
Courtesy of Angela Alexander / University of Reading
Mark Tomlin, an experienced prescriber and consultant pharmacist in critical care at University Hospital Southampton NHS Trust, spends much of his time managing and correcting errors made by medical prescribers.
“Medics come out of medical school with very little formal [prescribing] training and tend to learn ‘on the job’,” he says, describing this approach as ‘learning from Nelly’. “If Nelly taught it badly, errors are perpetuated,” he says.
Tomlin, who teaches junior doctors at the hospital, believes that part of the problem is that not all prescribers use the prescribing competency framework, first published in 2012 by the National Prescribing Centre through the National Institute for Health and Clinical Excellence (now called the National Institute for Health and Care Excellence [NICE]).
The framework sought to provide a unified set of competencies for all prescribers and outlined what good prescribing looks like, such as applying evidence-based practice and considering all treatment options. It was designed for use as a training resource and thereafter for reflection on practice and continuing professional development (CPD). The single framework replaced all profession-specific frameworks that had been published previously for each of the non-medical prescribing professions.
The unified approach recognised that a common set of competencies underpins all prescribing, regardless of professional background, and allowed prescribers to see clearly the activities or outcomes that they should be able to demonstrate.
The NICE framework was due to be updated in 2014 but as the scope of NICE’s work expanded, the framework was neglected. The task of revising it was taken over by the Royal Pharmaceutical Society (RPS) in October 2015. Nine months later, in July 2016, the RPS published ‘Competency framework for all prescribers’ (see ‘Figure 1: The framework’)[1]
.
Talking to those involved in developing the framework and clinicians who use it in their daily practice gives an insight into why the framework is needed and how it can be used to make prescribing safer.
A competency framework for all prescribers
The process of updating the framework (see ‘Box 1: How the framework was updated’) led the RPS to work with a range of experts from across disciplines and sectors: the 23-person steering committee had input from pharmacy, physiotherapy, radiography, nursing, dentistry and medicine. It was supported by a project board and validation group, along with an external referencing group, bringing the number of professionals involved in the framework’s development to 120, plus 3 lay persons.
The aim was to make the framework a more comprehensive and rationalised document, one that is relevant to all prescribers, explains Angela Alexander, professor of pharmacy education at the University of Reading, who was a member of the steering committee.
Three areas where it changed the most were in the framework structure, making it more logical and removing duplication; streamlining the guidance on professionalism; and giving more focus to stopping medicines, known as deprescribing.
Catherine Duggan, director of the RPS’s professional development and support programme, sees the new framework as an evolution in guidance, rather than a change, reflecting the shifting nature of prescribing and emergence of new non-medical prescribers.

Source: Simon Wright Photography / The Pharmaceutical Journal
Catherine Duggan, director of the RPS’s professional development and support programme, says the new framework reflects the shifting nature of prescribing and emergence of new non-medical prescribers
Nurses were the first non-medics to be granted independent prescriber status in 2006, with pharmacists and optometrists following in 2006 and 2008, respectively. Physiotherapists, chiropodists and podiatrists could become independent prescribers from 2014. And therapeutic radiographers joined the ranks of non-medical independent prescribers in 2016.
Prescribing has also become more complex. Polypharmacy is common in older people, who often have comorbidities, and in people with long-term conditions, which is why these cases are prioritised for medication reviews and medicines optimisation.
Alexander, who runs the joint pharmacist and nurse prescribing course at University of Reading, says good prescribing should support patient care and encourage adherence, while taking into account clinical response, tolerability, lifestyle and some negotiation. “It’s about giving [patients] options and involving them in the choice of medicine,” she adds.
Alexander gives the example of managing hypertension — starting with an angiotensin-converting enzyme (ACE) inhibitor, such as ramipril, but switching to losartan if ramipril is not tolerated; if the patient’s blood pressure is still uncontrolled then amlodipine can be added, although alternatives should be tried if there is ankle swelling. Other complex areas include anticoagulation (using warfarin or new oral anticoagulants and vitamin K) and prescribing adjunct treatments to counter the side effects of chemotherapy (e.g. anti-emetics and skin preparations).
Rachel Hall, a clinical pharmacist and partner at the Old School Surgery GP practice in Bristol, has been an independent prescriber since 2007. She describes good prescribing practice as spending sufficient time with the patient (typically 20 minutes), talking to them about side effects, interactions and contraindications, and monitoring relevant data. It is also important to consider which dosage schedule would suit the patient’s lifestyle and preferences, and to identify the particular needs of certain compromised patients (e.g. those with renal impairment). “Deprescribing is just as important, especially in palliative care,” she adds.

Courtesy of Rachel Hall
Rachel Hall, a clinical pharmacist and partner at the Old School Surgery GP practice in Bristol, says an important aspect of effective prescribing is to meet as a team of multidisciplinary clinicians and discuss decisions
Regular medication reviews enable clinicians to check that the medication prescribed is appropriate for the patient’s needs, is effective for the patient and is a cost effective choice.
Prescribing within a multidisciplinary team
Another important aspect of effective prescribing is to meet as a team of multidisciplinary clinicians and discuss decisions around prescribing, says Hall. This models the approach taken in secondary care and promotes mutual understanding across specialities, drawing on different skills so that care becomes more centred on the patient. “If a GP practice does not have a pharmacist on site then that GP should have a relationship with the local pharmacist that would allow these discussions,” she says. “GPs should not be prescribing in isolation because these decisions are very complex.”
Hall works with 14 GPs, four nurse practitioner prescribers and an additional pharmacist who runs an attached pharmacy. If the framework is used by all the prescribers in the team to optimise prescribing practice, it can help build relationships and allow shared decision making, she says. “You never have to make a clinical decision on your own,” says Hall.
Aligned with multidisciplinary care is the drive by NHS England to boost the number of pharmacists working in GP practices[2]
, which will lead to higher numbers of pharmacists becoming prescribers.
Helen Williams, a prescriber and consultant pharmacist for cardiovascular disease at Southwark clinical commissioning group (CCG), says that greater numbers of prescribing pharmacists should bring a different perspective to prescribing because they will have a dual role of reviewing GP prescribing and ensuring the whole practice is safe.

Courtesy of Helen Williams
Helen Williams, a prescriber and consultant pharmacist for cardiovascular disease at Southwark clinical commissioning group (CCG), wants the framework to be built into revalidation processes for both GPs and pharmacists
However, there is an added challenge for pharmacists working in multidisciplinary teams within GP practices: they do not have the backing of a pharmacy department, which a hospital prescriber would have. “Having a formal framework will help that, particularly if they are challenging established ways of working,” she says.
The framework also provides a clinical governance structure for these pharmacists, allowing them to measure competency during training and as part of CPD. “As individuals we have to take responsibility and having evidence of competence is quite powerful, especially if pharmacy is being scrutinised,” Williams explains.
Good prescribing should take a patient-centred approach, and this is reflected in the updated competency framework. Hall says there is an appetite for including patients in decision making and since pharmacists tend to have more consultation time than GPs, they can add value in this respect.
Interaction with peers was noted as a “powerful tool” used by pharmacist prescribers to keep their knowledge and skills up to date in a report produced by British pharmacy regulator the General Pharmaceutical Council (GPhC) in May 2016[2]
. The GPhC’s ‘Prescribers survey report’ also highlighted the importance of support and mentoring during and after qualification in facilitating more non-medics to become prescribers.
Using the framework to make prescribing safer
How the framework is used will determine its success in improving prescribing. Some people who already use it see the uptake of the framework by all prescribers, in particular medics, as critical to its success.
Williams wants the framework to be built into revalidation processes for both GPs and pharmacists. She explains that review of prescribing practice is currently ad hoc, whereas the framework would give it a formal structure.
Alexander suggests that the framework can be used as a “gap analysis for future CPD”. However, she agrees that using the framework as part of revalidation will be a more robust way of identifying that a healthcare professional is still a safe and effective prescriber and is taking active steps to improve their prescribing practice.
Richard Harris, professional development pharmacist at independent pharmacy chain Weldricks, also sees the framework as a tool that should be used as part of CPD. However, he acknowledges that pharmacists are continually reflecting on their prescribing practice as counter prescribers. “What prescribing means to a lot of people is supplying prescription only medicines (POMs),” he says. “But let’s not underestimate what pharmacists are doing already with counter prescribing, as they’re applying the same principles.”

Courtesy of Richard Harris
Richard Harris, professional development pharmacist at independent pharmacy chain Weldricks, sees the framework as a tool that should be used as part of prescribers’ continuing professional development
Although pharmacists and other non-medical prescribers are already using the framework as part of their postgraduate prescribing training, getting the framework used by medical schools is the biggest challenge, says Tomlin, another member of the framework steering committee.
“There is a political sensitivity that doctors have always prescribed [with the implication that things are OK as they are],” he says. This framework will help shape the training they receive after their degree, he adds. “It’s for all people who write prescriptions.”
Many prescribers do not know that the framework exists, adds Tomlin. He suggests awareness should be raised post-qualification through induction programmes and product training.
Harris echoes Tomlin’s view that the framework needs to be taken up by the medical profession, especially older medics who may not always understand the implications of their prescribing. “[Improving prescribing] should be [higher on their agenda] because poor prescribing leads to a lot of problems and good prescribing helps keep people fit and healthy and saves money in the long run,” he says.
Encouraging more non-medical prescribers
Non-medics who are training to become independent prescribers need to persuade a medic to act as their designated medical prescriber (DMP). The DMP has a supervisory role, confirming that the trainee has completed the necessary steps to become a prescriber. But for some GPs, training a non-medical prescriber is a step into the unknown and they need incentivising to get involved. “GP practices are businesses and so [they] need to see the value of their investment,” says Hall.
Finding a DMP is one of the biggest challenges to non-medics becoming prescribers, says Duggan, and she believes other experienced prescribers can fulfil this role. To this end, the RPS has called for a change in legislation to enable non-medical prescribers to formally supervise trainees.
Some believe that a dual approach would be better, with trainee prescribers supervised by both a non-medical and medical prescriber, providing a valuable opportunity for multidisciplinary relationship building and medical practice insights. “Part of finding a DMP is about building that relationship,” says Alexander.
“It doesn’t hurt to have a partnership approach,” says Williams, who suggests that pharmacist prescribers would bring a specialist approach, whereas GPs would offer generalist clinician input.
However, Williams acknowledges that there isn’t a huge pool of experienced clinical pharmacists to draw from to act as supervisors to trainee prescribers. “But this is changing over time and so we need the flexibility to allow this,” she adds.
Use of the prescribing competency framework is just one aspect of improving prescribing practice. Prescribers need to be able to learn from their mistakes and to focus on quality improvements in long-term conditions.
The move to increase numbers of non-medical prescribers helps to relieve the burden on GP time and exploit areas of specialism but the main challenge is to ensure prescribing continues to be safe and appropriate. The wide use of the prescribing competency framework can help achieve this.
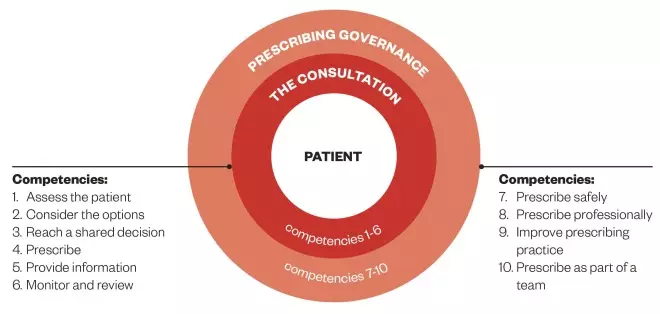
Figure 1: The framework
Source: The Prescribing Competency Framework / Royal Pharmaceutical Society
The competency framework (illustrated above) sets out what good prescribing looks like. There are ten competencies split into two domains — ‘prescribing governance’ and ‘the consultation’. Within each of the ten competency dimensions there are statements that describe the activity or outcomes that prescribers should be able to demonstrate.
Box 1: How the framework was updated
Following a literature review that began in October 2015, the project steering group (23 members including prescribers and patients) concluded that the 2012 framework was broadly fit for purpose. It was revised to reflect the literature review and then passed to a validation group who reviewed the updated framework. The amended draft was put out to public consultation for six weeks. Responses to the consultation, collected from nearly 100 organisations and individuals, were reviewed and incorporated to produce the final framework.
Box 2: Response to framework from other professions
British Dental Association (BDA)
“This new guide provides a useful resource for all prescribers and we’ve welcomed the opportunity to support its development. Armed with this framework, dentists can ensure patients can get the best use from the right medicines, while rising to the challenge of antimicrobial stewardship.”
Russ Ladwa, chair of the BDA’s Health and Science committee
Chartered Society of Physiotherapy
“This multi-professional competency framework is a key document that highlights that prescribing is an important professional function, and that all professionals who prescribe are expected to deliver safe and effective prescribing interventions… [A]ll physiotherapists should use [the framework] when assessing their competency to prescribe.”
Pip White, professional adviser, Chartered Society of Physiotherapy
College of Podiatry
It is comprehensive, user friendly and applicable across the wide spectrum of podiatric practice, from podiatric surgery to diabetes foot care. The growing number of podiatrist independent prescribers working in a variety of fields of practice will find the framework indispensable and ensure the highest standards of prescribing practice are maintained, particularly as practice becomes more complex.”
Matthew Fitzpatrick, consultant podiatrist, chair, medicines and medical devices committee provost, College of Podiatry
The General Optical Council
“We will be considering the framework when looking at the competencies for independent prescribing optometrists as part of our forthcoming education strategic review. Independent prescribing optometrists can complement the work of ophthalmologists by prescribing drugs to manage eye conditions such as glaucoma. We expect more optometrists to be doing this sort of work in the future, which is why it was important that the optical profession was involved in the validation group.”
Marcus Dye, head of education and standards, The General Optical Council
The Society and College of Radiographers
“[The framework] will underpin the outline curriculum frameworks for the Allied Health Professional Prescribers and provide consistency across the professions.”
Christina Freeman, professional officer, The Society and College of Radiographers
References
[1] Royal Pharmaceutical Society. A Competency framework for all prescribers. July 2016. Available at: http://www.rpharms.com/support-pdfs/prescribing-competency-framework.pdf (accessed September 2016).
[2] General Pharmaceutical Council. Prescribers Survey Report. May 2016. Available at: http://www.pharmacyregulation.org/sites/default/files/gphc_prescribers_survey_report.pdf (accessed September 2016).


