
Photofusion Picture Library / Alamy
Medicines optimisation could revolutionise medicines use and outcomes, according to Sir Bruce Keogh, NHS England medical director.
This endorsement came in May 2013, when the Royal Pharmaceutical Society (RPS) published four guiding principles for the concept within its report, ‘Medicines Optimisation: helping patients to make the most of medicines’. It was backed by NHS England, the Royal College of General Practitioners, the Royal College of Nursing, the Academy of Royal Colleges and the Association of the British Pharmaceutical Industry (ABPI).
Twenty months on, this concept is gaining traction among healthcare professionals, even if the core message is not yet universally recognised.
Medicines optimisation has its critics. Some believe it is medicines management rehashed; others view it as government jargon that is incomprehensible to patients.
Its proponents, however, see a chance to ensure patients get the right medicine at the right time while refocusing on the patient experience of care — an opportunity to improve patient outcomes, help them to take appropriate medicines correctly and safely, and to reduce waste.
Heidi Wright, English practice and policy lead at the RPS, says medicines optimisation needs to be better understood across the health service. “I think pharmacy is getting it, although I wouldn’t say all pharmacists get it,” she says. “They’re starting to understand the concept of medicines optimisation, invest to save and the focus on the patient’s involvement in decisions about their medicines.”
Anne Cole, regional manager South West for the Centre for Pharmacy Postgraduate Education (CPPE), whose programmes are designed to support the medicines optimisation agenda, says: “We’ve still got a lot of work to do if we want to embed it in the profession. People have heard about it but are not sure they understand it.”
The four RPS principles are to understand the patient’s experience of care; to choose medicines on the best available evidence; to ensure medicines are used as safely as possible; and to instil these aims in routine practice.
“I certainly wouldn’t say pharmacists and pharmacy technicians are not doing [these] already, but it provides them with a framework,” says Cole.
She believes medicines optimisation is now essential for the health service. “The two main issues are to improve outcomes for patients and reduce wastage,” she says. “We know that millions of pounds are wasted each year on medicines which are not used as intended, intentionally or unintentionally. It is for pharmacy to work with patients and other healthcare professionals to improve that situation.”
In early 2014, the RPS published four briefings in collaboration with the CPPE, showing how the principles could be applied to asthma, cardiovascular disease, type 2 diabetes and schizophrenia.
Now, the RPS and CPPE are publishing a further four — on rheumatoid arthritis, epilepsy, depression and acute kidney injury (see ‘Medicines optimisation briefings’).
Wright says the briefings illustrate the core concepts of medicines optimisation with practical examples, and will help pharmacists who are managing patients with these conditions — particularly in medicines use reviews and the new medicines service.
“It’s not just about making sure you get the right medicines for the right patient, it’s about how you then support the patient to take the medicine, or otherwise if the patient decides not to take it,” she says. “It’s about having grown-up conversations, shared decision-making.”
Health organisations plan to ramp up the medicines optimisation drive in 2015.
A medicines optimisation steering group, led by NHS England and the ABPI, has been established, and is working to implement the RPS principles in practice.
Meanwhile, Academic Health Science Networks across England are hosting a series of 15 roadshows, starting in London on 3 March 2015.
The second version of NHS England’s medicines optimisation dashboard — a digital resource that uses metrics to benchmark local performance — is due to be launched in early 2015. The prototype, published in June 2014, encouraged clinical commissioning groups and trusts to consider how patients are supported in their use of medicines, instead of focusing on cost and volume.
This area of work is gathering pace. Medicines optimisation has been a slow burner so far, but pharmacists should expect to hear much more in 2015.
Medicines optimisation briefings
Source: Royal Pharmaceutical Society (RPS)
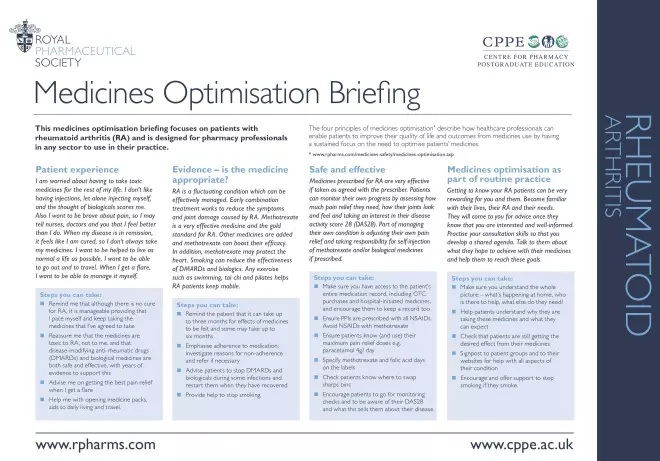
The Royal Pharmaceutical Society (RPS) and the Centre for Pharmacy Postgraduate Education (CPPE) have produced four medicines optimisation briefings to assist pharmacy professionals. These include worked examples of how to manage four conditions in line with the RPS principles.
The first, on rheumatoid arthritis, covers advice including reassuring patients that rheumatoid arthritis medicines are safe and effective; emphasising the importance of medicines adherence; and helping patients to understand why they’re taking the medicines.
This briefing appears as an insert with the 17 January 2014 issue of The Pharmaceutical Journal. Briefings on epilepsy, depression and acute kidney injury will follow on alternate weeks. All will be available on the RPS and CPPE websites.
In addition, CPPE’s regular ‘e-challenge’ quiz (www.cppe.ac.uk/e-challenge) will contain questions relating to the briefings over the coming weeks.

