Wikimedia Commons
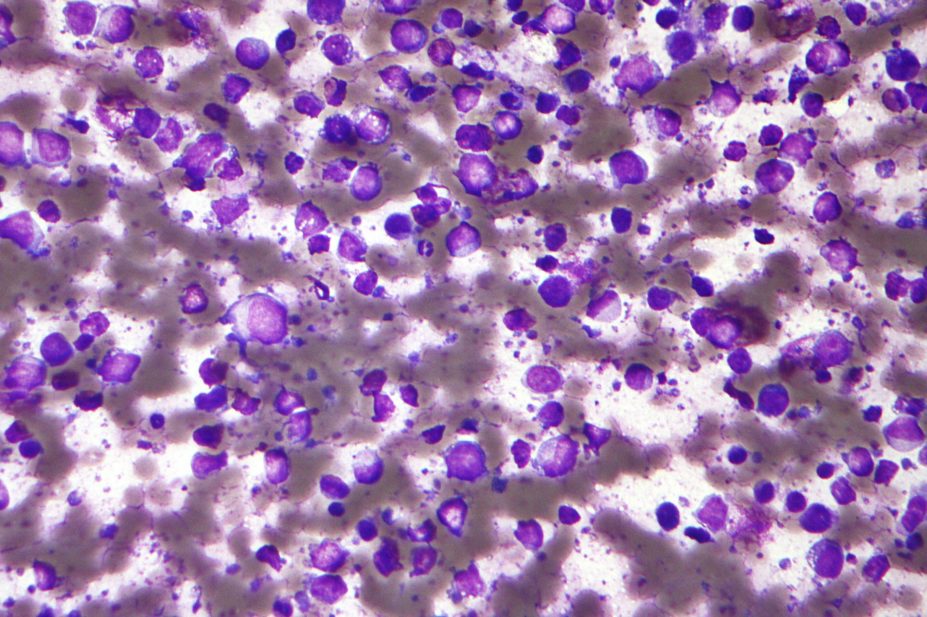
A bispecific antibody has been developed by researchers at US biotech company Genentech, who claim it is “highly active” against leukaemia and lymphoma cells.
The antibody has a different mechanism of action to the monoclonal antibody rituximab, which is currently used to treat blood cancers, and preclinical testing suggests it could circumvent rituximab resistance. The findings were published in Science Translational Medicine
[1]
on 13 May 2015.
A bispecific antibody is made by fusing fragments of two different antibodies, allowing it to simultaneously bind to two types of antigen. This latest bispecific antibody binds to a target on the surface of a patient’s T cells (CD3) and a target on their leukaemia or lymphoma cells (CD20). In this way, a patient’s T cells are redirected to attack cancer cells.
This so-called B cell-targeting anti-CD20/CD3 T cell-dependent bispecific antibody (CD20-TDB for short) is a full-length, humanised immunoglobulin G1 molecule with the near-native architecture of a typical antibody. It was constructed using what is known as “knobs-into-holes” technology, which favours the heterodimer production essential for an antibody that recognises two different antigens at once.
In cynomolgus monkeys, CD20-TDB wiped out B cells in peripheral blood and lymphoid tissues at a single dose of 1mg/kg, the researchers found. The bispecific antibody demonstrated pharmacokinetic properties similar to those of conventional monoclonal antibodies, like rituximab.
“CD20-TDB administration in cynomolgus monkeys demonstrated a pharmacokinetic profile typical of IgG1 monoclonal antibodies,” writes Liping Sun, research oncologist at Genentech, California, and co-authors. This is important, says Sun, because it will enable intermittent dosing schedules that can be combined with current standard therapies for B cell malignancies. Indeed, CD20-TDB was found to be active in the presence of high concentrations of rituximab, and since CD20-TDB and rituximab have different mechanisms of action, they could potentially be combined, enabling flexible treatment strategies.
Sun’s team say the findings warrant further investigation and clinical testing for the treatment of CD20-expressing B cell malignancies.
Emily Hoggar, Cancer Research UK’s science communication manager, agrees. “More research is needed to understand the possible benefits and side effects, because we don’t know how the antibody will work in patients,” she says. Finding ways to turn the immune system on cancer is a fascinating area of research, she adds. “We’re learning more all the time about how to harness this power, but there are challenges ahead.”
Bispecific antibodies have been generating much interest since catumaxomab (Removab) was approved in Europe in 2009. Catumaxomab is a monoclonal antibody that binds to both the T-cell target recognised by CD20-TDB (CD3) and EpCAM, which is found in high levels on some types of cancer cell.
The financial website Marketwatch, published by Dow Jones & Co, estimates that, by 2024, the bispecific antibody market will be worth US$5.8bn annually. Marketwatch identified 37 bispecific antibody molecules currently in different stages of clinical development, of which eight or nine are expected to be launched by 2024.
References
[1] Sun LL, Ellerman D, Mathieu M et al. Anti-CD20/CD3 T cell–dependent bispecific antibody for the treatment of B cell malignancies. Science Translational Medicine 2015;7(287):287ra70. doi:10.1126/scitranslmed.aaa4802.

