Images from Shutterstock.com
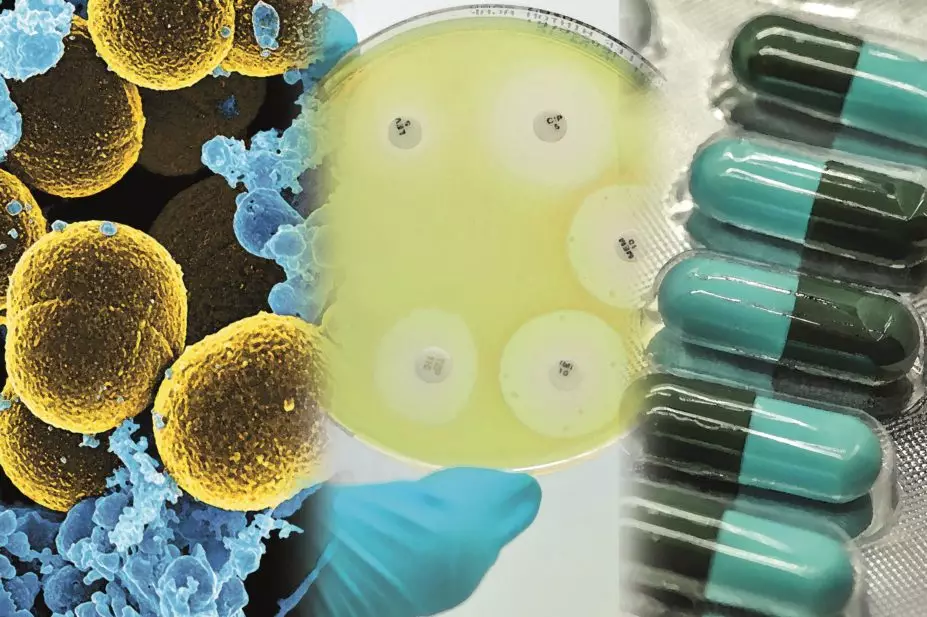
When it comes to tackling infections, we’ve had it pretty good for the past 90 years. The development of antibiotics has turned many previously deadly infections into mere inconveniences, but it couldn’t last forever. Slowly, bacteria have fought back, developing resistance to many of the most effective drugs. In the United States alone, around 2 million people are infected with resistant strains of bacteria each year, and at least 23,000 of these patients die.
“We’re at the end of the first antibiotic era,” says Lloyd Czaplewski, founder of Chemical Biology Ventures, an R&D consultancy based in Oxfordshire. “There might not be any new classes of drugs to discover.”

Courtesy of Lloyd Czaplewski
Lloyd Czaplewski, founder of Chemical Biology Ventures, an R&D consultancy based in Oxfordshire, says there might not be any new classes of antibiotics to discover
New ideas are needed. And while most researchers and pharmaceutical companies have all but given up on developing new antibiotics, work is racing ahead on alternative therapies, with an aim to extend the life of existing drugs, or replace them altogether.
In January 2016, Czaplewski and his colleagues published a review of the alternatives currently under investigation, and found at least 19 different approaches, of which they decided 10 should be given top priority (see ‘Table 1: Ten alternatives to antibiotics that should be given priority’)[1]
.
While traditional antibiotics work by targeting important bacterial pathways, like protein synthesis, or by killing the bugs directly, the alternative techniques take more subtle approaches. These range from the familiar — such as using antibodies to bind the pathogen or its virulence factors to inactivate or mark them for destruction — to more creative ideas, such as engineering viruses to attack harmful bacteria in the body. Other approaches include outcompeting the harmful bacteria with helpful probiotics, antibacterial vaccines, and enhancing the body’s own immune system.
“Any one of these approaches could work,” says Czaplewski. “It’s a grand experiment.”
But it is not a cheap one. Czaplewski and his colleagues estimate that it would cost around £1.5bn over ten years to advance all of the alternatives on their list to at least the level of phase II clinical trials.
Promising leads
Alan Hauser, a microbiologist at Northwestern University in Chicago, says the most promising alternative is the use of monoclonal antibody-derived therapeutics to combat infectious agents. “The medical field has lots of experience with using antibodies,” he says. “They work well and are relatively safe.”
The medical field has lots of experience with using antibodies — they work well and are relatively safe
To fight bacteria, one option is to use an antibody that recognises a toxin secreted by those bacteria. The antibody neutralises the toxin so the bacteria can no longer use it to cause infection, giving the body’s immune system and conventional antibiotics time to mop up the bacteria.

Courtesy of Alan Hauser
Alan Hauser, a microbiologist at Northwestern University in Chicago, says the most promising alternative to antibiotics is monoclonal antibody-derived therapeutics
One such antibody is already in use — GlaxoSmithKline’s raxibacumab was approved in 2012 to treat inhaled anthrax. It works by blocking a receptor on the surface of the host cell, preventing one of the three parts of the anthrax toxin — the protective antigen — from binding. There are six other points in the toxin’s pathway that offer opportunities to disrupt infection, and antibodies are being developed for each[2]
.
Researchers are also working on developing small molecule drugs that can do the same thing, which would have some advantages over antibodies, says Hauser. “They can often be given orally rather than injected, and once you have a lead compound, there are chemical techniques available to boost its efficacy,” he says.
Other techniques are further away down the pipeline but have potential, Hauser adds. For example, harnessing nature’s own antibacterial weapon, bacteriophages — viruses that attack bacteria.
Bacteriophages are an old technique, from before the age of antibiotics, which are becoming popular again and are already being used in Eastern Europe to treat infections in surgical wounds or burns, says Czaplewski. Phages are perfect bacteria-killing weapons; they hijack the bacterial host cell’s own machinery to make more of themselves, so when an infection is at its worst there are lots of phages being made. As the bacteria die out, the phages disappear. They are also tuned to attack just their target bacterial cells, so have no chance of infecting the human host.
That specificity is also one of their downsides though — many phages can only infect a single species, or even strain, of bacteria. This means patients must often take cocktails of several different phages to ensure that at least one will be able to target their infection. And a cocktail that works against a local strain of bacteria found in one country or city might not work in another.
The idea of putting viruses into people meets with resistance — people don’t like the idea
The concept can also put patients off, says Hauser. “The idea of putting viruses into people meets with resistance — people don’t like the idea.”
Vincent Fischetti, a microbiologist at Rockefeller University in New York, is working on a phage-based therapy that could avoid some of those issues. Rather than using a live phage, he uses just the phage lysins — the small proteins that viruses use to break out of bacterial cells. “[Lysins] go into the cell wall and cleave the peptidoglycan layer, causing the cell to explode,” he says. “They’re highly efficient, only a tiny amount is needed.”
Courtesy of Vincent Fischetti
Vincent Fischetti, a microbiologist at Rockefeller University in New York, is working on a phage-based therapy that uses lysins, small proteins that viruses use to break out of bacterial cells
Lysins are also able to work more broadly than a bacteriophage — generally just one will be effective against all strains of a particular species of bacteria. But so far they are mostly effective against Gram-positive bacteria. Gram-negative species, with their stronger cell walls, are proving to be a tougher nut to crack.
Fischetti says the lysins could be used on their own eventually, but for now he is testing them in combination with traditional antibiotics. When used together, the lysins allow the antibiotic dose to be five to ten times lower[3]
. Fischetti has just completed a successful phase I trial, and will be starting phase II work by the end of 2016.
Self defence
Another alternative approach to antibiotics involves boosting the body’s own ability to defend itself. Bob Hancock, an immunologist at the University of British Columbia in Vancouver, is working on stimulating the immune system to fight off bacterial infections. This strategy works in much the same way as a vaccine; doctors can take a bacterium that commonly causes an infection, kill it and use it as the therapy. It was initially thought that this process would create antibodies to the specific bacteria used, but it appears to boost the immune system in general, allowing the body to fight off other infections as well, including viral infections. This treatment has already been used successfully in Latin America for respiratory infections, says Hancock[4]
.

Source: Courtesy of Bob Hancock
Bob Hancock, an immunologist at the University of British Columbia in Vancouver, is using host defence peptides to boost the immune system
“Certain bacterial products are strongly recognised by the immune system,” he says. “Just having those molecules there is enough to stimulate it.”
Certain bacterial products are strongly recognised by the immune system — just having those molecules there is enough to stimulate it
Hancock’s work uses small, naturally occurring proteins called host defence peptides that can selectively boost the immune system, stimulating protective immunity while dampening down the inflammatory response. “You get the good part of the immune system without the potentially dangerous part — inflammation,” he says.
The research is still in the pre-clinical stage[5]
, but Hancock is working with partners to develop it commercially as an adjunct to support conventional antibiotics.
Hurdles ahead
While Hancock’s immune stimulants seem to be effective against a wide range of bacteria, as well as viruses and some parasitic diseases like malaria, the majority of antibiotic alternatives are like phage therapy — a narrow spectrum treatment specific to a single species or strain.
Narrow spectrum is better because there is less effect on the helpful gut flora, as long as the diagnostics can keep up with demand
But this can have advantages, says Fischetti. “We’re trying to get away from broad activity. Narrow spectrum is better because there is less effect on the helpful gut flora. As long as the diagnostics can keep up with demand,” he says.
However, so far those diagnostics are not up to scratch, says Czaplewski. “For a serious respiratory tract infection, you’d need about 18 diagnostic tests to cover the spectrum of possible bugs,” he says. “We don’t have them yet.”
This makes it hard for companies to justify working on targeted therapies because it is difficult to prove efficacy to regulators. Czaplewski gives the example of a highly targeted antibody that Roche was developing for Pseudomonas aeruginosa, a common hospital acquired infection, but eventually gave up on because it could not see a clear regulatory pathway to get a targeted product to market. “If Roche can’t do it, a lot of these approaches will be called into question until the need is so great that the regulatory approach changes,” he says.
Learning from the past
These new techniques also have to find ways to deal with the very problem that made them necessary in the first place — resistance. This is not an issue for some, like Hancock’s immune-boosting techniques, because they do not attack the bacteria directly, but “if there is a selection pressure, resistance will develop,” says Czaplewski.
This means we need to be smarter about how the new drugs are used to try and avoid the mistakes that allowed resistance to gain a foothold against traditional antibiotics. Better diagnostics that allow doctors to target specific bugs, and therapies that use a variety of approaches to attack an infection from multiple angles, will help to minimise the risk of resistance developing to the new treatments, says Hauser.
If some of these novel approaches were available, they would already be used
These hurdles are certainly surmountable with a little hard work, but will we be able to do it in time? “We could have used them yesterday,” says Hauser. “If some of these novel approaches were available, they would already be used.”
Hauser says it is hard to predict when the new techniques will be ready to use. Many haven’t yet started clinical trials, or have only reached phase I. But even if they prove successful, it may take years to get through phase III trials and gain regulatory approval.
Nonetheless, projects to deal with antibiotic resistance are beginning to take shape, as governments and philanthropic funders start to look for ways to speed up the development of new antimicrobial drugs. For example, on 29 July 2016, CARB-X, a public-private partnership backed by the US government, the UK’s Wellcome Trust, and the UK R&D Centre for Antimicrobial Resistance, announced plans to mobilise US$350m over the next five years to develop new drugs, vaccines and diagnostics.
And while this sort of commitment offers a glimmer of hope, Czaplewski says this will not be enough. “We need a very different approach, we’re not going to fix [antibiotic resistance] in the next five years. We need to put together a process so there are still medicines available in 100 years.”
Ultimately, Czaplewski says a new model is needed to make the discovery and development of these new drugs less risky for companies to take on and to ensure longevity. He likens the process to other large-scale international projects, like the Large Hadron Collider (LHC) or the International Space Station (ISS), where thousands of scientists work for decades, spending huge sums of money without creating any direct product. “The LHC has so far cost around £6bn, and the ISS almost £100bn” he says. “Antibiotic resistance probably needs an investment somewhere between the two.”
| Strategy | Mechanism | Probable use | Anticipated first registration |
|---|---|---|---|
| Source: Czaplewski L, Bax R, Clokie M et al. Alternatives to antibiotics — a pipeline portfolio review. Lancet Infect Dis 2016;16:239–251. doi: 10.1016/S1473-3099(15)00466-1 | |||
| Antibodies | Antibodies that bind to and inactivate a pathogen, its virulence factors, or its toxins | Prevent gram-positive and gram-negative infection; possibly adjunct use | 2017 |
| Probiotics | Live micro-organisms that outcompete harmful bacteria when administered in adequate amounts | Prevent or treat Clostridium difficile-associated diarrhoea or antibiotic-associated diarrhoea | 2018 |
| Lysins | Enzymes used by bacteriophages to destroy the cell wall of a target bacterium | Treat gram-positive infection | 2022 |
| Wild-type bacteriophages | Viruses that infect and kill bacteria | Treat gram-positive and gram-negative infection | 2023 |
| Engineered bacteriophages | Genetically engineered viruses with new properties to infect and kill bacteria | Treat gram-positive and gram-negative infection | 2023 |
| Immune stimulation | Innate proteins or bacterial extracts that boost the immune system | Prevent or provide adjunct therapy for gram-positive and gram-negative infection | 2021 |
| Vaccines | Inactivated bacteria or bacterial proteins that stimulate the immune system | Prevention, gram-positive more than gram-negative infection | 2019 |
| Antimicrobial peptides | Small proteins that have direct antibacterial activity | Treat or adjunct for gram-positive and gram-negative infection | 2022 |
| Host defence peptides and innate defence peptides | Peptides that increase expression of anti-inflammatory chemokines and cytokines, and reduce expression of pro-inflammatory cytokines | Adjunct for gram-positive and gram-negative infection | 2027 |
| Antibiofilm peptides | Peptides that specifically inhibit bacterial biofilm formation | Adjunct for gram-positive and gram-negative infections | 2027 |
References
[1] Czaplewski L, Bax R, Clokie M et al. Alternatives to antibiotics — a pipeline portfolio review. Lancet Infect Dis 2016;16:239–251. doi: 10.1016/S1473-3099(15)00466-1
[2] Hauser AR, Mecsas J & Moir DT. Beyond antibiotics: new therapeutic approaches for bacterial infections. Clin Infect Dis 2016;63:89–95. doi: 10.1093/cid/ciw200
[3] Daniel A, Euler C, Collin M et al. Synergism between a novel chimeric lysin and oxacillin protects against infection by methicillin-resistant Staphylococcus aureus. Antimicrobial Agents and Chemotherapy 2010;54:1603–1612. doi: 10.1128/AAC.01625-09
[4] Del-Rio-Navarro BE, Espinosa-Rosales FJ, Flenady V et al. Immunostimulants for preventing respiratory tract infection in children. Cochrane Review 2012;7:629–717. doi: 10.1002/ebch.1833
[5] Hancock REW, Haney EF & Gill EE. The immunology of host defence peptides: beyond antimicrobial activity. Nature Reviews Immunology 2016;16:321–334. doi: 10.1038/nri.2016.29