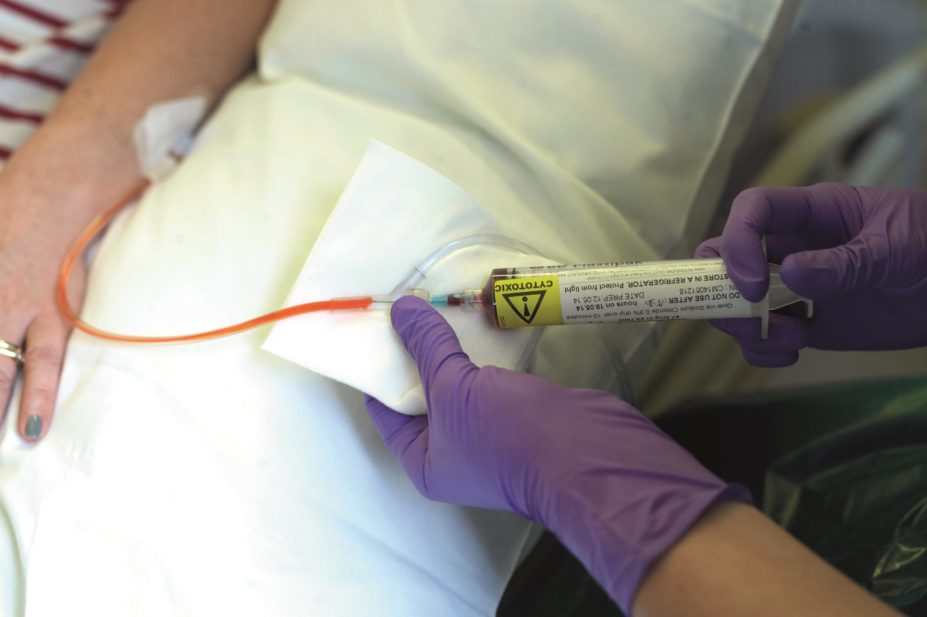
Lifestyle Photographer / Alamy Stock Photo
NHS England is pushing ahead with its proposed changes for England’s Cancer Drugs Fund (CDF), which will be run by the National Institute for Health and Care Excellence (NICE) from 1 July 2016 in an attempt to plug a growing hole in the fund’s budget.
NHS England set out its proposals for the CDF on 25 February 2016 and confirmed that the CDF would be run as a managed access fund, “with clear entry and exit criteria”, from July. The proposals follow a 12-week public consultation on the CDF that ended on 11 February 2016.
The CDF’s annual budget was increased from £200m in 2011–2012 to £340m in 2015/16. Despite this, the fund has exceeded its allocated budget each year since 2013–2014. A number of drugs and their indications were ‘de-listed’ from the fund in 2015 in an attempt to reduce this overspend.
The CDF has bypassed NICE for five years, and would typically fund medicines the institute deemed not cost effective. However, from July 2016, NICE will play a central role in deciding which drugs are funded, leading to fears that many new oncology treatments will be axed as a result of their price tags. Patients taking medicines funded via the CDF prior to July will continue to have their treatments funded.
The Association of the British Pharmaceutical Industry (ABPI) estimates that two thirds of existing CDF medicines are likely to no longer be available to NHS patients under the planned managed access fund.

Source: Association of the British Pharmaceutical Industry (ABPI)
Substantial change is needed to the way that NICE appraises cancer medicines, says Paul Catchpole (pictured), value and access director at the ABPI
“If cancer medicines go through more or less exactly the same NICE appraisal process that was in place five years ago — which necessitated the setting up of the CDF in the first place — we will largely get the same answers as before – the majority of medicines will be turned down,” says Paul Catchpole, value and access director at the ABPI. “Substantial change is needed to the way that NICE appraises cancer medicines to prevent this.”
The CDF was set up in 2010 as an interim budget due to end in April 2016. It was put in place to help bridge the gap in access to treatments before the creation of a new drug pricing system proposed by the then health secretary Andrew Lansley, known as value-based pricing (VBP), but this system failed to be approved.
Some charities have warned that the new CDF could deny patients access to the 47 medicines currently funded via this silo budget. The Rarer Cancers Foundation says almost 22,000 patients could lose out each year because of the changes.
Mark Flannagan, chief executive of the Beating Bowel Cancer UK charity, says he is concerned. “Many bowel cancer patients will lose out as a result of this. The CDF has always just been a sticking plaster — we all want to work toward a sustainable future, but I think that can only happen if NICE and its QALY formula [which is used to create a cost-effectiveness model for new drugs] is assessed and radically updated.
“We’ve argued with ministers about new ways of doing this, such as by asking pharma companies to run a system based on payments by results, but the government just isn’t interested,” he adds.
However, Cancer Research UK welcomed the move. Harpal Kumar, the charity’s chief executive, says the proposals are a “positive step in creating a more sustainable and flexible system”.
“Importantly, we believe the proposals will bring more certainty to patients and doctors about the drugs that can be prescribed, and swifter access to promising drugs,” Kumar says.
NHS England board papers state that the operational detail of the new scheme will be developed “over the coming months” and that a new standard operating procedure for the fund will be published by June 2016.