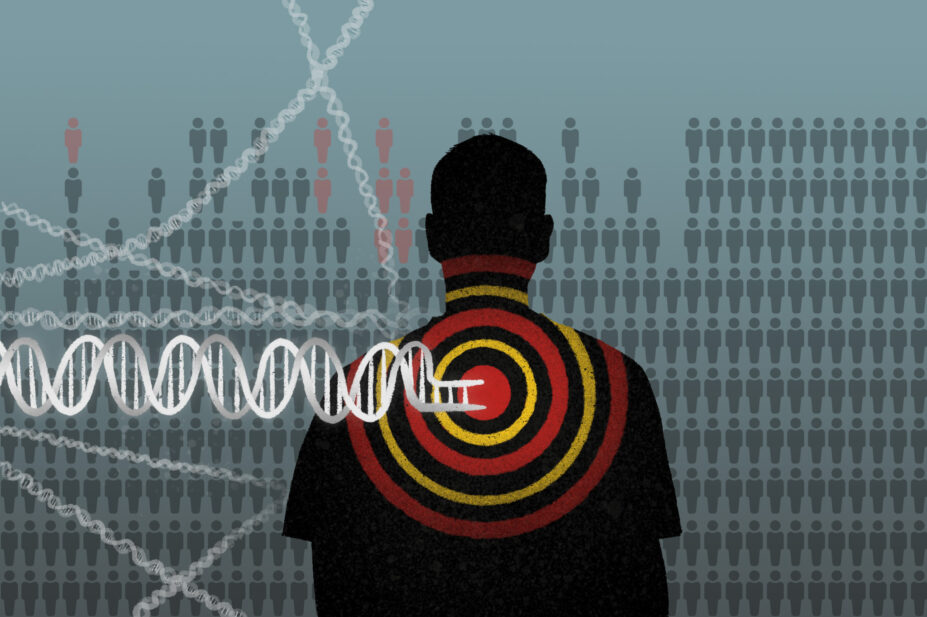
Wes Mountain/The Pharmaceutical Journal
In August 2022, I wrote about how patients described pharmacogenomics as something out of the realms of science fiction: the ability to look at someone’s DNA and predict drug efficacy and the likelihood of side effects. At the time, NHS Tayside was the first NHS trust in the UK to offer CYP2C19 genotype testing to guide clopidogrel prescribing in stroke patients. For most pharmacists, the reality of pharmacogenomics in daily practice seemed far in the distance.
But pharmacogenomics is gaining momentum. The ‘PREPARE’ study — a large European, multicentre cluster-randomised study, results of which were published in 2023 — gave us a glimpse into the tremendous potential pharmacogenomics holds in preventing adverse drug reactions. The ‘PROGRESS’ project, which is being carried out in the north of England, is currently introducing pharmacogenomics into primary care and the four UK nations have published or are developing genomic strategies signalling their intent to make the regular use of pharmacogenomics a reality.
The National Institute for Health and Care Excellence has now issued guidance calling for the national implementation of pharmacogenomics in acute stroke care when prescribing clopidogrel. Soon, local innovation will become national standard of care and, across the multiple areas of pharmacy practice, pharmacists — as the experts in medicines — will be called upon to interpret, support and lead in the development and implementation of pharmacogenomics in their clinical practice.
We have now been using pharmacogenomics in the management of stroke patients for over two years and can happily report that this implementation has been well received by both clinicians and patients alike.
Throughout the implementation, open dialogue was kept between pharmacists, clinicians and the laboratory; and the ordering and reporting processes streamlined
As a specialist pharmacist in stroke at Ninewells Hospital in Dundee, Scotland, I worked with Alex Doney, clinical reader in cardiovascular research at the University of Dundee, and David Baty, head of laboratory at East of Scotland Regional Genetic Service, Dundee Clinical Forum to develop and implement the NHS Tayside project to genotype acute stroke patients with an indication for clopidogrel.
This involved developing a Taqman-based assay for relevant CYP2C19 variants (*2 *3 and *17) to NHS genetics laboratory standards. A clinical pathway was implemented for requesting tests at diagnosis of non-cardioembolic ischaemic cerebrovascular events, as well as follow-up reporting and communication with primary care. Some 98.9% of results were reported to the stroke team within one week. Aspirin, dipyridamole, ticagrelor or their combinations were prescribed for individuals identified as impaired clopidogrel metabolism.
Between April 2022 and March 2024, the stroke service identified and tested 2,300 patients and found that 29% of those tested were poor or intermediate CYP2C19-clopidogrel metabolisers who should — following international guidelines — be prescribed an alternative antiplatelet for secondary prevention of stroke. Our results were in line with published prevalence figures for loss of function variants in a predominantly white European population, such as the one of Tayside.
Successful elements in our implementation included engaging with senior stroke clinical decision makers early on with one clear message: the implementation of pharmacogenomic testing is an additional tool being offered to them to improve patient safety and care, it should not be seen as an additional task being asked of them and their already stretched resources.
It was also critical to understand the existing stroke pathways, so the introduction of the new genotyping testing pathway could be incorporated as seamlessly as possible into the existing workstream with minimal impact on clinician workload. Throughout the implementation, open dialogue was kept between pharmacists, clinicians and the laboratory; and the ordering and reporting processes streamlined.
The stroke pharmacist led awareness sessions that were developed and delivered in-person and online, targeting primary and secondary care healthcare professionals as well as community pharmacy teams. Even though the genotyping only takes place in hospital, these sessions were important to ensure effective transfer of care, and so that healthcare professionals were informed along the different stages of care. Additionally, ongoing formal and informal training was provided to new medical staff joining the stroke service, particularly junior doctors and pharmacists during their rotations.
To ensure fast and effective uptake of this new genomic test, a ward pharmacist acted as a pharmacogenomic champion, identifying patients, ordering tests and communicating with patients and the medical team on a daily basis. The genomic test was easy to order, with the results reported back as a dichotomic action — either ‘appropriate to use clopidogrel’ or ‘choose an alternative to clopidogrel’ — allowing simple interpretation by clinicians when prescribing antiplatelets.
From the outset, it was anticipated that one of the main challenges in using pharmacogenomic data would relate to information technologies. Despite the successful and easy to interpret genotyping report used in this initiative, there is still a need for linked electronic records and integrated digital prescribing decision making tools to support clinicians. With the evolution of pharmacogenomics, more genomic information will become available, leading to greater complexity of interpretation and use in prescribing decision making. There is, therefore, an opportunity for information technology developments to support this field as well as the flow of information between healthcare settings.
The inability to integrate the genotyping results into different electronic systems in a usable way was also a challenge. It is important that clinicians can easily identify those patients that have been identified with CYP2C19 loss of function variants. As an interim measure, in addition to copying the full report to the patient’s medical record, it was also requested that primary care professionals record the loss of function as an allergy to clopidogrel with a descriptive entry.
Lessons from our pharmacogenomic implementation in NHS Tayside taught us that multidisciplinary work, open communication, education and awareness are crucial to a successful implementation. Pharmacists, as experts in medicines, are ideally placed to lead this evolution in how we approach prescribing of medicines with established pharmacogenomic guidance.
You may also be interested in

More than 2,000 patients tested in UK’s first routine genotyping project for clopidogrel prescribing

PJ view: Current testing for genetic variants risks undoing years of progress on health inequalities
