BSIP SA / Alamy
Treatment perceived to be expensive, even though it was a placebo, led to a two-fold improvement in motor function in Parkinson’s disease (PD) patients compared with a treatment perceived to be cheap, according to research published in Neurology
[1]
on 28 January 2015. Brain activity in these patients also followed a corresponding pattern.
Alberto J. Espay, associate professor of neurology at the University of Cincinnati and lead author of the study, believes that clinicians should harness the placebo response to maximise the benefits of treatment, and even reduce the dosage, potentially reducing side effects.
“Physicians may play a vital role in this process by increasing the value of medications beyond just their pharmacological actions,” he says.
In the double-blind, randomised study, which started in 2009 and concluded two years later, Espay’s team told 12 participants — all of whom were patients at his clinic at the Gardner Center for Parkinson’s Disease and Movement Disorders — that they would receive injections of two formulations of a novel dopamine agonist, the second one administered after the first one wore off.
The study’s goal was to learn whether patients’ perception of the cost of the drug would affect the placebo response. “We described the first drug as being produced according to the original manufacturing process, which made it more expensive at a cost per dose of US$1,500, and the second one as being produced according to a streamlined system, which made it cheaper, at a cost per dose of $100,” says Espay. “The rationale, as told to the participants, was that both drugs were equally effective, but one was less expensive. In fact, both drugs were placebo saline injections, which was information withheld from the participants.”
At the beginning of the study, all patients also received levodopa, the standard drug treatment for PD, which allowed the researchers not only to compare patients’ reaction to the ‘cheaper’ versus ‘expensive’ placebos, but also to see how the placebos fared in comparison with levodopa.
Before and after each injection, participants took several tests that measured motor skills. When patients received the ‘expensive’ drug first, their motor skills improved by 28% (P=0.007), an effect not significantly different from that of levodopa. On one particular test, people’s scores improved by seven points when taking the ‘expensive’ drug first, but by only three points when taking the ‘cheap’ drug first.
“When patients believed that a drug was going to work well for them, that drug worked nearly the same as levodopa,” says Espay.
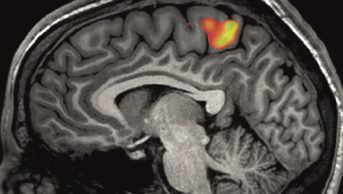
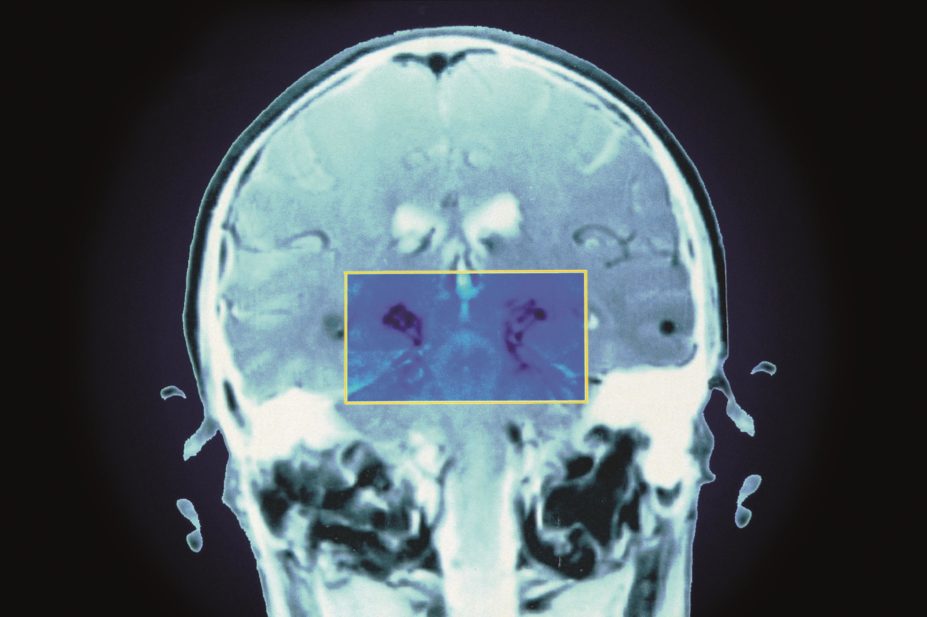
Patients’ brain activity was also assessed by functional magnetic resonance imaging (fMRI) brain activation analysis involving a feedback-based, visual-motor associative learning task.
The results of the learning task were intriguing. Performing the task after levodopa treatment led to deactivation in several left-brain areas, says Espay, but more regional brain activation occurred after administration of the ‘cheap’ placebo.
“We believe that this greater brain activity had to do with the patient perhaps trying to trick himself into believing the drug was working, and which may have required greater effort,” he says.
After the study, the 12 participants were told about the goal of the study and the deception by using placebos. Four of the patients said they had no expectation that the more ‘expensive’ drug would yield greater benefits, and for these patients the positive effects were indeed reduced.
Espay believes that clinicians can enhance the benefits of treatment through their interactions with patients. Instead of saying, “Here are the medications, let’s see what happens,” he suggests prescribers could say, “Here’s a medication — most people have a fantastic response to it, and chances are you will, too.”
In that way, he says, as well as the pharmacological benefit, prescribers can help patients benefit from a heightened expectation of efficacy through the placebo effect.