Courtesy of The Lancet
The cost of providing a basic set of 201 essential medicines to all people in low and middle-income countries could be as little as US$1–US$2 per person per month, according to the first analysis of the cost of providing a basket of essential medicines by The Lancet Commission on Essential Medicines.
Based on disease prevalence, consumption of medicines and medicines prices, the commission estimated that the cost of providing these 201 medicines from the World Health Organization’s model list of essential medicines to the total populations of low and middle-income countries is between $77.4bn and $151.9bn per year or the equivalent of $12.90–25.40 per person per year.
The commission brings together a group of 21 international experts. It reports the first cost analysis of providing a basket of essential medicines, and presents a series of recommendations aimed at governments, civil society, national health institutions, national medicines regulatory agencies and the pharmaceutical industry.
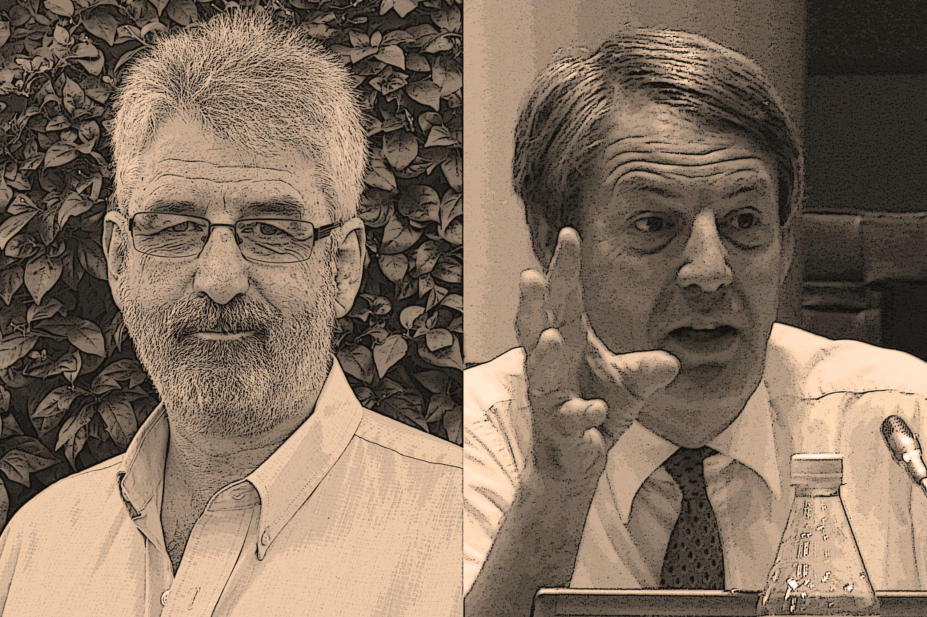
Andy Gray, a pharmacist, is senior lecturer at the division of pharmacology, University of KwaZulu-Natal, in Durban, South Africa. Hans Hogerzeil is professor of global health at Groningen University, the Netherlands, and a former senior World Health Organization (WHO) official. From 1999 to 2008 he was secretary of the WHO Model List of Essential Medicines and from 2004 to 2011 was WHO director for essential medicines in Geneva.
What are the key findings of The Lancet Commission?
Gray: The Lancet Commission takes a comprehensive view of essential medicines, not only looking at issues, for example, research and innovation and missing essential medicines, but covers the entire gamut, including the financing of essential medicines, their affordability, policy of medicines and how they are used appropriately or inappropriately.
We present, for the first time, an estimate of what it would cost to provide 201 basic essential medicines to the entire populations of low and middle-income countries, and we show that, for between US$1–US$2 per person per month, you can provide that basic set of medicines. That is more than what is being spent at the moment in low-income countries, and less than what is being spent in perhaps a quarter of middle-income countries. There is the means, but not the willingness. What we really need is social solidarity to provide for those who can’t pay for themselves, but also greater efficiency to meet the needs of everyone.
How do you close the gap to ensure the United Nations sustainable development goals target to have universal health coverage by 2030 is met?
Gray: It’s absolutely critical that, to have meaningful universal health coverage, there is access to medicines in that benefit package. If left alone, governments are not going to be able to do that. The price of new medicines, the price of medicines needed to treat conditions, such as cancer, other non-communicable diseases, and of emerging infectious diseases, is going to be impossible for those systems to be sustainable. So they have to engage in rational selection, appropriate interventions on pricing, and ensure appropriate use of those medicines for universal health coverage to be sustainable.
Hogerzeil: There are two aspects. On the one hand we say clearly for sustainable development goals and universal health coverage there’s no way you can do this without medicines, and on the other, we say there’s no way the market is going to do it. So you need active government intervention and payment for the poorer segment. Building up universal health coverage in the next 15 years cannot be done without government and it cannot be done without medicines.
Universal health coverage cannot be achieved without medicines
Do the estimates that you make in the report factor in the real cost of the delivery of the medicines, such as the logistics and the delivery by health personnel?
Gray: The figures in our report are costs for the medicines themselves, with an estimate of what it would cost for quality assurance and some logistics. We don’t cover health workers’ salaries or other deliverables, such as diagnostic tests or health facility costs.
The report highlights that many new medicines, such as antivirals for hepatitis C, are costly. How do you resolve this problem?
Gray: That’s one of the key issues we highlight: that the system of innovation, which is based entirely on patent protection and monopoly pricing, is never going to be sustainable. It’s not going to develop medicines that we need, but it’s going to create the very problems that we see now with the antivirals. Governments do have options – they can intervene Trade-Related Aspects of Intellectual Property Rights (TRIPS) flexibilities (an international agreement administered by the World Trade Organization), they can use the full gamut of pricing interventions and they can also procure in ways which are more active than just relying on markets to set those prices.
But what we also need is greater transparency. The sort of differentials that we see between the list prices in the higher- and middle-income countries, and the very low prices that have been made available in places such as Egypt, just show that there is simply no logic to the prices that are being demanded at the moment.
Hogerzeil: It is a public policy failure, rather than market failure, to rely on the markets to provide essential medicines when we need them for the poor or for people living in poor countries. The pharmaceutical industry doesn’t see that as a sufficiently interesting investment, and simply doesn’t do it. For example, a one-day treatment for malaria would be useful, as would shorter treatments for tuberculosis (TB), or new treatments for multi-drug resistant TB. These are some examples where you have missing essential medicines. And unless governments interfere, we’re simply not going to get them.
In the meantime, we have, of course, some essential medicines, such as antivirals for hepatitis C, that have entered the market and have fallen in the hands of financial mechanisms and are totally overpriced. It’s good news that, in Egypt and other places, it’s down to a few hundred dollars. But it shows how ridiculous it is that the special negotiated price in the Netherlands is €55,000 for one box of antivirals for hepatitis C. In France, its use has had to be rationed, so it is just give to patients with final stages of the disease. In 2015 it was not going to spend more than €450m on it, and this year not more than €750m. This shows how the system has derailed.
It is a public policy failure to rely on the markets to provide essential medicines
One of your proposals is to have routine monitoring of affordable pricing and availability. How realistic is this given that the reporting of countries in many international fora are lagging behind?
Gray: What we try to get across is that you can’t intervene without data, and you can’t manage your medicine budget appropriately without knowing what you’re paying and where it’s going to. You also need to be tracking the progress of equity, so you need to have disaggregated data looking at particular key populations that are relevant to your own country. So investment in systems and institutions is not only important in terms of providing global availability in pricing data. That will be absolutely crucial to the ability of universal health coverage schemes to be able to manage that fund for your core budget.
Do you anticipate impediments in pursuit of such data given that, often, companies use the commercial confidentiality criteria to shield access to this kind of information?
Gray: Yes. Right through the report you will see a commitment to increase transparency. Be that of pricing information or in medicines regulatory practices, we see the barriers that are thrown up. The European Medicines Agency is fighting two court cases in Europe at the moment surrounding its transparency efforts. But the trend of history and public policy is towards greater transparency. We think that’s really important. We’ve seen how effective it’s been in the Global Fund’s databases, for example. It’s crazy that, in many parts of the world, we don’t actually know what the drug prices are. We know, for example, that there is some sort of discount offered for hepatitis drugs in the United States but that’s a secret deal between pharmaceutical benefit companies and the manufacturers. We don’t know where the savings are and how much of that is passed on to the consumer.
What are your main messages to the global health community and the pharmaceutical industry?
Gray: We call on the pharmaceutical industry to contribute positively by being more transparent, thinking about its social obligations and playing an appropriate role as a global citizen. We look at civil society and say it should be holding governments accountable and contributing in many areas, including safety monitoring, pricing availability monitoring and engagements in medicines regulatory affairs.


