
Mark Thomas / Science Photo Library
1. Engage clinicians early and at all stages of the project
Make sure staff members are on board from the beginning — resistance from those who are going to be using the systems daily will inevitably get in the way of a smooth transition.
Kavi Gohil, senior pharmacist and electronic prescribing and medicines administration (EPMA) lead at St Andrew’s Healthcare — a large mental health charity treating NHS patients across England — has overseen the implementation of an EPMA system in more than 70 hospital wards. He created a one-page briefing document on forthcoming changes for each specialty and gave each team at least six weeks’ notice before the new system was put in place.
Displaying the benefits of the changes and appeasing concerns is critical to ensure that early adoption of the system is successful
“Displaying the benefits of the changes and appeasing concerns is critical to ensure that early adoption of the system is successful,” he says.
Arti Punn, lead community healthcare pharmacist at Birmingham Community Healthcare NHS Foundation Trust, agrees, adding that getting support from doctors, nurses and pharmacists will help individualise the system.
“It makes a big difference to how you want the system to work and understanding the output of a system — why some things would work efficiently and perhaps where they might not.”
2. Learn from those who have already done it
Efforts are already being made by NHS trusts to share information and best practice on the use of EPMA systems. There is a lot of experience out there — the first of these systems went live in the early 1990s. In 2016, a programme to create global digital exemplars— NHS trusts deemed to be “delivering improvements in the quality of care through the world-class use of digital technologies and information” — was launched by NHS England. Now totalling 17 acute trusts, 3 ambulance trusts and 7 mental health trusts, these exemplars have been sharing their experiences by creating blueprints to enable other, less advanced trusts to follow in their footsteps as quickly and effectively as possible.
Visit other sites that have already implemented the software and ask for their lessons learned and benefits realised
Similarly, the ePrescribing Research Programme, funded by the National Institute for Health Research, has developed the ‘ePrescribing toolkit’ for NHS hospitals, which contains case studies, a series of ‘How to’ guides and several tools to support EPMA implementation.
However, Gohil says getting out of the office is just as important. “Visit other sites that have already implemented the software and ask for their lessons learned and benefits realisation piece of work,” he advises. “This will help you to avoid similar mistakes and save you time and resources.”
3. Ensure the right team is in place
Getting an EPMA system in place is a huge undertaking that will likely take years between procurement planning and full rollout. During that period, putting together the right project team and having good leadership in place is vital to the implementation running as smoothly as possible.
The project team should involve people with different knowledge and skills on both the technical and clinical sides. Ideally, it should have representation at executive or senior clinical leadership level to give the project visibility and ensure motivation to see it through.
Aziz Sheikh, chair of Primary Care Research and Development at the University of Edinburgh, says implementing EPMA is a “challenging” area to get right and leadership has an important role to play in seeing such a project through those tricky times.
“Providers need to commit for the long haul in order to maximise realisation of benefit,” he adds.
4. Push for high investment
EPMA systems come in a variety of shapes and sizes, encompassing everything from basic electronic versions of a drug chart in standalone systems to fully integrated versions that incorporate patient records, laboratory results and other relevant information. Some can even work as closed-loop systems, using barcodes to track medicines from prescription to administration.
If you make the right investment it will be so worth it in the long run
While Punn says she understands NHS trusts have other financial pressures, she would always advocate for the maximum possible investment in EPMA systems. A quick fix now might not be the best option in the long term.
“If you make the right investment it will be so worth it in the long run,” she says.
Matt Elliott, a pharmacist with responsibility for EPMA at University Hospitals of Derby and Burton NHS Foundation Trust, says that investment is about more than the purchase price of the system.
“Clinical staff, for example, are busy and will need protected time if the project is to be a success. It will always cost more than you imagine,” he says.
Putting together a comprehensive business case is vital to securing the required investment. This should set out how the EPMA system fits with the overall organisational information strategy, as well as the organisational and individual benefits that can be expected as a result of its implementation.
Several examples of NHS hospitals’ business cases are available to view in the ePrescribing toolkit.
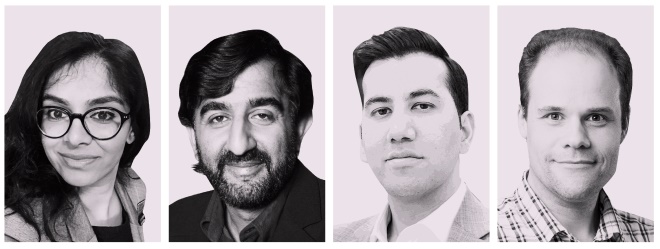
Source: Courtesy of Arti Punn; Aziz Sheikh; Kavi Gohil and Matt Elliott
From left: Arti Punn, lead community healthcare pharmacist at Birmingham Community Healthcare NHS Foundation Trust; Aziz Sheikh, chair of Primary Care Research and Development at the University of Edinburgh; Kavi Gohil, senior pharmacist and electronic prescribing and medicines administration (EPMA) lead at St Andrew’s Healthcare; and Matt Elliott, a pharmacist with responsibility for EPMA at University Hospitals of Derby and Burton NHS Foundation Trust
5. Future-proof the infrastructure
It is important to consider the purpose of the EPMA system and ensure that it is not only appropriate for current or short-term needs. A standalone system may work as a quick fix for moving a hospital from paper to electronic prescribing but it may be of no use in the future if systems are required to work together.
It could be the best EPMA out there, but if the hardware to access it has flaws then acceptance may be hindered
Punn points out that an inability for systems to integrate may leave trusts sharing information in risky ways or ultimately spending more money on other systems to bridge the gap. “This could all be avoided through making the right choices and investments [at the outset], with government backing for integration in technological systems,” she adds.
Elliott has found that the user interface for both hardware and software is just as important as system functionality. “It could be the best EPMA out there, but if the hardware to access it has flaws then acceptance may be hindered.”
6. Gradually move up to using complex features
Do not run before you can walk — getting the basics right is important. Brian Power, lead informatics pharmacist at Wirral University Teaching Hospitals NHS Foundation Trust, says his trust has done a lot of work analysing simple things, such as how people search for medicines on an electronic list to help prescribers pick the right item.
“Go back and start at the basics, and consider how your prescribing will integrate with the system,” says Power.
“We need to be looking at system design and usability. For example, we tried to constrain having multiple records open at once. We need to go right back to looking at the best way to present drugs and decision support,” he adds.
7. Ensure devices are fit for purpose
Poor Wi-Fi connectivity is one of the most common reasons for failure in implementing an EPMA system, says Ann Slee, associate chief clinical information officer for medicines at NHSX, a unit launched in early 2019 overseeing digital transformation in the NHS.
“Having good Wi-Fi connectivity across an organisation is critical,” she adds. After all, what is the point of having an electronic system if staff cannot properly access it during the course of their work?
“Get a wide range of devices for clinical staff to test, in the environment that they will be using them. Let them feedback what works for them in their context,” advises Elliott.
“This may mean you need a range of devices across locations to fit with different workflows. The same goes for connectivity; map and re-map wireless coverage to ensure there are no dead spots,” he adds.
8. Adapt the system for different departments
Many of those who have gone through the process of EPMA implementation have found that wards and departments within the same hospital trust have unique ways of doing things or requirements that others would not need. For example, an emergency department may do things differently to others because of the high level of patient turnover, and need to give verbal orders or retrospective prescribing.
Equally, some trusts with more than one site have found that hospitals within the same organisation do things differently, in which case there needs to be a certain amount of flexibility.
“Ensure configuration of the system is completed to meet the requirements of your local trust’s needs,” says Gohil, who found differences in the way departments needed to obtain consent for treatment from patients.
“One size may not fit all,” he warns.
9. Mandate the system’s use
Implementing an electronic prescribing system is not something that can be done in a half-hearted way. Staff will have to be on board with using it if it is to have any degree of success. But this also means that the planning process before going live is essential — if a system is going to be mandatory, it needs to meet the requirements of those using it.
There must only be one prescribing system in place for any patient at one time
“There must only be one prescribing system in place for any patient at one time,” says Elliott.
“Any more than this is a risk to patient safety because staff administering the medicines could become confused.”
He adds that options for reversion should be limited and controlled, and co-ordinated by the organisation.
“This should ensure a co-ordinated response and assure patient safety.”
10. Make it easy for staff to report problems
There will always be problems with new systems because they bring change to old ways of working. This means you will need to have a strong team in place to support the post-deployment phase, says Punn. “Where problems are not reported because the reporting process is slow, or feedback is slow, it creates a negative attitude towards working or carrying out tasks.”
Gohil agrees that following up with staff after implementation is important “to resolve any niggles and issues they may have”, as this may deter them from using the system or even lead to them reverting back to paper prescriptions.
The ‘how’ is also vital in this case, says Elliott. “Dedicated areas on intranet sites, generic email addresses for comments, criticism and feedback all help. Consider the use of blogs, vlogs and multimedia to engage and inform users.”
You may also be interested in

Reviewing prescribing practice in an adult critical care unit with a newly implemented electronic prescribing system
