This content was published in 2012.
We do not recommend that you make any clinical decisions based on this information without first ensuring you have checked the latest guidance.
An update to this article was published in 2018 and can be found here.
Postoperative nausea and vomiting (PONV) is a common concern for patients undergoing surgery[1]. Despite attempts to reduce it, the incidence of PONV remains roughly 25%[2].
Hospitals that consistently achieve levels significantly below 25% without having implemented an adequate PONV policy should ensure that they are recording the incidence of PONV thoroughly — from recovery through to discharge. Where patients are discharged promptly following their procedure (e.g., in day-case surgery), consideration should be given to auditing PONV levels for patients after they have returned home. PONV policies should include (as a minimum):
- Risk scoring;
- Combination antiemetic prophylaxis;
- How to treat established PONV;
- Other mechanisms to reduce risk.
Risk scoring
The simplest and most widely used system for assessing a patient’s risk of experiencing PONV is the modified Apfel score (see Box)[3]. Other risk-scoring systems are available but they tend to be complicated and better suited to research.
Box. Modified Apfel score
The modified Apfel score is used to assess patients’ risk of postoperative nausea and vomiting (PONV). One point is allocated to patients for each of the four following risk factors:
- Female
- Non-smoker
- Use of postoperative opioids
- Previous history of PONV or motion sickness[3].
A patient’s score is then used to determine his or her likelihood of developing PONV, as follows:
Score (Risk of PONV)
- 0 (10%)
- 1 (20%)
- 2 (40%)
- 3 (60%)
- 4 (80%)
Apfel recommends that anyone with two or more risk factors should receive prophylactic antiemetics.
Antiemetic prophylaxis
Despite the relatively widespread adoption of the modified Apfel score, uncertainty remains over the most effective prophylactic antiemetic regimen as well as the identification of those patients who should be given prophylaxis.
IMPACT
The landmark IMPACT study involved over 4,000 high-risk patients (i.e., Apfel score of 2 or higher) and demonstrated the effect of six interventions (including three different intravenous antiemetics)[4]. It showed no statistical difference between any of the antiemetics tested or, indeed, any pair of antiemetics. Results showed that ondansetron, dexamethasone and droperidol all individually reduced the incidence of PONV by around 26%. Adding a second agent reduced the incidence by a further 26% (and, indeed, a third agent generated a further 26% reduction).
It is likely that other evidence-based antiemetics (e.g., cyclizine) would have a similar efficacy. Haloperidol has been used at a dose of 0.5–1mg as an alternative to droperidol. The take-home message from IMPACT is that it does not matter which antiemetic is used for PONV prophylaxis; rather, it is the number of antiemetics administered that is important. In any case, metoclopramide 10mg is ineffective forprophylaxis[5] and should not be included in guidelines.
As with all treatments, benefits should be weighed against potential risks. Nevertheless, it may be appropriate to consider antiemetic prophylaxis for all patients — even those at low risk of PONV.
A working example
At Doncaster and Bassetlaw Hospitals NHS Foundation Trust, all patients receive prophylaxis with ondansetron (given its low cost and low potential for adverse effects or interactions). Those with a modified Apfel score of 2 or more receive a combination of antiemetics (usually ondansetron plus dexamethasone).
Timing of antiemetics
Most prophylactic antiemetics should be administered intravenously 20 to 30 minutes before the planned end of surgery to achieve optimal effect. Dexamethasone should be administered shortly after induction. Also, since its administration is associated with perianal pruritus, dexamethasone should not be administered to conscious patients (although this effect might be reduced by diluting the drug with 50ml of sodium chloride 0.9% or glucose 5% and administering over 5–10 minutes).
Treatment of PONV
There is a paucity of evidence to guide the management of established PONV that occurs despite the use of antiemetic prophylaxis. In a systematic review of patients with established postoperativevomiting,6single doses of dolasetron (12.5–100mg), granisetron (0.1–3mg), tropisetron (0.5–5mg) and ondansetron (1–8mg) were shown to prevent further vomiting with no evidence of a clinically relevant dose response, suggesting that the lowest possible dose should be effective. The effects on nausea were less marked. Data supporting the use of other medicines are lacking.
Consensus guidelines suggest that established PONV should be treated with an antiemetic that acts on a different receptor to that used for prophylaxis(repeated administration of the same treatment should only be undertaken after six hours has elapsed)[2]. This appears to be rational: ondansetron has been shown to be ineffective for treating established PONV where it has already been used for prophylaxis[7].
If antiemetics are administered without effect, and medical causes of nausea and vomiting have been excluded, prescribers should seek specialist advice (from the acute pain or anaesthetic teams). Some centres suggest the use of combination treatment for established PONV. Although this approach might seem reasonable, supporting evidence is limited[8].
Other ways to reduce risks
In the IMPACT study, the combination of using propofol and avoiding nitrous oxide (known as “total intravenous anaesthesia”) reduced the incidence of PONV similarly to using a single antiemetic[4]. Other ways to minimise PONV include:
- Using regional anaesthesia (rather than general anaesthesia);
- Avoiding reversal of neuromuscular blockade with neostigmine (or keeping its dose below 2.5mg);
- Keeping patients well hydrated, well oxygenated and normotensive;
- Using low doses of opioids.
Acupuncture
Stimulation of the P6 acupuncture point (located on the wrist) is effective for preventing early PONV (i.e., 0–6 hours after surgery) in adults, with numbers needed to treat of about four[9]. However, it has demonstrated no benefit for children or in late vomiting (i.e., up to 48 hours post surgery). Rather than advocating that this technique be used routinely, a more targeted approach would be to recommend it adjunctively for patients who have used it successfully in the past to manage nausea and vomiting (e.g., for travel sickness).
Implementing PONV policies
The Royal College of Anaesthetists suggests that there should be a local policy for PONV and provides audit standards. It should be noted, however, that some of these standards (in particular those relating to appropriate use of 5HT3 antagonists and not providing prophylaxis for low-risk patients) may be outdated — an update is planned for 2012.
Irrespective of the contents of a PONV policy (and the antiemetics selected), the act of implementing such a policy has been shown to reduce the incidence of PONV[10]. In one study, a hospital using an aggressive prophylactic approach achieved considerable reductions in PONV rates for those undergoing day surgery[11].
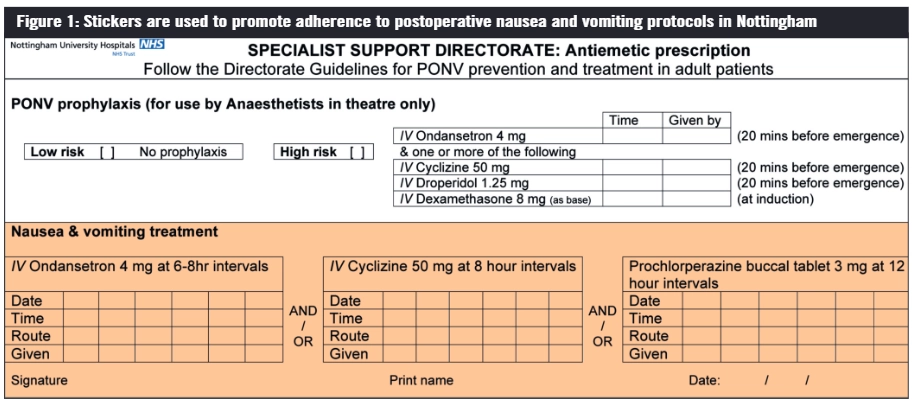
Documenting when PONV occurs is helpful for auditing and highlighting issues. Recording on observation charts focuses clinicians’ attention on PONV and, when combined with guidelines for management, should promote prompt treatment. At Nottingham University Hospitals NHS Trust, a sticker (see Figure 1) is attached to the drug chart to promote adherence with local guidance.
Future developments
PONV remains a considerable clinical challenge. New antiemetics continue to be developed (e.g., aprepitant, palonosetron, rolapitant) but these medicines offer only modest advantages over other widely available and less expensive therapies. Glass and White stated in a 2007 editorial: “Given the high efficacy, low cost and excellent safety profiles of the most commonly used antiemetic drugs (e.g., droperidol, dexamethasone and ondansetron), in our view these drugs should be routinely administered for antiemetic prophylaxis of all patients receiving general anaesthesia irrespective of their risk classification”[12].
Summary
Postoperative nausea and vomiting (PONV) is common — it affects about 25% of patients who undergo surgery. Hospitals, therefore, should implement policies to tackle PONV.
Such policies should include a scoring system to assess patients’ risk of PONV and treatment algorithms for the prophylaxis and treatment of PONV.
References
- Macario A, Weinger M, Carney S. Which clinical anaesthesia outcomes areimportant to avoid? The perspective of patients. Anaesthesia and Analgesia 1999;89:652–8.
- Gan TJ, Meyer TA, Apfel CC, et al. Society for Ambulatory Anaesthesia guidelines for the management of postoperative nausea and vomiting. Anaesthesia and Analgesia 2007;105:1615–28.
- Apfel CC, Laara E, Koivuranta M, et al. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology 1999;91:693–700.
- Apfel CC, Korttila K, Abdalla M, et al. (for the IMPACT investigators). A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. New England Journal of Medicine 2004;350:2441–51.
- Henzi L, Walder B, Tramer MR. Metoclopramide in the prevention of postoperative nausea and vomiting: a quantitative systematic review of randomized placebo-controlled studies. British Journal of Anaesthesia 1999;85;761–71.
- Kazami-Kjellberg F, Henzi I, Tramer M. Treatment of established postoperativenausea and vomiting: a quantitative systematic review. BMC Anesthesiology 2001;1:2.
- Kovac AL, O’Connor TA, Pearman MH, et al. Efficacy of repeat intravenous dosing of ondansetron in controlling postoperative nausea and vomiting: a randomized, double-blind, placebo-controlled multicentre trial — effect on outcome. Journal of Clinical Anaesthesia 1999;11:453–9.
- Rüsch D, Arndt C, Martin H, et al. The addition of dexamethasone to dolasetron orhaloperidol for treatment of established postoperative nausea and vomiting. Anaesthesia 2007;62:810–7.
- Lee A and Done ML. The use of nonpharmacological techniques to prevent postoperative nausea and vomiting: a meta-analysis. Anaesthesia and Analgesia 1999;88:1362–9.
- Hadji F, Eastwood D, Fear S, et al. The impact of audit in a district general hospital on post-operative nausea and vomiting after major gynaecological surgery. European Journal of Anaesthesiology 1998;15:595–9.
- Williams BA, Kentor ML, Skledar SJ, et al. Routine multimodal antiemesis including low-dose perphenazine in an ambulatory surgery unit of a university hospital: a 10-year history. Scientific World Journal 2007;7:978–86.
- Glass PSA, White PJ. Practice guidelines for the management of postoperative nausea and vomiting: past, present, and future [editorial]. Anaesthesia and Analgesia 2007;105:1528–9.


