlled, phase 1 trial. Lancet, online 27 June 2017. doi: 10.1016/S0140-6736(17)30575-5
[8] McEwan C, Owen J, Stride E et al. Oxygen carrying microbubbles for enhanced sonodynamic therapy of hypoxic tumours. J Controlled Release 2015;10:51–56. doi: 10.1016/j.jconrel.2015.02.004
[9] Papa AL, Korin N, Kanapathipillai M et al. Ultrasound-sensitive nanoparticle aggregates for targeted drug delivery. Biomaterials. 2017. doi: 10.1016/j.biomaterials.2017.06.003