Science Photo Library
An experimental group of drugs works wonders in a mouse-model of fragile X syndrome, the most common single-gene cause of autism. The drugs, which calm overactive metabotropic glutamate receptors (mGluRs) in the brain, restore social sniffing behaviour to normal levels, boost learning and memory, and reduce seizures related to the syndrome. Yet despite being the most promising new strategy for treating autism, these drugs are floundering once they reach human subjects.
The obscurity of the causes of autism means that doctors have little to offer the one in 100 people affected worldwide. Intensive behavioural therapies help some, but current medicines are limited to two drugs, risperidone and aripiprazole, used to treat aggression and irritability.
“There’s a place for those types of drugs, but they don’t really fix the main problems of autism at all,” says Kevin Sanders from Vanderbilt University, Nashville, Tennessee, a physician involved in multiple autism drug trials.
Finding drug targets based on the underlying pathophysiology of autism, rather than merely treating symptoms, is a possibility being raised by autism gene discovery, which has been invigorated in the past five years. Nearly a hundred genes have been implicated so far, and these conveniently coalesce around a few distinct biological pathways that could be worthy drug targets. Combining this genetic information with other biomarkers may also help unravel different subtypes of autism, which could be used to group patients in drug trials.
Translating research
Fragile X syndrome offers a cautionary tale about the difficulties of translating genetic insights into effective treatments. The mGluR drugs that worked so well in mice have repeatedly failed in clinical trials, most recently in one funded by Novartis and led by Elizabeth Berry-Kravis from Rush University in Chicago, Illinois[1]
. “Without having another model closer to human than mouse, there couldn’t be any more evidence that this would be a successful thing to do,” says Berry-Kravis.

Source: Elizabeth Berry-Kravis
Elizabeth Berry-Kravis, from Rush University in Chicago, is planning a new trial design for an mGluR blocker in fragile X syndrome
The disappointment follows two other failed trials: in 2014, Swiss pharmaceutical company Roche reported a lack of efficacy of its mGluR-inhibiting drug, RG7090, in fragile X syndrome. And in 2013, Seaside Therapeutics, based in Cambridge, Massachusetts, tested arbaclofen, which indirectly suppresses mGluR signalling, and it fell short in adults with autism — a result that interrupted a trial of the same drug in children and closed down the company.
Some issues lie in clinical trial design, for example, the mice studies measured learning while the human trials measured irritability, and the drugs remedied deficits in young and adult mice, but human trials focused mainly on adults. “We can’t decide the drug doesn’t work until we do a big paediatric trial,” says Berry-Kravis.
Finding treatments for autism is further complicated by the fact that researchers are still identifying the genes involved in autism, a condition stemming from many as yet nebulous causes. Modelling these genetic clues in mice or other species is crucial to understanding their function. But such findings must be interpreted carefully, since autism may affect brain regions specific to humans.
“Autism is in essence a uniquely human condition — much more developed in us than in mice,” explains Patrick Bolton, an autism specialist at King’s College London.
Ironing out the kinks in translating autism research is essential if the body of genetic work in humans is to be properly exploited.
It really has only been in the past three or four years that we’ve had a solid, highly reproducible set of autism genes with high effect size
Although the task list is long, each item is workable, says Matthew State, a psychiatrist and geneticist at the University of California, San Francisco. “It really has only been in the past three or four years that we’ve had a solid, highly reproducible set of autism genes with high effect size,” he says. “It takes a while to figure out how to leverage those basic biological insights to develop and bring to market novel treatments.”
Black box
For autism, heterogeneity is the rule. In the diagnostic manual used by US psychiatrists, more than 600 different combinations of symptoms can deliver an autism diagnosis. Defined by social and communication difficulties and repetitive behaviours that arise in childhood, autism is diagnosed in a range of people, from a person disabled by seizures and unable to speak, to someone who is highly intellectually capable and can live independently.
Symptoms are thought to reflect brain development derailed by genetic or environmental factors, or both. But what exactly has gone wrong in the brain remains unclear, making autism a kind of black box. What’s more, multiple pathophysiologies are suspected. Just as a fever may be caused by a bacterial or a viral infection, autism may be an outward sign of a problem in one of several different biological processes.
At least there is no shortage of treatment ideas, with more than 600 clinical trials registered worldwide. Some try to remedy biological effects of genetic mutations linked with autism, as in the mGluR trials, whereas others take a symptom-based approach. For example, Sanders is involved in a trial that seeks to boost sociability by inhibiting the actions of vasopressin, a peptide that counteracts the pro-social hormone oxytocin.
Genetic convergence
In 2012, three sequencing studies identified the first crop of autism genes, and hundreds more are expected[2],[3],[4]
. Although this progress is welcome, it initially led to concerns. “There was handwringing about if there are a thousand different autism genes, does there need to be a thousand different treatments?” says State, who has led some of the genetic studies. “But already we can see that the genes are self-organising into several different areas of biology.”
Autism genes converge on processes involved in wiring synapses together, or making DNA available for transcription, for example[5]
. This means that a particular biological pathway could be a drug target, rather than the individual gene products working in the same pathway. In this way, autism’s many different genes could reveal more clearly the core, malfunctioning biology.
“So I do think, in the long run, the heterogeneity is going to be a strength, and not as much of a curse,” says State.

Source: Matthew State
Matthew State, a psychiatrist and geneticist at the University of California, San Francisco, says that it has has only been in the past three or four years that we’ve had a solid, highly reproducible set of autism genes with high effect size
This idea has gained heft from a recent study showing that the Akt-mTORC1 pathway, a collection of molecules that work together to promote cell growth, is perturbed in Phelan-McDermid syndrome, an intellectual disability often accompanied by autism that is caused by mutations in the SHANK3 gene. Other single gene disorders associated with autism are also marked by disturbances in the Akt-mTORC1 pathway, namely Rett syndrome and Angelman syndrome.
A drug that restores the pathway was recently reported to normalise social behaviours in mice carrying SHANK3 mutations, as well as pathway abnormalities in induced pluripotent stem (iPS) cells grown from skin samples of Phelan-McDermid patients[6]
.
The addition of human cells to explore the effects of a mutation may add a safeguard against clinical trial failure, says study leader Ivan Galimberti from Novartis Institutes for BioMedical Research in Basel, Switzerland. Likewise, the new genetic information will lead to more precise animal models, including mice, zebra fish and most recently, monkeys[7]
. The monkeys did not fully reproduce behaviours seen in people with the same mutation, but they were less sociable and repetitively circled their cages. Although the monkey model received a muted reception, non-human primates are seen as essential animal models.
But no single animal or cell model will fully recapitulate autism. Instead, researchers say, each model should be seen as a tool with its own strengths and weaknesses.
“Autistic features in a mouse model, a zebra fish model, or even an iPS-derived neuron, may not tell you how sociability can be rescued in a person suffering from autism,” Galimberti says. “But these are the models we have and this is how we should try to move forward.”
Delineating people
While treatment targets may be identified by following these genetic trails, one target will probably not suit every person with autism. For example, a drug targeting glutamate neurons may not do much for people with autism that stems from another abnormality. Clinical trials may fail because true improvements in some patients are diluted by a lack of response in others, who have autism for a different reason.
We’ll see that some people are better, it’ll be easier to carry on a conversation with them, or they like hanging out with their family or friends in ways that they didn’t before, but it’ll end up being a failed trial
“We’ll see that some people are better, it’ll be easier to carry on a conversation with them, or they like hanging out with their family or friends in ways that they didn’t before,” Sanders says. “But it’ll end up being a failed trial.”
“Different people across the autistic spectrum may need different types of treatment because they have different causes and different neurobiology,” says Eva Loth from King’s College London. Loth is a science coordinator for EU-AIMS (European Autism Interventions – A Multicentre Study for Developing New Medications), a partnership between academia and pharmaceutical companies, including Roche and Eli Lilly, launched in 2012 to find treatment targets for autism and to identify autism subtypes.

Source: Eva Loth
Eva Loth, science coordinator for EU-AIMS (European Autism Interventions – A Multicentre Study for Developing New Medications), says that different people across the autistic spectrum may need different types of treatment because they have different causes and different neurobiology
EU-AIMS received US$34m — the largest grant in the world devoted to studying autism — from the Innovative Medicines Initiative, a public-private partnership between the European Union and the pharmaceutical industry association EFPIA. EU-AIMS comprises a collaboration of researchers in 37 European countries, which has allowed it to assemble the large group of people with autism necessary to detect subgroups with statistical certainty. The project is now characterising a variety of features in 800 people, more than half of whom have autism[8]
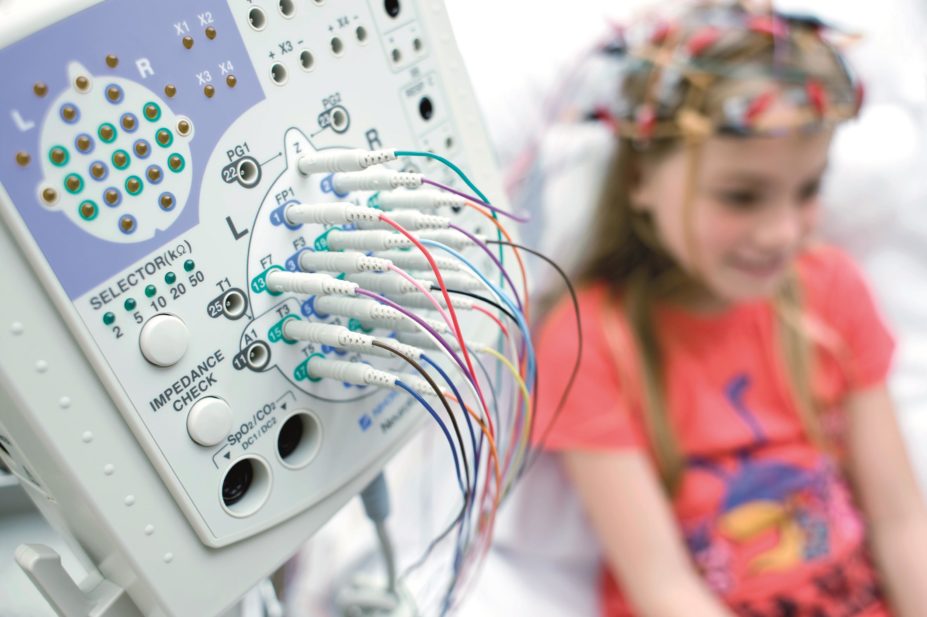
. These include: tests of eye movements, which can flag abnormalities in brain wiring; measures of brain structure and connectivity, as revealed by magnetic resonance imaging or scalp-based electroencephalogram; and blood tests that reveal metabolite signatures, or profiles of genetic variation, which may distinguish a person with autism.
These measures, or a combination of them, may eventually delineate autism into subgroups with their own distinct biology.
Other researchers and companies are seeking similar biomarkers. Not only will they help doctors match the appropriate treatment to their patients, but they may also eventually predict treatment response, or indicate whether a drug has reached an important brain circuit. This could help with dosing and give an understanding of how long a drug needs to be taken to have an effect.
Outstanding outcomes
While the genetic information filters in, objective ways to measure changes in autism’s diverse symptoms are needed, as well as ways to rework trial designs to make them more sensitive to the effects of drugs.
Drug trials may also miss meaningful changes if the measurement tools are too coarse. So far, clinical trials mainly rely on behavioural checklists, which give fuzzy snapshots of how well a person is doing. “A lot of families want a drug to work so badly because they’ve been waiting so long for our medical system to help them. So I feel like this maybe translates into families noticing changes in things they weren’t seeing before, even if they’re tiny,” says Sanders.
Several initiatives, including one led by pharmaceutical company Janssen, headquartered in Beerse, Belgium, are seeking more objective, standardised outcome measures.
One idea is to use wearable sensors to track a person’s activities throughout the day. For example, a 3D accelerometer worn by someone with autism can pick up their movements, and repetitive behaviours, such as rocking or flapping, can be extracted from these data with 90% accuracy[9]
. Audio or video data may eventually capture changes in social and communication abilities.
Some of these changes may be too subtle for parents to pick up on, but it doesn’t mean meaningful differences aren’t happening

Source: Empatica
A wearable sensor can track a person’s activities, for example, movements and repetitive behaviours, such as rocking or flapping, as well as detect sympathetic nervous system arousal
“Some of these changes may be too subtle for parents to pick up on, but it doesn’t mean meaningful differences aren’t happening,” says Matthew Goodwin from Northeastern University in Boston, Massachusetts. Goodwin developed a repetitive behaviour system, as well as one that detects sympathetic nervous system arousal, now sold by Empatica. Currently, he is working to use commercially-available equipment in the home of a person with autism, turning parents into citizen-scientists so that they can collect research-quality data.
Correctly interpreting such data remains a challenge, and it may be between five and ten years before these approaches find their way into the clinic, Goodwin says. “But I’m generally of the impression that more data are better,” he adds.
While outcome measures are under development, Berry-Kravis is planning a new trial design for a mGluR blocker in fragile X syndrome. It will have a learning-related outcome more aligned to mouse findings, one which drug companies had shied away from because it hasn’t been used before to gain regulatory approval.
“Some decisions for the previous trials were made simply on the basis of having a regulatory precedent, not because it was the most scientific thing to do,” says Berry-Kravis.
As planned, the trial will be conducted in children, with the drug given for a longer period than in previous trials, and objective measures of learning and cognition used. If the new trial design is successful, it could pave the way for similar trials in the future. Berry-Kravis says: “We might only have one shot at this, so we’re trying to fix all the problems in one study.”
References
[1] Berry-Kravis E, Des Portes V, Hagerman R et al. Mavoglurant in fragile X syndrome: results of two randomized, double-blind, placebo-controlled trials. Sci Transl Med 2016;8:321ra5. doi: 10.1126/scitranslmed.aab4109
[2] Sanders SJ, Murtha MT, Gupta AR et al. De novo mutations revealed by whole-exome sequencing are strongly associated with autism. Nature 2012;485:237-241. doi: 10.1038/nature10945
[3] O’Roak BJ, Vives L, Girirajan S et al. Sporadic autism exomes reveal a highly interconnected protein network of de novo mutations. Nature 2012;485:246-250. doi: 10.1038/nature10989
[4] Neale BM, Kou Y, Liu L et al. Patterns and rates of exonic de novo mutations in autism spectrum disorders. Nature 2012;485:242-245. doi: 10.1038/nature11011
[5] De Rubeis S, He X, Goldberg AP et al. Synaptic, transcriptional and chromatin genes disrupted in autism. Nature 2014;515:209-215. doi: 10.1038/nature13772
[6] Bidinosti M, Botta P, Krüttner S et al. CLK2 inhibition ameliorates autistic features associated with SHANK3 deficiency. Science 2016;351:1199-1203. doi: 10.1126/science.aad5487
[7] Liu Z, Li X, Zhang JT et al. Autism-like behaviours and germline transmission in transgenic monkeys overexpressing MeCP2. Nature 2016;530:98-102. doi: 10.1038/nature16533
[8] Loth E, Spooren W, Ham LM et al. Identification and validation of biomarkers for autism spectrum disorders. Nat Rev Drug Discov 2015;15:70-73. doi: 10.1038/nrd.2015.7
[9] Goodwin MS, Intille SS, Albinali F et al. Automated detection of stereotypical motor movements. J Autism Dev Disord 2011;41:770-782. doi: 10.1007/s10803-010-1102-z


