Summit PLC
Antimicrobial resistance (AMR) — the ability of previously-sensitive microorganisms to resist the effects of an antimicrobial agent — is a growing problem. In 2014, the World Health Organization (WHO) warned that we could be moving into a post-antibiotic era where even minor injuries could lead to life-threatening infections. This could put the future of our whole healthcare system in jeopardy, putting an end to complex surgery and returning us to an era where childbirth is high-risk.
In June 2014, as a response to the enormous challenge of antimicrobial resistance, the UK government commissioned the economist Lord Jim O’Neill to chair the Review on Antimicrobial Resistance[1]
. Its aim was to analyse the problem and propose actions that could be deployed internationally. Lord O’Neill concluded that if the spread of AMR was not curtailed, the current 700,000 deaths a year that can be linked with AMR could rise to 10 million by 2050, and the loss of global production between 2016 and 2050 could top US$100 trillion.
He said: “It is now clear to me, as it has been to scientific experts for a long time, that tackling AMR is absolutely essential. It needs to be seen as the economic and security threat that it is, and be at the forefront of the minds of heads of state, finance ministers, agriculture ministers, and of course health ministers, for years to come.”

Courtesy of the Office of Lord Jim O’Neill
The UK government commissioned economist Lord Jim O’Neill to chair the Review on Antimicrobial Resistance (AMR), who said that AMR needed to be at the forefront of the minds of heads of state, finance ministers, agriculture ministers, and of course health ministers, for years to come
Reducing the threat of antimicrobial resistance is about both reducing unnecessary prescribing of antibiotics, and ensuring appropriate prescribing, where the right antibiotic is used against the right organism. Both of these can be tackled by the use of diagnostics — ideally to provide a differential diagnosis and suggest the best antibiotic to use. This approach is backed by the WHO, which has called for “diagnostic stewardship”, which it defines as “appropriate use of microbiological diagnostics to guide therapeutic decisions… [promoting] appropriate, timely diagnostic testing, including specimen collection, and pathogen identification and accurate, timely reporting of results to guide patient treatment”.
At an event hosted by the Westminster Health Forum that brought together health leaders from medicine, research, public health and politics in July 2017 — ‘Next steps for antimicrobials and combating antimicrobial resistance: funding research and clinical practice’ — Lord O’Neill said if he had to prioritise just one of the ten recommendations he had made in his review, it would be diagnostics.
“We discovered research evidence showing that perhaps as many as 50% of antibiotics prescribed are not necessary in Western countries alone. Therefore, the difference that using diagnostics could make is potentially huge,” he said.
Of the 27 AMR review proposals put forward, the one that Lord O’Neill described as the most “ambitious and aggressive” is the proposition that, by 2020, all developed economies should make it mandatory to use recognised diagnostic tests before antibiotics can be given. He sees this as important in unleashing bigger growth in the diagnostic research world.
“Another idea is to make diagnostics compulsory for anyone who needs last-in-line antibiotics for Gram-negative drugs in Western economies, and if biopharma companies want to charge higher prices for these drugs, they must pay for the diagnostics,” he added.
The history of AMR
AMR has a longer history than the modern use of penicillin and other drugs. Evidence of antibiotic resistance genes dates back to between 10,000 and 2 billion years ago, as a response to the naturally occurring antibiotics in the environment[2]
.
But Alexander Fleming was the first to warn about the risk of antibiotic resistance. In his Nobel Lecture in December 1945, he said: “I would like to sound one note of warning… It is not difficult to make microbes resistant to penicillin in the laboratory by exposing them to concentrations not sufficient to kill them, and the same thing has occasionally happened in the body. The time may come when penicillin can be bought by anyone in the shops. Then there is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non-lethal quantities of the drug, make them resistant”[3]
.
His concerns came to bear. Penicillin was first prescribed in the 1940s and signs of penicillin resistance were first seen as early as the 1950s. Since then, resistance has emerged to almost every class of antibiotics developed[4]
.
“Antibiotics are frequently prescribed ‘just in case’ because we lack the diagnostics that could reliably and quickly indicate whether someone has a virus or a bacterial infection,” said chief scientific officer Sue Hill of NHS England and chief pharmacist Keith Ridge in their report ‘Government response to the Review on Antimicrobial Resistance’, published in 2016[5]
.

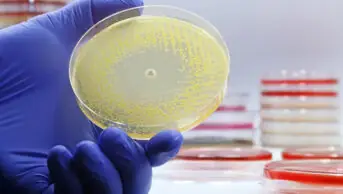
Source: Summit PLC
AMR has a longer history than the modern use of penicillin and other drugs. Evidence of antibiotic resistance genes dates back to between 10,000 and 2 billion years ago
Integrating diagnostics into healthcare
They added that the vision in England is for patient-centred, cost-effective diagnostics that help tackle AMR by ensuring the right test is available at the right place at the right time. One of the challenges, however, is going to be finding a way to integrate the diagnostics into the clinical pathway — for example, it may not be practical to ask patients attending a GP to wait for a prescription while the diagnostic is run, and individual small practices may not have the resources to do this.
The alternative approach, as put forward by chief medical officer Sally Davies at the Westminster Forum event in July, could be that a doctor deciding that the patient needs an anti-infective gives the patient a prescription to take to the pharmacy or walk-in centre, where the pharmacist, who deals with a number of GP practices and so has more of an economy of scale, uses point-of-care diagnostics to define the correct antibiotic. He or she then endorses the prescription and dispenses the most appropriate drug.
Source: Pacific Press / Alamy Stock Photo
The alternative approach to diagnostics in a GP surgery was proposed by chief medical officer Sally Davies at the Westminster Forum event in July. She suggested that a doctor deciding that the patient needs an anti-infective can give the patient a prescription to take to the pharmacy or walk-in centre, where the pharmacist, who deals with a number of GP practices and so has more of an economy of scale, can use point-of-care diagnostics to define the correct antibiotic
“Patients feel validated in their illness when they get an antibiotic, so a massive cultural change needs to take place that will be really difficult. Point of care testing would be a nirvana,” she said.
This route to diagnosis and treatment of bacterial infections could have a number of benefits. It might take the pressure off GPs, saving them time in individual appointments, as they could refer patients directly to pharmacists. It may integrate pharmacists more closely into patient care, perhaps encouraging patients to go directly to the pharmacist in future for minor ailments. It could also reduce the number of antibiotic prescriptions overall and, in the case of differential diagnoses, potentially shift appropriate prescribing from broad spectrum to narrow spectrum antibiotics for specific infections.
O’Neill is also a fan of the proposed model: “Could this work in practice? The simple answer is yes. In addition to improving the overuse of unnecessary antibiotics, it would probably play a useful role in reducing pressure on GPs’ time. This is another reason why the NHS should consider offering funding support for really effective technology at reasonable prices, as it could result in significant benefits.”
Growing the role of the pharmacist
The Community Pharmacy Forward View, published in 2016 by Pharmacy Voice and the Pharmaceutical Services Negotiating Committee and supported by the Royal Pharmaceutical Society English Pharmacy Board has supported the routine availability of point-of-care testing and diagnostics in pharmacy settings as a general concept[6]
. Pharmacists have also shown support for the idea of point-of-care diagnostics as part of a model where the pharmacist validates the prescription.
“The model reinforces the clinical skills of the pharmacist. Local pharmacies have a lot to offer with additional services like this and the profession could benefit from some out-of-the-box thinking generally,” said Phil Day, pharmacist at Pharmacy2U.

Source: Pharmacy2U
The Community Pharmacy Forward View supports the routine availability of point-of-care testing and diagnostics in pharmacy settings as a concept. Phil Day, at Pharmacy2U believes that the profession would benefit from using such additional skills of local pharmacists
It would require a careful look at funding, workload and governance, and would need to be backed up by solid evidence.
Matt Barclay, director of operations at Community Pharmacy Scotland, agrees: “The role of community pharmacy in antibiotic stewardship is important and this could potentially be another area where this impact could be demonstrated. If ultimately it helped inappropriate antibiotic use without having a detrimental effect on other outcomes, for example patient recovery rates or hospital admissions, then it could be considered.”
The evidence for this type of model would therefore have to be scoped and the governance arrangements between GP and CP would have to be worked through, he added.

Courtesy of Matt Barclay
Matt Barclay, director of operations at Community Pharmacy Scotland, believes that antimicrobial stewardship could potentially be another area where the impact of Community Pharmacy is demonstrated
The Royal Pharmaceutical Society is playing an important role in AMR and antimicrobial stewardship (AMS) by supporting pharmacists to educate patients and the general public on both appropriate and inappropriate use of antimicrobials.
Funding the diagnostics
The diagnostics approach can potentially reduce the levels of inappropriate prescribing, but the question of who will pay remains.
Davies raises this as a legitimate issue: “Point-of-care diagnostics have made a big difference in other fields,” she said. “But the unintended consequence is that antibiotics are very cheap generic drugs whereas a rapid diagnostic tends to be much more expensive, so how do we reconcile that disconnection?”
A position statement from the British In Vitro Diagnostic Association (BIVDA)[7]
calls for guidance for evidence requirements for the use of in vitro diagnostics to help companies developing these, for education of the public about the role of diagnostics in AMR, and for funding to support the implementation of diagnostics as well as their development.
The UK government is doing its bit by investing £50 million in a global AMR innovation fund, funding the development of diagnostics and exploring the use of rapid diagnostics to drive appropriate prescribing within the NHS, but it is going to take more than that.
In the case of the newer antibiotics, Franki Neal, director of marketing at Italian pharmaceutical company Menarini, suggests it could be up to the drug developers to fund the diagnostics:
“When a company develops a new anti-infective, hospitals and CCGs are likely to include diagnostic criteria. It will be in the company’s interest to develop and fund the diagnostic, getting point-of-care diagnosis into the healthcare chain. This is not the classic pharma sales model. It is closer to the biologics model, where companies pay for diagnosis and other services, and would need a dialogue between the Department of Health and big pharma,” he said.
“This will benefit GPs and patients, and is likely to gain a better price for the pharma companies. While some companies may see this as a restriction, we at Menarini see it as an opportunity.”
There is support for the use of diagnostics in the pharmaceutical industry, from both small and medium-sized entities (SMEs) and big pharma. At the smaller end, Summit Therapeutics is developing ridinilazole, a highly-selective antibiotic for Clostridium difficile infections. It is orally delivered and is not systemically absorbed. Because of its selectivity, a diagnostic is required. Summit’s chief operating officer, David Roblin, sees the way forward as using newer, targeted antibiotics first, along with diagnostics, and protecting the older, broader spectrum antibiotics for use where the selective antibiotics do not play a role.

Courtesy of David Roblin
David Roblin, Summit’s chief operating officer, sees the way forward as using newer, targeted antibiotics first, along with diagnostics, and protecting the older, broader spectrum antibiotics for use where the selective antibiotics do not play a role
“We use a 20-minute rapid enzyme-linked immunosorbent assay [ELISA], which detects the toxin in the stool, along with a clinical diagnosis. We use this rather than a DNA test because around 5% of the population have commensal C difficile in their guts, and the ELISA test just picks up the pathogenic form,” said Roblin. “While C difficile rarely shows resistance, agents used to treat the infection are also important against system infections, such as metronidazole and vancomycin. Using these too often can build up resistance as ‘collateral damage’. Using a narrow spectrum antibiotic also preserves the microbiome, which itself protects against infection.”
Swiss pharma giant, Roche, develops both pharmaceuticals and diagnostics, explained Pierre Hazlewood, director — Point of Care at Roche Diagnostics.
“Roche supports the recommendations from the Review on Antimicrobial Resistance that pharmaceuticals, diagnostics and the NHS should work together to improve access to diagnostics,” said Hazlewood.

Source: Roche
Pierre Hazlewood, director, Point of Care at Roche Diagnostics said that Roche supported the recommendations from the Review on Antimicrobial Resistance that pharmaceuticals, diagnostics and the NHS should work together to improve access to diagnostics
UK drug major GlaxoSmithKline (GSK) also sees the diagnostics route as an opportunity, and suggests a role for pharma in providing scientific advice and seed-funding for public-private partnerships and ‘prizes’ aimed at catalysing the development of fast, accurate and cost-effective point-of-care diagnostics. GSK is also working with companies, researchers, public health organisations and other stakeholders to develop diagnostics that ensure appropriate use of its antibiotics and antimicrobials. For example, GSK is partnering with a diagnostic company and other pharma companies to development a rapid diagnostic test that can target multi-drug resistant pathogens and support the appropriate use of antibiotics. There is a win-win for the company too.
“This engagement can help inform or complement our product development or post-marketing activity,” said a spokesperson from GSK.
The Longitude Prize, which opened for submissions in November 2014, was created to act as an incentive for diagnostics development to fight antimicrobial resistance. The £10 million prize fund will go to the first team that meets the criteria: to invent an affordable, accurate, fast and easy-to-use test for bacterial infections that will allow health professionals worldwide to administer the right antibiotics at the right time. As of August 2017, there are 239 entrants, including accuRx.
Where it comes to the generics, though, it will be a harder ‘sell’, both for the drug companies and for the health providers. Because of the low cost of generic antibiotics set against the potential costs of diagnostics, bringing in diagnostics is unlikely to be a cost-saving, or even a cost-neutral, process in the short- or medium-term. And that will be a big challenge for the cash-strapped NHS, and a harder job to persuade manufacturers.
“Pharmaceutical companies could set up contracts with the NHS, where they are contracted to supply a ‘basket’ of generics and higher-cost antibiotics, provided they pay for the point-of-care diagnostics,” said Neal.
Diagnostics in practice
There are a number of point-of-care approaches to testing for bacterial infections in use or in development. In 2016, Boots rolled out a ‘test and treat’ service for streptococcus A, aiming to cut inappropriate prescribing of antibiotics and reduce the number of consultations with a GP for sore throats. In a pilot study that began in 2014, 41% of patients presenting to the pharmacist with a sore throat were tested with an on-the-spot throat swab, 24% were positive for group A streptococci, and only 10% of the patients who initially consulted the pharmacist were given antibiotics[8]
,[9]
.
“Boots has trialled a strep throat diagnostic that individuals pay for in some London and Nottingham branches. I believe this should be encouraged to become bigger and by growing it the cost would probably come down,” said Lord O’Neill.
The effectiveness of this approach has, however, been questioned, with studies showing that the rapid antigen test used may not reduce antibiotic use any more than a clinical score would, and that any cost savings did not take into account the cost of service delivery[10]
,[11]
. While NHS England is backing the scheme, it has not as yet committed to a fully-funded national scheme[12]
.
Roche Diagnostics has begun to roll out a diagnostics device called cobas Liat, which uses molecular polymerase chain reaction (PCR) technology to test for viral or bacterial pathogens in a point-of-care setting rather than in a traditional molecular lab.
“The Liat device uses a PCR technique to make many copies of a specific DNA region, from a patient sample, in vitro (leading to the device’s name of Liat, or Lab in a tube). PCR can test for a specific bacterium or DNA virus: if a pathogen is present, it may be possible to amplify regions of its DNA from the patient sample. This enables healthcare professionals to make quick diagnoses (testing takes around 20 minutes) on illnesses such as flu, leading to better control of antibiotic use. Liat provides a clinical decision tool and helps justify the use of appropriate antibiotics for specific patients, and therefore can be personalised to the clinical need,” said Hazlewood.
According to economic models created by Aquarius Population Health, using point-of-care testing to identify drug resistance does increase treatment cost, but it optimises antibiotic choice, potentially reducing the longer-term impacts and costs of AMR[13]
. Aquarius, along with Atlas Genetics and the Applied Diagnostic Research and Evaluation Unit at St George’s University of London, is looking at mapping patient pathways and supporting the introduction of a diagnostic that can identify a variety of sexually transmitted infections in just 30 minutes rather than up to a week[14]
.
“This is a highly exciting and innovative approach to overcoming the substantial challenges to getting great technology adopted into the NHS by shedding light on potential routes through the complex landscape of factors and obstacles in our health systems,” said Tariq Sadiq, director of The Applied Diagnostic Research & Evaluation Unit at St George’s University of London.
Oxford Nanopore Technologies’ MinION is a portable real-time PCR-based DNA sequencer, including 10-minute sample preparation. While it is currently a research tool, the company plans to seek regulatory approval for a diagnostic version, which could be used to identify pathogens and look at resistance.
Diagnostics could make a difference
The general perspective is that adding in diagnostics to the antibiotics pathway is a positive and that the approach suggested by Davies could make a difference. Lord O’Neill is very much in favour of this type of approach, and said at the forum: “It is one of my favourite ideas. This is a relatively simple solution. We welcome it. It is not that much of a challenge. So many people in the health space think of everything in silos. Diagnostics is a massive part of the solution.”
RPS activity on antimicrobial stewardship
Antimicrobial stewardship has long been a policy and campaign focus of the Royal Pharmaceutical Society (RPS).
Responding to the UK Government’s Antimicrobial Resistance Strategy, published 13 September 2013, the RPS said that “Training of community pharmacists has the potential to reduce GP consultations by means of public education and symptomatic management of self-limiting infections”. In another response, to a 2014 NICE consultation on guidance for ‘Antimicrobial resistance: changing risk-related behaviours’ the Society said that the “use of minor ailment schemes whereby patients can receive symptomatic treatments for infections can decrease visits to a GP by 50% and reduce the number of prescribed antibiotics”.
In July 2014 the Society, together with the Royal College of General Practitioners (RCGP), the Royal College of Physicians (RCP), the Royal College of Nursing (RCN) and the UK Faculty of Public Health (FPH) published a Joint Statement on Antimicrobial Resistance. Among the recommendations of this statement was a call for antimicrobial prescribing data to be monitored, and for licensing requirements for new antimicrobials changed to include data on the minimum dosage required for clinical effectiveness.
In 2014, RPS Scotland collaborated with the Scottish Antimicrobial Prescribing Group (SAPG), Community Pharmacy Scotland and Pharmacy Voice to produce a European Antibiotic Awareness day resource pack for community pharmacists, which included a patient-directed self-care information leaflet for treating infectious ailments. The packs were distributed in November 2014.
Later that month, on European Antibiotic Awareness Day itself — 18 November 2014 — RPS Scotland held a parliamentary reception and debate on antimicrobial resistance, sponsored by Jim Eadie MSP. The event led to a Scottish Parliamentary debate on the subject, held on 5 February 2015. Also on European Antibiotic Awareness Day, RPS Wales and the Royal College of General Practitioners (RCGP) held a lunchtime discussion with Welsh Assembly Members (AMs) on the use of antibiotics in primary care. During the summit, the two professional bodies called for Wales to commit to a public education campaign on the subject, and greater antimicrobial stewardship.
At the 2017 annual conference, the RPS launched its new GB-wide campaign on antimicrobial stewardship. The campaign aims to show how pharmacists are contributing to a targeted 50% reduction in inappropriate prescribing of antibiotics by 2020. As part of this campaign, the AMS portal— a hub for health professionals co-produced by the RPS and University College London — will be updated and relaunched.
Throughout all antimicrobial campaign and policy activity, the Antimicrobial Expert Advisory Group — chaired by antimicrobial pharmacist Harpal Dhillon —acts to advise the Society and shape policy on the subject.
Your Society working for you.
Not a member? Become a member now
References
[1] O’Neill J. Tackling drug-resistant infections globally: Final report and recommendations — the Review on Antimicrobial Resistance. May 2016. Available at: https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf (accessed September 2017)
[2] Aminov RI. A brief history of the antibiotic era: lessons learned and challenges for the future. Front Microbiol 2010;1:134. doi: 10.3389/fmicb.2010.00134
[3] Fleming A. Penicillin — Nobel lecture. 11 December 1945. Available at: https://www.nobelprize.org/nobel_prizes/medicine/laureates/1945/fleming-lecture.pdf (accessed September 2017)
[4] Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T 2015;40(4):277–283
[5] AMR policy team. Government response to the Review on Antimicrobial Resistance. September 2016. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/553471/Gov_response_AMR_Review.pdf (accessed September 2017)
[6] Community Pharmacy Forward View. 2016. Available at: http://pharmacyvoice.com/wp-content/uploads/2016/08/Community-Pharmacy-Forward-View-FINAL.pdf (accessed September 2017)
[7] British In Vitro Diagnostic Association. Antimicrobial Resistance (AMR) Position Statement. January 2017. Available at: https://www.bivda.co.uk/Portals/0/Documents/Working%20parties/AMR%20Task%20Force/AMR%20Short%20Position%20Statement%20and%20Infographic%20%281%29.pdf (accessed September 2017)
[8] Oswald K. Pharmacy Strep A testing could reduce GP appointments for sore throats. July 2016. The Pharmaceutical Journal. Available at: http://www.pharmaceutical-journal.com/news-and-analysis/news/pharmacy-strep-a-testing-could-reduce-gp-appointments-for-sore-throats/20201494.article (accessed September 2017)
[9] Lewis G. NHS England to roll out Boots sore throat scheme. November 2016.Chem Drug. Available at: https://www.chemistanddruggist.co.uk/news/nhs-england-roll-out-boots%E2%80%99s-sore-throat-scheme (accessed September 2017)
[10] McCartney M. Testing sore throats at pharmacies won’t solve anything. 15 November 2016. The Guardian. Available at: https://www.theguardian.com/commentisfree/2016/nov/15/sore-throats-pharmacies-nhs (accessed September 2017)
[11] Little P, Hobbs FD, Moore Met al. Clinical score and rapid antigen detection test to guide antibiotic use for sore throats: randomised controlled trial of PRISM (primary care streptococcal management). BMJ 2013;347:f5806. doi: 10.1136/bmj.f5806
[12] Lewis G. NHS England clarifies position on Boots sore throat scheme. November 2016. Chem Drug. Available at: https://www.chemistanddruggist.co.uk/news/nhs-england-%E2%80%98support-scaling%E2%80%99-boots-sore-throat-scheme (accessed September 2017)
[13] Huntington S. Evaluating the use AMR POCT in treatment of gonorrhoea. July 2017. Aquarius Population Health. Available at: http://aquariusph.com/news/amr-poct-gonorrhoea-cost-effective-news/ (accessed September 2017)
[14] Aquarius Population Health. Aquarius Population Health wins a prestigious SBRI grant from Innovate UK. August 2017. Aquarius Population Health. Available at http://aquariusph.com/news/innovate-uk-grant-news/ (accessed September 2017)