JL / Shutterstock.com
The much-anticipated new community pharmacy contract was unveiled in July 2019. The five-year contract — due to start operation on October 2019 — marks a big change for community pharmacy in England, with income from dispensing being gradually reduced and the proportion of funding for clinical services being increased.
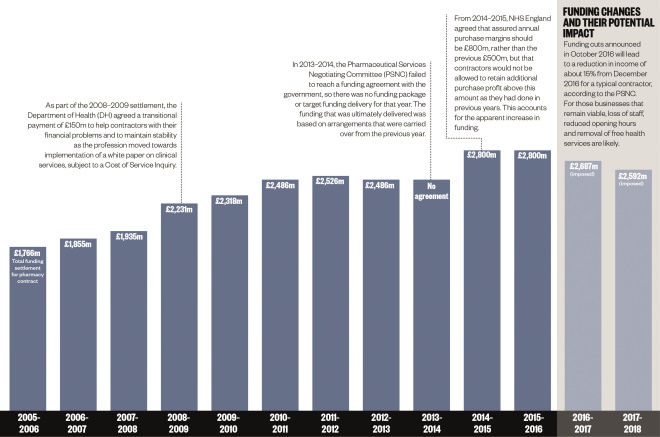
Although generally welcomed by pharmacy bodies (see ‘First impressions’), the resulting document was light on both detail and extra funding for the sector, with the Department of Health and Social Care (DHSC) setting out how it plans to spend funds, which have been frozen at £2.59bn per year for the next five years, in just 26 pages.
But despite its brevity, the contract does offer the sector a new, more clinically-focused, direction, which pharmacy bodies, including the Royal Pharmaceutical Society and The Company Chemists’ Association, have been calling for for years.
Some of the finer details behind the new services that community pharmacists will be expected to provide have yet to be worked out between the DHSC and the Pharmaceutical Services Negotiating Committee (PSNC); however, there are already five major things that community pharmacists need to understand before the contract begins.
1. Community pharmacies will gradually be paid less for dispensing medicines
The sector is expected to receive a total of £13bn over the five years between 2019/2020 and 2023/2024 at a flat rate of £2.6bn each year. This investment is not expected to change to reflect the inflation rate, which currently sits at around 2%.
But pharmacy negotiators regard this as a victory; the PSNC said in a webinar on 25 July 2019, which explained changes to the contract to pharmacists, that its negotiators were “very close” to walking out of the contract talks as a result of the government’s initial funding proposals.
Although the amount of funding is staying largely the same, how it is being delivered to pharmacies is changing but the details on this are vague.
The contract states that the government “expects that the level of funding for dispensing will reduce, by an amount to be agreed, over the course of the settlement as new technology and transformation is enabled”. This prospect is likely to alarm many contractors, even though the document says this funding released will be recycled to fund further service provision by community pharmacies.
To achieve this, the government has said it will move forward with “automation and developments in information technology and skill mix”, including hub-and-spoke dispensing and allowing pharmacy technicians to take on dispensing roles to free up pharmacist time. However, the details of these longer-term ambitions have yet to be discussed fully or agreed with the PSNC.
More broadly, the government believes the agreed level of funding is “still supporting more pharmacies in some places than may be necessary”, suggesting ministers would not be overly disappointed if this deal precipitated an increase in pharmacy closures.
2. Medicines use reviews will be completely phased out
Funding for medicines use reviews (MURs) in community pharmacy will gradually decline until it is phased out completely in 2020/2021.
According to the contract, structured medication reviews carried out by pharmacists working in primary care networks “are more clinically effective for patients than the current” MURs offered in pharmacies. As a result, community pharmacists will each only be able to provide up to 250 MURs during 2019/2020 and 100 MURs in 2020/2021. After that, MURs will cease to exist as a service.
But community pharmacists will still have a role in medicines optimisation and safety. Pharmacists will instead participate in a medicines reconciliation service “to ensure that changes in medicines made in secondary care are implemented” after the patient is discharged. The government has also committed to expanding the new medicines service “to include further indications and conditions”.
However, further details on how and when these services will be rolled out have yet to be announced.
Much of the funding from MURs will be redirected to an “unallocated” pot of funding “for future clinical services” and “transition payments”, which amounts to £1.02bn over the five-year contract.
First impressions
“This deal provides the accessible and convenient healthcare that the public really wants, while offering a more fulfilling clinical career to pharmacists and pharmacy technicians as a valued part of the NHS team” — Keith Ridge, chief pharmaceutical officer for England
“Referring patients with minor illnesses [to community pharmacy] who would have otherwise required an appointment with their GP to community pharmacists will be game-changing for our primary care systems” — Claire Anderson, chair of the Royal Pharmaceutical Society English Pharmacy Board
“While we recognise that a further five years of flat funding will present significant challenges to what is already a financially strained sector, we are encouraged by the direction of travel set out by the agreement” — Malcolm Harrison, chief executive of the Company Chemists’ Association
“Pharmacists are integral to community health and I want to move towards the French model, where they offer a wider range of services and play a stronger role in the community” — Matt Hancock, health and social care secretary
3. Pharmacists will take on a bigger role in urgent care
One of the biggest changes will be the national roll-out of the ‘community pharmacist consultation service’ (CPCS).
The CPCS will roll out nationally from 29 October 2019 and will replace both the NHS urgent medicines supply advanced service and the digital minor illness referral service.
As part of the CPCS, pharmacists will be paid £14 per consultation to field referrals from an increasing number of providers, including NHS 111, GPs, urgent care centres and eventually A&Es.
Pharmacies will be able to receive alerts of incoming referrals to the service through the “CPCS IT system”, which will be provided by NHS England for the first 18 months of the service. But from April 2021, pharmacies will have to source their own IT system if they want to continue offering the service.
Pharmacies offering the NHS CPCS by 1 December 2019 will be given £900 to help with set-up costs. However, those signing up after this, but before 15 January 2020, will only receive £600 (see ‘Key dates’).
Overall funding for the CPCS will increase from £4m in 2019/2020 to £19m in 2023/2024.
A further £10m has been set aside to reimburse pharmacists for dispensing according to a serious shortage protocol at the cost of £5.35 per item.
4. Pharmacists will provide an increasing number of clinical services
The contract does not specify how many or which services will be included by the end of the contract, but several services are set to be tested in community pharmacy by 2024. These include:
- Introducing a hepatitis C testing service in pharmacies for any patients using needle and syringe programmes;
- Piloting a case-finding scheme for undiagnosed cardiovascular disease;
- Piloting a stop-smoking referral scheme from secondary care;
- Piloting point-of-care testing in community pharmacies to support efforts to tackle antimicrobial resistance.
The schemes are expected to start in 2019/2020 and finish in 2020/2021, after which they would become nationally commissioned services if they had “demonstrated value for money”.
In his introduction to the contract document, Matt Hancock, the health and social care secretary, says he expects the five-year contract to allow community pharmacies to become “further integrated within local primary care networks”. But day-to-day, community pharmacists will likely see their jobs shifting away from dispensing towards more clinical, patient-facing care over the next five years.
5. Pharmacy incentives will change
A revamped quality payments scheme — now called the pharmacy quality scheme (PQS) — will include 26 incentivised targets worth a total of £75m. Some of the previous incentive measures, including accessing the summary care record, will become essential terms of service for community pharmacy contractors from April 2020.
One of the new incentives include requiring community pharmacies to reduce their sales of sugary drinks to no more than 10% of all beverages sold by volume.
The government has also committed to improving reimbursement arrangements to ensure a fairer distribution of the £800m annual medicines margin, with proposals suggesting that community pharmacists recoup less money on Category M generics for which a branded version exists and more money from all other Category M drugs.
A consultation on the changes was published shortly after the contract announcement and will close on 17 September 2019.
Key dates
1 October 2019: New contractual arrangements come into force.
1 December 2019: Pharmacies that sign up to the new ‘community pharmacist consultation service’ (CPCS) by this date will receive £900 to help cover set-up costs.
15 January 2020: Pharmacies that sign up to the new CPCS by this date will receive £600 to help cover set-up costs.
31 March 2020: All pharmacies will be expected to have cut the total volume of sugary drinks sold to 10% or less of all beverages.
By end of 2019/2020 financial year:
- Pilot of the CPCS with referrals from NHS 111 online begins;
- Pilot of case-finding for undiagnosed cardiovascular disease begins;
- Pilot of stop-smoking referrals from secondary care begins;
- Pilots for point-of-care testing in community pharmacy begin.
April 2020:
- National rollout of CPCS referrals from GP practices to community pharmacies;
- All community pharmacies expected to become ‘level 1 healthy living pharmacies’;
- All pharmacies must be able to access summary care record and process electronic prescriptions.
By end of 2020/2021 financial year:
- Introduce a medicines reconciliation service as part of a ‘transfer of care around medicine’ service;
- Government to review payment model of CPCS and medicine use reviews to be fully phased out.
By end of 2021/2022 financial year:
- Pilot of the CPCS with referrals from urgent treatment centres begins;
- Undiagnosed cardiovascular disease case-finding service commissioned nationally if it “demonstrated value for money”;
- Stop-smoking referrals from secondary care service commissioned nationally if it “demonstrated value for money”;
- Discuss and agree any expansion of the new medicine service to other therapeutic areas.


