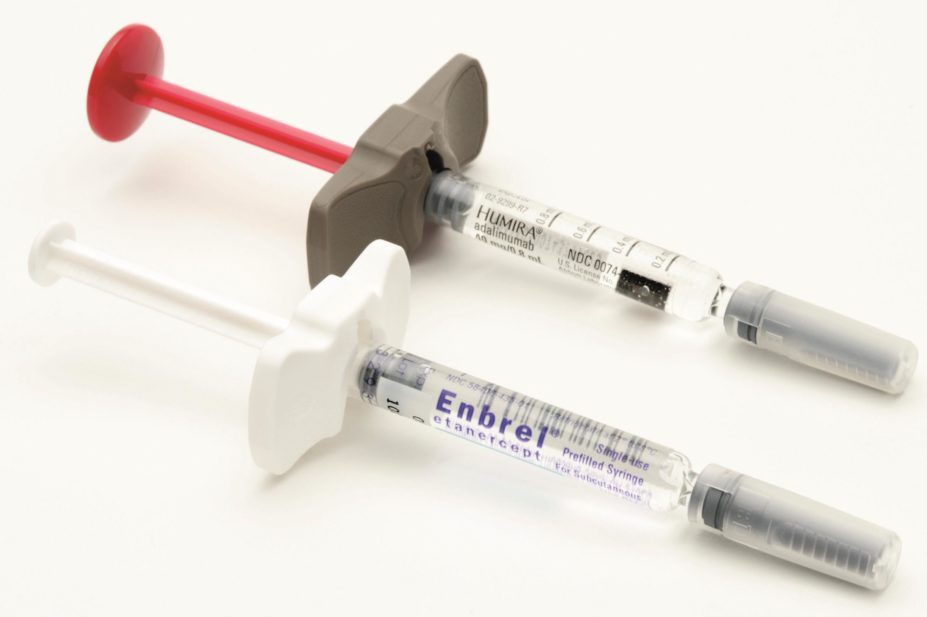
Martin Shields / Alamy Stock Photo
Biosimilar tumour necrosis factor (TNF)-α inhibitors have similar efficacy and safety profiles to their branded equivalents, the authors of a systematic review conclude.
The researchers, led by Caleb Alexander, associate professor of epidemiology and medicine at Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland, say the results could have significant implications for healthcare systems at a time when biologic drugs are beginning to come off-patent and cheaper biosimilar versions are becoming available.
“These findings are big news, because TNF-alpha inhibitors are a costly and commonly used class of biologics and it hasn’t been clear whether TNF-alpha biosimilars are as safe and effective as their branded counterparts,” Alexander says.
Doubts have previously been raised over the equivalence of biosimilars because the function of biologics is so closely related to their structure – even small changes that arise during the manufacturing process can impact on pharmacological activity.
The paper, which is published in the Annals of Internal Medicine
[1]
(online, 2 August 2016), looked at 19 studies involving seven biosimilars for etanercept, infliximab and adalimumab. Eight studies were phase I trials, five were phase III trials and six were observational studies.
The researchers found that the efficacy profiles of biosimilar TNF-α inhibitors showed equivalence with those of their reference biologics. In all phase I trials, pharmacokinetic outcomes fell within the prespecified equivalence margin of 80%–125%. In the phase III trials, which involved patients with rheumatoid arthritis, achievement of the primary clinical end points was comparable between biosimilar and reference biologics in all studies.
The researchers also found that most treatment emergent adverse events were mild or moderate in severity and there were no notable differences in the type or prevalence between groups.
The ten trials that considered immunogenicity, an important factor in biologic efficacy as antidrug antibodies can impair clinical response, found that the drugs were broadly the same across treatment groups, with the exception of trials involving the etanercept biosimilar SB4. These studies found that fewer patients produced antidrug antibodies to SB4 than the reference biologic.
The two observational studies that considered immunogenicity showed that anti-infliximab antibodies cross-react with the biosimilar CT-P13. But some small, uncontrolled studies that looked a switching from the branded version (Remicade) to the biosimilar suggested that efficacy was maintained. The researchers say that they hope their findings will result in better uptake of biosimilar TNF-α inhibitors. They say that increased competition in this area of the pharmaceutical market – which is estimated to represent 20% by next year – will benefit patients and save healthcare systems money.

Courtesy of Caleb Alexander
Caleb Alexander, associate professor of epidemiology and medicine at Johns Hopkins Bloomberg School of Public Health, says further work is needed to look at the efficacy of other types of biosimilars
“Hospitals and health systems have a vital role to play in facilitating the adoption of biosimilar products through the development of guidelines and clinical policies that promote their use,” says Alexander, but adds that further research is needed to see if the findings hold true for other types of biosimilars.
“We examined a single important class of biologics – further work is needed to characterise the real world safety and effectiveness of other biosimilar products,” he says.
In Europe, manufacturers are required to demonstrate equivalence of physicochemical characteristics, adverse effects, and clinical efficacy between the biosimilar and the reference biologic for marketing authorisation. The European Medicines Agency has so far issued three authorisations for infliximab biosimilars and one for an etanercept biosimilar.
Natalie Carter, head of research and evaluation at the charity Arthritis Research UK, says the results of the review are encouraging but further research is needed. “The findings indicate that biosimilars are interchangeable with their predecessors, which is great news,” she says.
“However, these are small sample sizes and more research needs to be done to understand their suitability for the millions of people living with the daily pain caused by arthritis.”
Carter adds: “We welcome the continued development of biosimilars which have the potential to bring greater choice of treatment to people with inflammatory arthritis.”
References
[1] Chingcuanco F, Segal JB, Kim SC, et al. Bioequivalence of Biosimilar Tumor Necrosis Factor-# Inhibitors Compared With Their Reference Biologics. Annals of Internal Medicine 2016; doi: 10.7326/M16-0428


