Michele Zuliani / Alamy
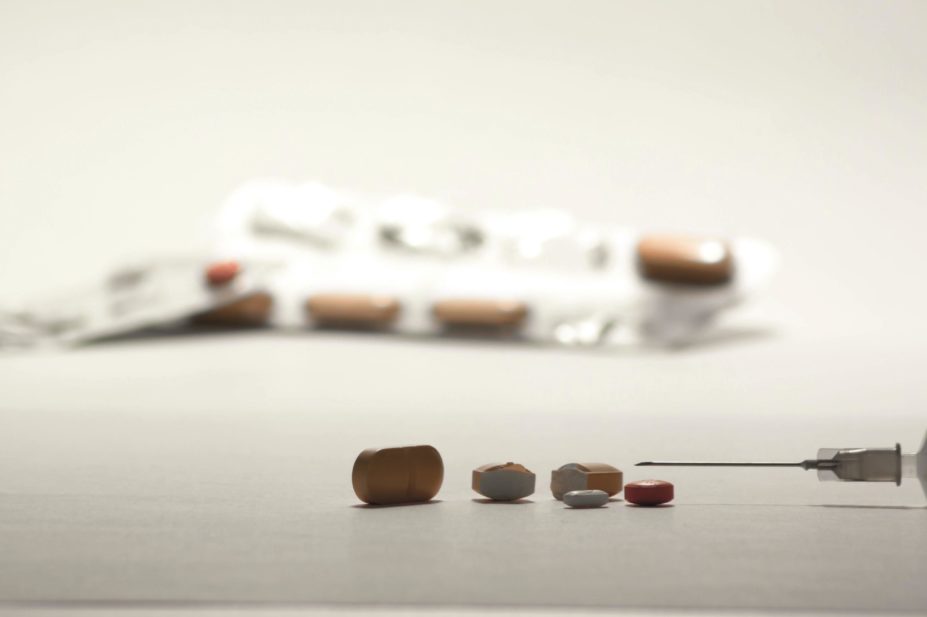
Prescription medicines can be a powerful life saving tool, but they carry with them a danger of abuse. The euphoric effects of prescription painkillers, as well as stimulants and drugs designed to treat anxiety and trouble sleeping, can encourage some people to use them recreationally, with potentially fatal results. Others who start using these drugs therapeutically can go on to become addicted.
The problem is a huge one. In the United States, drug overdoses are the leading cause of accidental deaths, eclipsing even car accidents. And the UK joins the United States in the grim statistic that overdose deaths from prescription opioids outnumber those from heroin and cocaine combined. A variety of approaches are being used to tackle the problem, including educating prescribers, monitoring prescriptions, introducing drug formulations that are tough to abuse and, ultimately, treating addicted individuals.
Several different classes of prescription drugs are commonly abused, says Doug Throckmorton, deputy director of regulatory programs at the US Food and Drug Administration (FDA). These include depressants — for example, benzodiazepines such as diazepam (Valium) and alprazolam (Xanax), used to treat anxiety — and stimulants — for example, the combination of amphetamine and dextroamphetamine (Adderall), and methylphenidate (Ritalin or Concerta), prescribed for attention deficit hyperactivity disorder.
But by far the most widely abused, and dangerous, drugs are opioid painkillers, such as hydrocodone (Vicodin) and oxycodone (Roxicodone). Slow-release oxycodone tablets, such as OxyContin, contain a huge amount of the drug, and so account for a disproportionate number of overdoses and deaths, says Throckmorton. They take up most of the agency’s attention. “Prescription opioids have been our focus for several years,” he says.
Global prevalence
While prescription opioid abuse is widespread, it is particularly prevalent in North America and Australia, according to Kamran Niaz, an epidemiologist at the United Nations Office on Drugs and Crime. The annual prevalence of abuse of opioid painkillers in the population is greater than 5% in the United States and more than 3% in Australia; across most of Europe it is well below 1%. Although there are indications that opioids are also being abused in Asia and Africa, Niaz adds, there is not yet any good data on the prevalence.
“The extent of misuse of prescription opioids in Europe is not in any way comparable to North America,” says Niaz. In contrast, rates of heroin use are roughly the same on both continents.
The extent of misuse of prescription opioids in Europe is not in any way comparable to North America
“We haven’t got a huge problem with misuse and diversion of opioids in the UK, with the possible exception of tramadol,” agrees Catherine Stannard, a consultant in pain medicine at Southmead Hospital in Bristol. Tramadol was, until recently, widely prescribed for fairly minor pain in the UK, and was sold over the counter in some parts of Europe.
In contrast, prescription drug abuse in the United States is so bad that the Centers for Disease Control and Prevention have described it as an ‘epidemic’ in the country.

Catherine Stannard, a consultant in pain medicine at Southmead Hospital in Bristol, says prescription drug misuse is not a huge problem in the UK.
Part of the discrepancy between North America and Europe is to do with how commonly the drugs are prescribed. Canada and the United States lead the world in per-capita consumption of prescription opioids — the United States alone, with 5% of the world’s population, uses more than 80% of the world’s oxycodone and 65% of the hydromorphone (Palladone).
Differences in prescribing practices also play their part. Weaker regulatory restrictions, higher patient demand for ‘effective treatment’, and a more pronounced for-profit organisation of healthcare in North America, particularly the United States, may have exacerbated the problem in this region[1]
. In contrast, tighter control and surveillance over prescriptions in the UK’s NHS has probably kept the problem from reaching the same level, says Stannard.
Doctors’ greater flexibility and willingness to prescribe medications open to abuse in the United States is reflected in the way most people obtain these drugs. Rather than getting them from illegal dealers, most of the drugs that are abused are prescribed legally and then diverted elsewhere, as friends or family members share them or leave them unguarded in medicine cabinets. This is particularly true of young people, who are at the highest risk of starting to abuse prescription drugs.
Most do not pay, three-quarters of adolescents and young adults get them free from their friends
“For adolescents, the primary source is friends and relatives,” says Carol Boyd, who studies prescription medicine abuse at the University of Michigan in Ann Arbor. “Most do not pay, three-quarters of adolescents and young adults get them free from their friends.”
Educating prescribers
Carol Boyd, of the University of Michigan in Ann Arbor, says most adolescents who abuse prescription drugs obtain them from friends or relatives.
Boyd’s research has found that when young people are prescribed controlled medications legally, their risk of going on to abuse those drugs goes up dramatically — by as much as 12-fold in the case of sleep medications[2]
. For this reason, she feels that a large part of the responsibility for preventing abuse falls upon prescribers.
“Every prescriber should tell their patients four things,” she says. “How to take the drug properly, to beware of people asking them to share, to control and count their pills, and to dispose of them correctly. But not enough of them do it.” Even if they do, of course, it is then up to the patients to follow that advice.
Throckmorton says that educating doctors is one of the FDA’s main priorities in its efforts to fight prescription drug abuse. In 2012, the agency introduced a requirement that the manufacturers of slow-release opioids make educational materials available to doctors and patients. So far around 20,000 prescribers have taken educational courses, and the FDA hopes to increase that number to around 80,000 this year. “Education is critical,” he says. “We want to get the best information to the doctors so they decide who’s going to benefit from these drugs, and who’s going to be potentially placed at risk of harm by using them.”
But regulators and doctors need to strike a balance between keeping the drugs away from those who might abuse them, and ensuring that they are available for patients who genuinely need them. Regulations, according to Boyd, run up against “a quality of life issue”. She says: “I would never want patients to not have access to these medications.”

Rebecca Haffajee, a pharmaceutical policy researcher at Harvard Medical School, Boston, says there is patchy evidence that prescription drug monitoring programmes reduce overprescribing.
Governments can also help doctors prescribe more wisely by setting up prescription drug monitoring programmes, says Rebecca Haffajee, a pharmaceutical policy researcher at Harvard Medical School, Boston, Massachusetts. These are electronic systems that can show doctors, pharmacists and law enforcement officials what a patient has been prescribed over the past three to six months, who prescribed it, how many times a prescription has been refilled and other data.
There is some patchy evidence from the United States that such systems can reduce overprescribing, but getting doctors on board is tricky. Drug monitoring programmes are usually separate from other e-health records, and often have clunky or slow user interfaces. Every state except Missouri has a system in place but participation rates are only around 35%, says Haffajee. Even in the 22 states where the programmes are mandatory, opposition from doctors — who, says Haffajee, “don’t like to be told what to do” — often delays full implementation[3]
.
Deterring abuse
Another approach is to make the drugs themselves harder to use improperly. Stamford, Connecticut-based Purdue Pharma, which makes the often-abused painkiller OxyContin, was the first to add an ‘abuse deterrent formulation’ to its pills in 2010. The new pills are harder, so they can no longer be ground into a fine powder that can be snorted, and include a polymer that turns to gel when mixed with water, so they cannot be drawn into a syringe. Several other companies have since followed suit.
“It’s not a silver bullet, but current abuse-deterrent properties can make it difficult for novice users to snort or inject opioids,” says Dan Cohen, chair of the Abuse Deterrent Coalition in Washington, DC, an alliance of drug companies and patient groups that is pushing for regulations that would make abuse-proof formulations mandatory.
Cohen likens the situation to that of car safety in the 1950s, with companies introducing safety technologies such as seatbelts that the government eventually adopted as standard. “They’ve started the whole safety paradigm in the right direction,” he says.
Already, the FDA has announced that generic versions of OxyContin cannot be sold without abuse-deterrent properties, and it looks like Health Canada is about to do the same. To clarify the situation for the pharmaceutical industry, in April 2015 the FDA released guidelines on how it will evaluate abuse deterrence, so that companies can put the claims on their labels. “I would like the majority of opioids to have abuse-deterrent formulations as soon as possible,” says Throckmorton.
I would like the majority of opioids to have abuse-deterrent formulations as soon as possible
So far, there is no technology that can prevent someone from getting high just by swallowing a handful of pills, but it is on the horizon, suggests Cohen. It will probably involve adding a ‘prodrug’ that will only activate the main ingredient when in the presence of a certain intestinal enzyme, he says. To combat excessive pill-popping, it will also contain a small amount of a compound that inactivates that enzyme — if too many pills are taken at once, there will be enough of the compound to shut down the reaction. A California-based company, Signature Therapeutics, is currently working on developing prodrug-protected pills.
Drugs against drugs
But no matter how much effort is put into stopping abuse, it will be impossible to crack down on it completely, and some people will become dependent on, or addicted to, prescription drugs. The best way to treat addiction is with medication, says Kelly Clark, president-elect of the American Society of Addiction Medicine in Chevy Chase, Maryland, but there are not many medications available.
“In the United States, there is only one prescribed drug class for which there are FDA-approved medications to treat addiction, and that’s the opioids,” she says. “We don’t have any medications to treat benzodiazepine addiction, or stimulant addiction, or the other kinds of drugs of abuse.”
And these medicines are hard to access. In the United States, the opioid replacement therapy methadone can only be administered at specialised clinics, and doctors are limited in the number of patients they are allowed to treat with a combination of opioid replacement therapy buprenorphine and opioid antagonist naloxone (Suboxone). In much of Europe, methadone is also tightly controlled, but it can be provided in community pharmacies rather than special clinics.
Many of the private clinics in the United States that treat addiction are also philosophically opposed to using drugs to help fight addictions, preferring to rely on 12-step type programmes that focus on willpower and behavioural change. But Clark says that approaches like these that can be successful for alcohol addiction simply do not work for drugs like opioids. Relapse rates after short detox treatments are greater than 90% within a week, and longer rehabilitation courses are similarly unsuccessful, according to Clark.
Addiction is a chronic brain disease, and needs to be treated that way
“They are not embracing the evidence,” she says. “Addiction is a chronic brain disease, and needs to be treated that way.”
Levelling off
Despite all these hurdles, it looks like the United States is slowly getting its prescription drug abuse epidemic under control. The number of overdose deaths from prescription drugs has levelled off since 2011, and seems to be on the decline.
Overdose deaths from some opioid painkillers also seem to have plateaued in the UK in the past few years, but the overall picture is less rosy. For example, deaths from tramadol overdose have seen a sharp increase. But there have been moves to get it under control. Tramadol was recently reclassified in the UK, which Stannard hopes will lead to more careful prescribing and a drop in the number people misusing it. “The rescheduling of tramadol seems to have given some people pause,” she says.
Throckmorton is also hopeful. “The evidence is that the general trend [in the United States] is going in the right direction,” he says. The trick now, though, is to determine which of the myriad different interventions put in place by various groups around the country are having the biggest effect, so that they can be expanded and less successful ones scrapped or adjusted.
It may be too soon to celebrate though. As prescription opioids gained popularity among drug users over the past decades, rates of heroin use plummeted. But now, as authorities have cracked down, and prescription drugs such as OxyContin have become harder to get hold of and abuse, heroin is making a big comeback. The number of heroin overdose deaths in the United States increased fivefold between 2001 and 2013. “As opioid use has declined, opiate use in the form of heroin has increased,” says Boyd. “We are seeing an epidemic of heroin problems now.”
References
[1] Fischer B, Keates A, Bühringer G et al. Non-medical use of prescription opioids and prescription opioid-related harms: why so markedly higher in North America compared to the rest of the world? Addiction 2014;109:177–181.
[2] Boyd CJ, Austic E, Epstein-Ngo Qet al. A prospective study of adolescents’ nonmedical use of anxiolytic and sleep medication. Psychology of Addictive Behaviours 2015;29:184–191.
[3] Haffajee RL, Jena AB, Weiner SG. Mandatory use of prescription drug monitoring programs. JAMA 2015;313:891–892.


