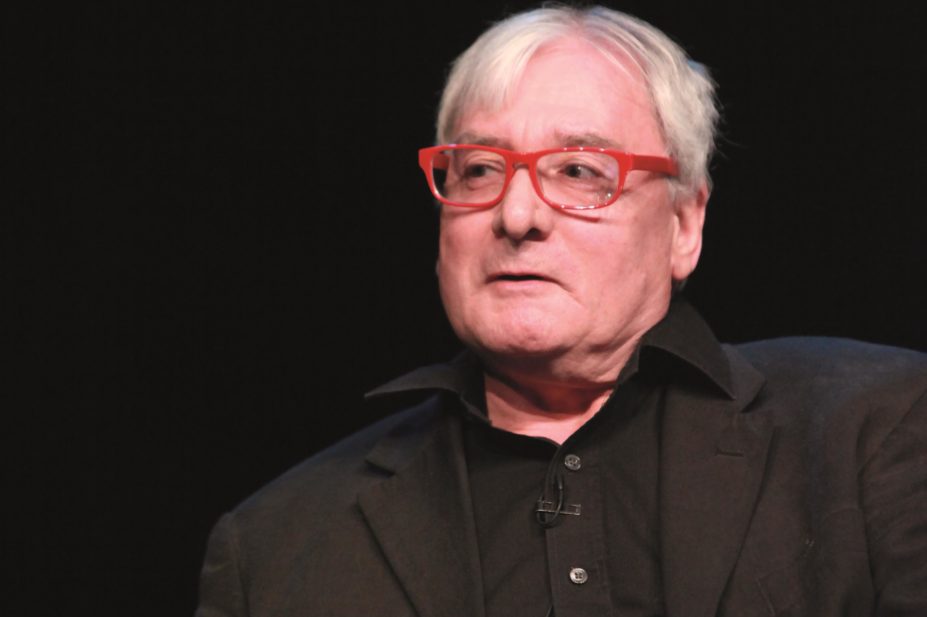
Nadia Attura
Following his recent retirement as chief pharmaceutical officer in the Scottish Government, Bill Scott discusses initiatives to promote greater integration of pharmacists into general practice and how pharmacy training should accommodate the growing emphasis on pharmaceutical care.
‘Prescription for excellence’, a vision and action plan for the future of NHS Pharmaceutical Care in Scotland (launched in 2013), is seen as a huge vote of confidence for the profession. What were the challenges in pushing this through government?
‘Prescription for excellence’ is part of a long-term strategy for pharmacists to work in collaborative partnerships with medical practitioners, and we worked with ministers, civil servants and others for some time to promote the pharmacist as a clinician. We had a sound base for the programme, thanks to the ‘Review of NHS pharmaceutical care in the community in Scotland’ by Nick Barber and Hamish Wilson. As part of the review, they held numerous meetings with the profession, contractor groups and the public to discuss how pharmacists can be involved in improving pharmaceutical care.
There is now a team working across the Scottish Government pharmaceutical division and the health boards that is working towards delivering the plans outlined in ‘Prescription for excellence’. They are dealing with pharmacists and GPs who are showing support and enthusiasm but this is a ten-year programme and it will take time for it to be implemented. At an individual level, there will be a natural progression for GPs and pharmacists to work together more closely.
Other parts of the UK are looking at this and are engaged in producing strategies. At the end of the day, the difference will be in the time taken to achieve these things rather than whether or not they are achieved.
How do you envisage the pharmacy degree changing in the next five to ten years?
The drivers will be the ways in which the health service, social care and patients regard pharmaceutical care. The skills that pharmacists will need will depend on how pharmaceutical care is integrated into the healthcare system, but pharmacy training will need to be more clinically oriented and there will be a need for greater patient contact at an earlier stage of the undergraduate syllabus. I would be supportive of greater integration of medical and pharmacy students during their training.
Pharmacy training will need to be more clinically oriented and there will need to be greater patient contact at an earlier stage of the undergraduate syllabus
I can only speak for Scotland, but I know that the schools of pharmacy in Scotland are starting to engage with this. Like any business, the universities will have to pay attention to what their customers require.
Your comments at the Royal Pharmaceutical Society Annual Conference 2014 regarding taking science out of the pharmacy degree drew much criticism. Do you stand by this view?
I was responding to questions and we didn’t have enough time to have the discussion that was required because of the nature of the event. It stimulated interest and opinion and it’s now for others to move the discussion forward.
The reason for doing it was to get people to think about the future. The pharmacy degree currently requires chemistry at A level (or higher level in Scotland), but we need graduates with the ability to solve problems and to think laterally and in a broader way. This does not depend on any particular aspect of science, so I don’t think we should limit people getting on the pharmacy course based on chemistry.
I don’t think we should limit people getting on the pharmacy course based on chemistry
Historically, pharmacy was wedded to chemistry and, if you look at practitioners now, there are still some who will work in the pharmaceutical industry synthesising new drugs. But the bulk of our graduates will work in the NHS, directly or indirectly, and the priority is on the appreciation of clinical care and social care.
What was your proudest achievement during your term as chief pharmaceutical officer of Scotland?
We all stand on the shoulders of the giants who’ve gone before and that’s what allows us to make progress. But the thing I feel good about is that civil servants, the public and other professions now think of pharmacists as part of the clinical team of clinicians and not as shopkeepers or chemists. I’m also pleased to have been in post through two major strategies for my profession – ‘Prescription for excellence’, of course, and ‘The right medicine’, on which ‘Prescription for excellence’ was built.
What is Scotland doing better in terms of the chronic medication service and minor ailments?
The terminology probably isn’t right because the public don’t see “chronic” as a good thing. But the concept of looking at the patient from beginning to end, and not just their prescriptions, is important. The chronic medication service allows patients with long-term conditions to register with a community pharmacy of their choice for the provision of pharmaceutical care, as part of a shared agreement between the patient, community pharmacist and GP. ‘Prescription for excellence’ builds on that.
We brought the minor ailments service in under a programme of social justice when we had prescription charges in Scotland, and it was primarily for patients who could not afford to purchase medicines themselves. We wanted to encourage them to visit their pharmacist, so it was a way of giving them access to medicines without having to go through the GP. That system could evolve into more of a common ailments service with the pharmacist working closely with other healthcare professionals in the GP practice. For this, pharmacists need a wider skill set so there is a trust and understanding between all the healthcare professionals about their strengths and how they can best be used together.
We have too many pharmacists and not enough GPs. What is your solution?
With the current excess of pharmacists and shortage of GPs, we must encourage closer working so that pharmacists can use their skills when working with GPs in their practice. That doesn’t mean pharmacists walking in and taking over – there is enough work for all of us. It’s all about how we work and train together and have a joint vision of patient care. We’re not looking to produce barefoot doctors but we must look at how both professions can work together for the benefit of patients.
What is the one public health issue the new UK government should tackle?
The government needs to encourage healthcare professionals to work with education services and engage with the public from an early age so they have a better appreciation of how their body works and how to stay well.
People need to be encouraged to look after their body as they would a new car
If you ask a child — or an adult — where their heart or their spleen is, it’s not something they can often answer. People need to be encouraged to look after their body as they would a new car — to read the “owner’s manual” — and to understand what is good and bad for it. If a society has a good understanding of health, it makes it easier to approach preventive medicine and this would pay dividends in the future.
What are your future plans?
I’m going to chill out and relax. I’m still getting used to the idea of staying in bed after the alarm, but I also want to keep my brain active. So I will be looking for new challenges, I just don’t know what they are yet.


