Charles Shearn
The role of the pharmacy technician continues to evolve. Many are taking on patient facing roles and it is not unheard of for some, at least in the hospital sector, to be managing their pharmacist colleagues.
At a conference in 2015, Keith Ridge, the chief pharmaceutical officer for NHS England, hinted that it would only be a matter of time before pharmacy technicians were managing community pharmacies to free pharmacists’ time for clinical activities[1]
. And a decade earlier, in what was effectively Ridge’s inaugural speech as England’s most senior pharmacist, he called on pharmacists and pharmacy technicians to work more closely to address deficiencies in patients’ experiences of the health service[2]
.
Since that speech, pharmacy technicians have become registered healthcare professionals. Registration with the General Pharmaceutical Council (GPhC) became compulsory on 1 July 2011 (a voluntary system operated from 2005) and there are now around 23,000 technicians on the register, compared with 52,000 pharmacists.
The initial education and training of pharmacy technicians is vocational and is completed through simultaneous part-time study and employment. Two qualifications are required: a knowledge-based qualification and a competence-based one. These qualifications, which can be taken simultaneously or consecutively, are generally taught face to face, mainly in further education colleges and NHS trusts or health boards, but others are delivered at a distance. Training usually takes two years and accredited qualifications include the BTEC National Diploma in pharmaceutical science; an NVQ/SVQ level 3 in pharmacy services; or the National Certificate in pharmaceutical science. Courses cover human physiology, disease management, actions and uses of medicines, pharmacy manufacturing and pharmacy law.
Like pharmacists, pharmacy technicians have to keep their skills and knowledge up to date with a minimum of nine continuing professional development (CPD) entries each year.
What a pharmacy technician does depends on who you ask and where they work. Technicians prepare, dispense, supply and issue medicines to patients but they are involved in a range of areas, including clinical, operational and management roles. Typical duties include medicines reconciliation, advising patients about medicines on discharge or at the counter, and procuring medicines stock. But these tasks can vary depending on the particular trust or hospital, as well as whether the technician is based in community or hospital pharmacy.
If pharmacists continue to expand their clinical role, in whichever sector they work, then it is logical that they will require more support in fulfilling their existing duties. Indeed, this has happened already; pharmacy technicians are taking on a growing number of tasks that were traditionally the preserve of pharmacists.

Source: General Pharmaceutical Council (GPhC)
It is not for the GPhC to define the role of pharmacy technicians in such a narrow way as to limit their responsibilities, says Duncan Rudkin, chief executive of the GPhC
And it seems the GPhC, the regulator of both pharmacists and pharmacy technicians, has no intention of trying to restrict what pharmacy technicians can do.
“The role of pharmacy technicians is likely to continue to change as pharmacy and healthcare delivery in each of the three countries of Great Britain continues to change. It is not for us as the regulator to define their role in such a narrow way as to limit their responsibilities,” says Duncan Rudkin, chief executive of the GPhC. “It is, however, our responsibility to listen to governments across Great Britain, to the NHS and other employers, to registrants and to patients about how pharmacy and the roles of pharmacy professionals are changing.”
Growing responsibilities
Michelle Sullivan, a pharmacy technician who leads medicines management for cardiac patients at Barts Health NHS Trust in London, says that in her team, pharmacy technicians are largely patient-facing and work in clinical areas to help facilitate early diagnosis and prevent missed doses of medicines.
Many of the operational tasks that Sullivan now carries out were handled by pharmacists in the past, and the rest of the team is also taking on duties previously carried out by pharmacists, including managing patient databases for hospital prescriptions and medicines reconciliation.
“Pharmacists and pharmacy technicians have very different roles but the set-up we have instilled within the cardiac team allows the pharmacists to support the clinical roles and the pharmacy technicians [to support] the technical and operational roles on a broader basis,” Sullivan says.
Counselling patients and things like that are all normally pharmacist jobs that now can be taken over by technicians, which then allows the pharmacist to take on more clinical roles
Kieran Casey-McEvoy, a senior pharmacy technician at King’s College Hospital, London, says the way that most hospital pharmacies operate in terms of dispensing, storage and the clinical team’s work is probably quite standard from trust to trust. But where he works, pharmacy technicians are increasingly taking on tasks that historically were done by the pharmacist, as exemplified by the emergence of the checking technician.

Source: Courtesy of Kieran Casey-McEvoy
The role of pharmacy technicians is highly dependent on location, even within the hospital sector, says Kieran Casey-McEvoy, a senior pharmacy technician at King’s College Hospital, London
“Checking a prescription before it was given out was typically a pharmacist job,” says Casey-McEvoy, who is also media officer at the Association of Pharmacy Technicians UK (APTUK), the professional leadership body for pharmacy technicians. “Counselling patients and things like that are all normally pharmacist jobs that now can be taken over by technicians, which then allows the pharmacist to go and do ward rounds, be in clinics and take on more clinical roles.”
But he adds that the role of pharmacy technicians is highly dependent on location, even within the hospital sector.
“Different trusts do things differently,” he says. In his previous role at the Whittington Health NHS Trust, London, he worked alongside the district nursing team to administer medicines to patients in the community. But this might be the only trust in the country to do this, he says.
“It is quite an unusual role, it’s not the typical technician role,” he says. “I’ve come across technicians who will visit patients at home to deal with compliance, but never to actually do the administration.”
Sullivan believes that pharmacy technicians could do more to ease pressure on busy wards. “It could be standard practice for the pharmacy technicians to support the administration of medicines,” she says. “We know nursing recruitment and retention is hard in the NHS and as pharmacy technicians we could support a medication round for the patients.”
Such a supporting role has been evaluated by researchers at Birmingham Children’s Hospital. Chief pharmacist Anthony Sinclair and colleagues examined whether pharmacy technicians could support the workload of nurses on one of the hospital’s haematology oncology wards. Three pharmacy technicians were trained and assisted in the preparation and administration of intravenous injections. The researchers reported a reduction in adverse events of one to two per day during the study period, a reduction in nurse work-related stress associated with preparing complex medicines, and the release of four hours of nursing time per day[3]
.
Sullivan also suggests that, in specialist centres, it would be possible to implement pharmacy technician-led clinics, such as for asthma reviews or referrals, warfarin clinics, pre-admission clinics, first-cycle chemotherapy counselling or diabetic clinics. “Nurses lead on these so why not a pharmacy technician?”
The variety seen within pharmacy technician roles goes some way to explaining the uncertainty around what technicians do and how their roles are evolving. At the 2015 conference attended by Ridge, Rudkin remarked that he had been shocked to meet several pharmacists who did not know what the role of the pharmacy technician involved[1]
.
But, according to Alice Llewellyn, a pharmacy technician at Banwell Village Pharmacy near Bristol, those pharmacists could be forgiven.
“I can understand why some wouldn’t [understand the role], as I don’t believe there are any clear definitions and tasks specifically centred for technicians at the moment,” says Llewellyn. “Many tasks I do haven’t changed from when I was a dispenser to being a technician, even though my knowledge has greatly improved.”
The need to distinguish between the role of the dispensing assistant and the pharmacy technician was also identified in responses[4]
to a discussion paper, ‘Tomorrow’s pharmacy team; future standards for the initial education and training of pharmacists, pharmacy technicians and pharmacy support staff’[5]
, published by the GPhC in June 2015.
Community developments
At Banwell Village Pharmacy, the technicians are involved in ordering stock, labelling and dispensing prescriptions, dispensing dosette boxes, and counselling patients on prescribed medicines, including offering advice on inhaler technique and some over-the-counter (OTC) items.
But there is still capacity for technicians to take on new responsibilities. Llewellyn suggests that community pharmacy technicians could be involved in providing emergency hormonal contraception or the OTC medicine azithromycin to treat chlamydia. “We could do the initial chat with the patient and then dispense and get the item checked by the pharmacist.”

Courtesy of Banwell Village Pharmacy
Alice Llewellyn (left), a pharmacy technician at Banwell Village Pharmacy, with superintendent pharmacist Margaret Hook (right)
She also suggests that pharmacy technicians could be involved in delivering the new medicine service (NMS) – a scheme run in England to provide private consultations with a pharmacist to discuss recently prescribed medicines.
This suggestion has the support of Llewellyn’s superintendent pharmacist Margaret Hook. Operating in a tiny pharmacy in a village location, Hook takes advantage of her pharmacy technicians’ skills, as well as employing two additional pharmacists, to allow her to provide a more personal service to local residents.
Hook believes technicians are qualified to provide more patient-facing services, such as delivering initial advice as part of the NMS. And if an appropriate standard operating procedure were in place, technicians could also be responsible for the NMS for specific drugs.
“The course [undertaken by pharmacy technicians] is unbelievably in depth across the therapeutic areas,” she explains. “If they are up-to-date and they’ve done training that we’ve designed for them, [then they should] be fully abreast of all of the things that we would explain.”

Source: APTUK
Tess Fenn, president of APTUK, says that she can see pharmacy technicians doing medicines use reviews in community pharmacy for less complex patients and referring patients to the pharmacist when necessary
Tess Fenn, president of APTUK, also says that she can see pharmacy technicians doing medicines use reviews (MURs) in community pharmacy for less complex patients and referring patients to the pharmacist when necessary. Some of the skills involved in medicines reconciliation, which many pharmacy technicians already do on hospital wards, are the same ones needed to do an MUR, she argues.
“It’s about working in that supportive team, and within the governance arrangements, and being aware of what you can and what you can’t do in terms of your own knowledge and expertise,” says Fenn.
It is not clear how much the role of pharmacy technicians has already evolved or will evolve within larger pharmacy chains, which may not be open about their staffing strategies. The UK’s third largest pharmacy chain Well, formerly The Co-operative Pharmacy, is reviewing the descriptions of roles for pharmacy support staff.
We are conscious that the role they undertake is evolving to meet the changing needs of patients, the public and the NHS
“Pharmacy technicians play a key part in our pharmacy teams,” says Janice Perkins, the company’s superintendent pharmacist. “We are conscious that the role they undertake is evolving to meet the changing needs of patients, the public and the NHS. In light of this, we are reviewing our role descriptions and also how we train and support our technician workforce to ensure they are well placed to embrace these changes.”
The UK’s two largest pharmacy chains – Boots UK and Lloydspharmacy – chose not to discuss their plans for pharmacy technicians. However, in its response to the GPhC’s discussion paper on educating the pharmacy team[4]
, Boots UK’s parent company Boots Walgreens Alliance said: “The current role of pharmacy technicians, especially in community pharmacy, is around the technical assembly and preparation of medicines for dispensing, but we would expect them to move in to assisting with or providing more clinical services, especially as the automation of dispensing increases.”
Legal dilemmas
It seems the question is not whether the role of the pharmacy technician should change, but how.
This is currently a matter being debated in private by the Rebalancing Medicines Legislation and Pharmacy Regulation Board. The board – whose members include representatives from the UK’s four health departments, professional associations for both pharmacists and technicians, chief pharmacists and representatives from large community pharmacy chains – is looking at what is in the law at the moment and what could be changed to allow innovation and improvements in efficiency, while keeping patients safe.
The board has already looked at what happens when dispensing errors are made, with legislative changes expected to be laid before parliament in 2016, as well as the regulation of pharmacy premises. Their next task is supervision. In particular, whether any parts of the law currently “restrict full use of the skills of registered pharmacists and registered pharmacy technicians, impede the deployment of modern technologies and put disproportionate or unnecessary obstacles in the way of new models of service delivery by and/or involving pharmacy”.
Regulation 220 of the Human Medicines Regulations 2012 sets out the requirements for the lawful sale or supply of pharmacy and prescription medicines. In its responsible pharmacist guidance, the GPhC also sets out the level of supervision required for certain activities.
Although practice does vary, the legal position is clear, says Fenn: “The law is very clear at the moment that a registered pharmacist, as the responsible pharmacist, must be in charge of a registered pharmacy to allow pharmacy services to take place.”
Fenn insists that it is not about simply shifting the duties of a pharmacist over to the pharmacy technician, but is about delegation – pharmacy technicians will take on tasks requested by the pharmacist that they are competent to do.
“It’s about looking at the whole team, at the pharmacy services that the pharmacy needs to provide to meet the needs of the public, within the current healthcare environment that’s extremely challenged at the moment,” says Fenn.
The responsible pharmacist is ultimately in charge of the safe and legal operation of the pharmacy and can choose to utilise the skills of the team, according to their training level, she argues.
“It is looking at who have we got in the pharmacy team, looking at their knowledge, skills and behaviours, looking at who is best placed at any one time to actually provide the services that are required.”
Training reviews
The GPhC is currently reviewing the initial education and standards for pharmacy technicians with a consultation planned for 2016. Once the standards have been signed off, they will be used to develop new qualifications for pharmacy technicians, incorporating the national occupational standards that were updated by Skills for Health, an organisation that works across the UK health sector to maximise the potential of the workforce, earlier in 2016[6]
.
It is more important to teach the future workforce to be flexible enough to respond effectively to the unpredictability of changing roles and settings of practice
Training and standards need to reflect the larger role that technicians are playing in the pharmacy team, says the GPhC. But there is difficulty in predicting the knowledge and skills that will be needed down the line, adds Rudkin.
“It is more important to teach the future workforce to be flexible enough to respond effectively to the unpredictability of changing roles and settings of practice. Education and training therefore need to be ongoing processes beyond qualification.”

Source: Courtesy of Alpana Mair
Alpana Mair, deputy chief pharmaceutical officer for Scotland, says there needs to be a career framework for pharmacy technicians
In Scotland, the ten-year ‘Prescription for excellence’ action plan, launched in September 2013, sets out a more clinical role for pharmacists. Alpana Mair, deputy chief pharmaceutical officer for Scotland, says there needs to be a career framework for pharmacy technicians as well as professional leadership support to enable them to take on new roles in the pharmacy team.
“In order to deliver the ambitions of ‘Prescription for excellence’ and the clinical patient facing role of the pharmacist, workforce development and planning will be essential to develop current and future pharmacy services,” says Mair. “A strong professional leadership body for technicians, such as APTUK, that will work in partnership with the Royal Pharmaceutical Society will be important.”
Underlying tension
Fenn believes many pharmacists are grateful and respectful of the role pharmacy technicians play. But she is also aware of a lack of understanding about the initial training that technicians receive, and also of the responsibilities they can take on since achieving professional status in 2011.
There is already room for autonomous working within the level 3 qualification that technicians must now achieve for entry on to the register, she points out.
Sullivan acknowledges that tensions could arise if pharmacists feel threatened by technicians taking on more clinical and managerial roles. “But I think this can be overcome by promoting a team approach to the overall tasks and the objectives,” she says.
At Barts Heart Centre at St Bartholomew’s Hospital, London, the lead pharmacy technician manages the pharmacy team, including pharmacists – something that Sullivan believes breaks an unwritten rule.
“There is a recognition by all staff, including the pharmacist, that we have the right set up in terms of a pharmacy technician operationally managing the team,” she says. “The senior level pharmacist team recognises the roles the pharmacy technicians are capable of now and are keen for that to be embedded.”
The team’s consultant pharmacist Sotiris Antoniou says their set up has worked, and could work elsewhere.
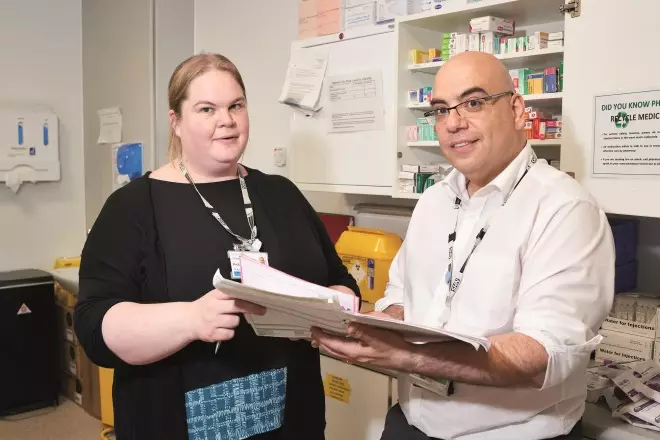
Source: Charles Shearn
Pharmacy technicians are integral to enabling developments such an independent pharmacist prescribing, says consultant pharmacist Sotiris Antoniou (right), pictured with Michelle Sullivan (left), a pharmacy technician at Barts Health NHS Trust in London
“Undoubtedly, some pharmacists may initially see this as an erosion of their responsibility, especially when roles that were traditionally carried out by them are being transferred. However, once they see how this enables them to apply their clinical expertise to the patient, they soon recognise the benefits it could have,” says Antoniou.
He adds that with initiatives such as independent prescribing extending the role of pharmacists, pharmacy technicians are integral to enabling these developments while maintaining the service still expected of pharmacy.
“As a clinical pharmacist, we must embrace this opportunity to maximise the care that pharmacy can provide to patients. Only by doing so, can we change the mindset to pharmacy being an essential service, as opposed to being a clinical support service.”
References
[1] Technicians will be managing pharmacies to free up pharmacists, suggests chief pharmaceutical officer. The Pharmaceutical Journal 2015;295:7883. doi: 10.1211/PJ.2015.20200078
[2] Pharmacists and technicians must work together closely. The Pharmaceutical Journal, 2006;276;432. URI: 10021535
[3] Sinclair A, Eyre C, Petts H et al. Introduction of pharmacy technicians onto a busy oncology ward as part of the nursing team. Eur J Hosp Pharm 2016. doi: 10.1136/ejhpharm-2016-000951
[4] Tomorrow’s pharmacy team — responses to the discussion paper. November 2015. General Pharmaceutical Council. Available at: https://www.pharmacyregulation.org/sites/default/files/report_on_educating_the_pharmacy_team.pdf (accessed 20 June 2016)
[5] Tomorrow’s pharmacy team: Future standards for the initial education and training of pharmacists, pharmacy technicians and pharmacy support staff. June 2015. General Pharmaceutical Council. Available at: http://www.pharmacyregulation.org/sites/default/files/tomorrows_pharmacy_team_june_2015.pdf (accessed 20 June 2016)
[6] Pharmacy National Occupational Standards Review. Context document and Signposting to NOS. February 2016. Skills for Health. Available at: http://www.skillsforhealth.org.uk/images/standards/nos/Pharmacy%20Context%20&%20Signposting%20document%20February%202016.pdf (accessed 20 June 2016)