Alamy Stock Photo
1. Biological medicines, or biologics, are medicines that are made or derived from a biological source, such as living cells or organisms
Most biologics in current clinical use contain active substances made of proteins that can differ in size and structural complexity, from simple proteins, such as insulin or growth hormone, to more complex proteins, such as coagulation factors or monoclonal antibodies[1]
.
Biologics offer treatment options for patients with chronic and often disabling conditions, such as diabetes, autoimmune disease and cancers[2]
.
A biosimilar is a biologic that is highly similar to a biologic that is already approved (the originator). The clinical performance of the biosimilar and the originator are expected to be the same[3]
.
2. The European Medicines Agency evaluates biosimilars according to the same standards as all biologics approved in the EU
Biologics are larger and more complex than typical small molecule drugs, so the manufacturing process is highly complicated and they are difficult to produce[1]
.
Manufacturers, who are regularly inspected, must hold a license and are legally obliged to comply with good manufacturing practice.
The EU has approved the highest number of biosimilars worldwide, although three of these have since been withdrawn for commercial reasons
The EU has pioneered regulation of biosimilars by establishing a rigorous framework for their approval. The EU approved the first biosimilar in 2006 – the growth hormone somatropin[1]
. Since then, with the total currently at 46, the EU has approved the highest number of biosimilars worldwide, although three of these have since been withdrawn for commercial reasons.
The European Medicines Agency (EMA) evaluates biosimilars according to the same standards of pharmaceutical quality, safety and efficacy that apply to all biologics approved in the EU, in comparison to the originator.
When a company applies for marketing authorisation from the EMA, data are evaluated by the EMA’s scientific committees on human medicines and safety, as well as by EU experts on biologics and biosimilars. The EMA then sends a scientific opinion to the European Commission, which ultimately grants an EU-wide marketing authorisation.
Where the National Institute for Health and Care Excellence has recommended the originator biologic, the same guidance will normally apply to a biosimilar.
3. Biosimilars are typically much cheaper than the originator, enabling the NHS to make savings
This commercial competition provides the NHS with the opportunity to save vast amounts of money, while also increasing access and choice for patients and clinicians.
According to NHS England, by embracing the use of the ‘best value’ biologics, it could save at least £200m–£300m per year by 2020/2021.
Switching to the latest biosimilars infliximab, etanercept and rituximab saved the NHS in England £210m in 2017/2018.
4. Procurement and tender exercises are carried out according to the region/country
The NHS England Commercial Medicines Unit (CMU) typically runs regional procurement and tender exercises and the successful products then go on to a framework agreement[4]
. Hospital trusts will then purchase from the individual manufacturer using the terms in that framework agreement.
The tenders are coordinated nationally and the resulting frameworks are delivered at a four region level model (North, South, London, Midlands and East).
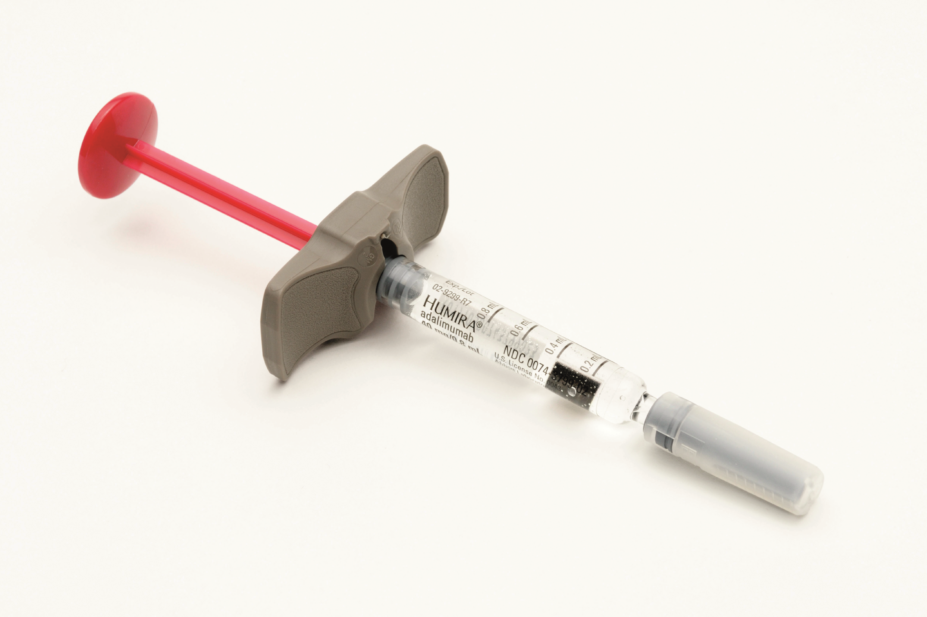
The NHS England CMU is scheduling the procurement process for adalimumab after the loss of patent exclusivity in October 2018 and it is likely the contract will be in place by December 2018.
NHS National Procurement, the centre of procurement expertise for health in Scotland, will be tendering for the future supply of biosimilar adalimumab on behalf of NHS Scotland, and in Wales, the All Wales Drugs Contracting Committee will lead the procurement exercise.
The adalimumab biosimilars approved for use in the UK, but still subject to the procurement exercise, are: Amgevita (Amgen), Hyrimoz (Sandoz) and Imraldi (Samsung Biogen). The products will be reviewed on an ongoing basis as information concerning the products, including formulations and administrative devices, becomes available.
This information may be accessed through the local UK Medicines Information Centre[5]
.
5. There are no specific targets for switching to biosimilars but some incentives are in place to support uptake
NHS England has developed a Commissioning for Quality and Innovation (CQUIN) framework to support uptake of ‘best value’ medicines in specialised commissioning, with a focus on generics and biologics, including biosimilars[4]
.
For biologics, the 2017/2019 CQUIN payment is given to a trust if it demonstrates:
- Adoption of ‘best value’ biologics, including biosimilars, in 90% of new patients within one quarter of guidance being made available;
- Adoption of ‘best value’ biologics, including biosimilars, in 80% of applicable existing patients within one year of being made available (except if standard treatment is less than six months).
The NHS England Medicines Optimisation Dashboard presents data on the take-up of biosimilars by hospital trusts and allows comparison between them.
There are no national prescribing incentive schemes such as CQUIN in Scotland — Scottish NHS boards may choose to invest in additional resource within clinics, where required, to support maximising the benefits from the introduction of biosimilar adalimumab.
There are an estimated 18 important biologics coming off patent by 2023
In Wales, a national prescribing indicator is in place to support biosimilar uptake, including adalimumab. No absolute target is set in relation to the level of use, however health boards are expected to maximise uptake of ‘best value’ biologic products.
6. There are currently 14 reference or ‘originator’ biological medicines that have biosimilars approved for use in the UK
These are infliximab, etanercept, rituximab, adalimumab, trastuzumab, bevacizumab, enoxaparin, insulin glargine, insulin lispro, teriparatide, follitropin alfa, somatropin, filgrastim and epoetin.
There are an estimated 18 important biologics coming off patent by 2023, including trastuzumab, alemtuzumab and bevacizumab. For a full list, see ‘Preparing for the big biologic switch’.
7. The process for deciding which biosimilars are incorporated in the local formulary is separate for each country
If a biosimilar has been selected through the tender and procurement process by the CMU it will be available but it is up to individual hospital trusts and relevant commissioners to decide which biosimilars they will incorporate in the local formulary.
At the time of dispensing there must not be automatic substitution of the originator with a biosimilar. Therefore, the clinician in consultation with the patient should make the decision on whether the originator or biosimilar will be prescribed for the patient.
After the launch of the biosimilar adalimumab in Scotland, National Procurement will provide NHS boards with an updated ‘best value’ biologic treatment cost comparison tool to support boards in reviewing the local formulary advice and prescribing guidelines. This will enable boards to ensure that they continue to recommend the most cost-effective treatment options.
In Wales, the All Wales Drug Contracting Committee will undertake a procurement exercise to determine which biologic should be included in local formularies and oversee compliance with any national framework contract.
8. Patients may have concerns about switching to a biosimilar
Patients should be fully informed in a face-to-face discussion with a familiar healthcare professional about what can be expected when starting treatment with a biologic or when switching from one biologic to another. Leaflets should also be available for patients to take home.
It is important for patients to understand that regulatory bodies have recommended that all biologics, including biosimilars, are prescribed by their brand name
Pharmacists should be aware of the available products and reassure patients regarding the rigorous regulatory process the biosimilar has gone through to ensure quality, safety and efficacy.
To ensure that patients understand which medicine they are being prescribed, especially if being switched from an originator biologic to a biosimilar, it is important for patients to understand that regulatory bodies have recommended that all biologics, including biosimilars, are prescribed by their brand name, as opposed to their generic name. This recommendation is in line with Medicines Healthcare products Regulatory Agency guidelines and has been endorsed by patient and healthcare professional organisations across Europe.
Any forthcoming biosimilars and potential change to homecare services should be communicated to all patients as early as possible and at least two weeks before a switch[6]
.
NHS England have developed a template patient letter, patient newsletter and a set of frequently asked questions in partnership with national patient organisations, which are available on the Specialist Pharmacy Service (SPS) website[4]
.
Information is also available on patient organisation websites, such as the National Rheumatoid Arthritis Society website.
9. Targeted support is available to help inform clinicians about biosimilars
As uptake of biosimilars increases, doctors, nurses and pharmacists may require a more in-depth understanding of the NHS’s position regarding uptake of the ‘best value’ biologics and which biologics, including biosimilars, are available in the specialities in which they are providing care. This will enable them to engage with patients, answer any questions they may have and provide reassurance where necessary.
Doctors can also be referred to the SPS website where a ‘Briefing for clinicians’, developed by the NHS England Regional Medicines Optimisation Committees (RMOCs), is available to download to help answer any questions or concerns they may have.
10. There are several resources pharmacists can use
NHS England briefings, developed during the countdown to the patent expiry of the originator adalimumab, are available to view on the SPS website. They advise on the next steps for commissioners and providers, provide practical advice in the context of homecare services, and outline progress to date in planning for the patent expiry of adalimumab.
In addition, in partnership with NHS England, the commissioning support units have produced an interactive toolkit for use by commissioners and providers to support implementation of best value biological medicines and this has been complemented with regional webinars.
The Cancer Vanguard, a partnership led by three London NHS trusts, has also built a resource around its biosimilar adoption process, which can be used by healthcare professionals across the NHS to assist with the adoption of biosimilars in their own trusts.
In Scotland, Healthcare Improvement Scotland has developed a prescribing framework for biosimilars, which was published in March 2018. The framework builds on previous best practice and aims to promote the safe use of biosimilars, encourage shared decision making between healthcare professionals and patients, and ensure a consistent approach across Scotland[7]
.
References
[1] European Medicines Agency & European Commission. Biosimilars in the EU: Information guide for healthcare professionals. 2017. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/Leaflet/2017/05/WC500226648.pdf (accessed October 2018)
[2] European Medicines Agency. Biosimilar medicines. 2018. Available at: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/general/general_content_001832.jsp&mid=WC0b01ac0580bb8fda (accessed October 2018)
[3] Association of the British Pharmaceutical Industry & UK BioIndustry Association. Biological and biosimilar medicines in the UK. 2014. Available at: http://www.abpi.org.uk/media/1391/biological_biosimilar_medicine_uk.pdf (accessed October 2018)
[4] NHS England, NHS Improvement & NHS Clinical Commissioners. Commissioning framework for biological medicines (including biosimilar medicines). 2017. Available at: https://www.england.nhs.uk/wp-content/uploads/2017/09/biosimilar-medicines-commissioning-framework.pdf (accessed October 2018)
[5] NHS England. Regional Medicines Optimisation Committee briefing best value biologicals: adalimumab update 3. 2018. Available at: https://www.sps.nhs.uk/wp-content/uploads/2018/07/Adalimumab-RMOC-Briefing-Final-July.pdf (accessed October 2018)
[6] NHS England. Regional Medicines Optimisation Committee briefing best value biologicals: adalimumab update 2. 2018. Available at: https://www.sps.nhs.uk/wp-content/uploads/2018/05/Adalimumab-RMOC-Briefing-Final-May.pdf (accessed October 2018)
[7] Healthcare Improvement Scotland. Biosimilar medicines: a national prescribing framework. 2018. Available at: http://www.healthcareimprovementscotland.org/idoc.ashx?docid=93faeca2-1f4d-4ffc-a41f-7a17909ae236&version=-1 (accessed October 2018)

