Nick Lowndes / Ikon Images
As a lead pharmacist in HIV and sexual health, Claire Richardson uses her independent prescriber (IP) qualification to prescribe everything her patients need — from antiretroviral drugs to medicines to manage side effects.
“It’s just brilliant to be able to have that consultation with a patient, make those decisions with them and then just say, ‘here you go’. I don’t have to ask someone else to do that for me or get someone to approve it,” explains Richardson, who is based in a specialist HIV centre at the Royal Sussex County Hospital.
“It really improves the patient experience and patient flow — it reflects well on pharmacists too. Patients don’t really question it, they accept us as part of the clinical team,” she says.
But Richardson’s experience does not reflect that of all pharmacists. Just 11% (6,188) of the General Pharmaceutical Council’s (GPhC) 55,275 registrants are independent prescribers (as of 26 February 2018) and not all of these are using their qualification.
In a survey carried out by The Pharmaceutical Journal in 2017, 17% of 255 independent prescribers who responded said they have never prescribed and 16% said they use their qualification no more than once a month. Another survey, carried out by the GPhC in 2016, found that of 648 respondents, 11% had never prescribed and 27% found it either difficult or very difficult to find opportunities to prescribe[1]
.
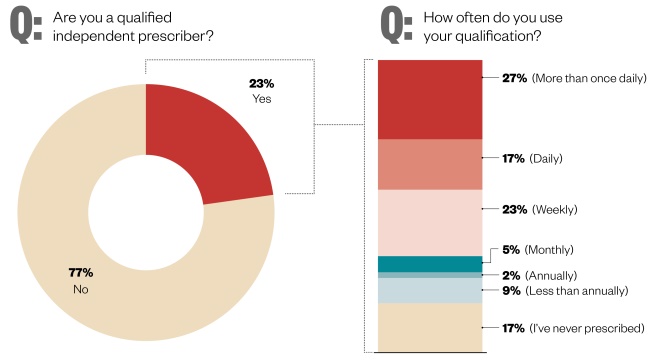
Figure 1: Independent prescribers and how often they use their qualification
Source: The Pharmaceutical Journal
In a survey carried out by The Pharmaceutical Journal in 2017, 17% of 255 independent prescribers who responded said they had not prescribed at all since receiving their qualification
These data raise questions about how barriers to pharmacist independent prescribing can be removed.
A short history
Supplementary prescribing for pharmacists was introduced in 2003 following publication of the NHS Plan 2000, which set out a policy on non-medical prescribing to improve patient care[2]
. The supplementary prescribing qualification enables pharmacists to prescribe a number of medicines within the context of a patient-specific clinical management plan agreed by a doctor.
The pharmacist independent prescriber (PIP) role was created in 2006, although it excluded controlled drugs until 2012. As the then regulator, the Royal Pharmaceutical Society (RPS) of Great Britain accredited conversion training courses to allow pharmacists qualified as supplementary prescribers to become independent prescribers, enabling them to prescribe without the need to consult a doctor.
Currently, there are 45 providers of PIP programmes across Great Britain, accredited by the current regulator, the GPhC.
In order to apply for a programme, pharmacists must have at least two years’ experience in a patient-facing role and an assigned designated medical practitioner to support their training. Once qualified, PIPs can only prescribe within their chosen area of competency.
To apply for a PIP programme, pharmacists must have at least two years’ experience in a patient-facing role
Healthcare professionals who can qualify as non-medical prescribers include pharmacists, nurses, optometrists, physiotherapists, radiographers and podiatrists, and this may soon be extended to paramedics.
According to Heidi Wright, practice and policy lead for RPS in England, funding for PIP training places in England is being made available via the Pharmacy Integration Fund (PhiF) and is linked to supporting pharmacists to undertake new roles working in general practice, care homes, NHS 111, integrated urgent care centres and care homes.

Source: MAG / The Pharmaceutical Journal
Practice and policy lead for the Royal Pharmaceutical Society in England Heidi Wright says that funding for PIP training places in England is being made available via the Pharmacy Integration Fund
A new training pathway has also been commissioned in collaboration with Health Education England (HEE) for GP practice pharmacists and care-home pharmacists. As part of the training pathway, pharmacists will become PIPs if they are not already qualified.
The Scottish Government’s nine-point plan, ‘Achieving excellence in pharmaceutical care: a strategy for Scotland’, promises to target resources in order to expand the number of community pharmacists undertaking independent prescriber training to aid the ongoing success of the minor ailment scheme[3]
. It also committed to providing more technological support for existing prescribers in primary and secondary care.
The Welsh Government is also supportive of non-medical prescribing and has committed to developing policies that will enable its expansion in the country[4]
.
In 2016, the RPS updated thePrescribing Competency Framework for all prescribers in collaboration with the other prescribing professions in the UK. The updated framework, which was originally published by the National Institute for Health and Care Excellence in 2012, has been restructured and now reflects the increasing prevalence of multiple comorbidities and number of non-medical prescribers.
Breaking down barriers
To encourage more pharmacists to become independent prescribers, the GPhC plans to launch a consultation in mid-March 2018 to examine the education and training of PIPs.
Among the proposals are changes to the prerequisite entry requirements for training and the introduction of general learning outcomes. The GPhC is also suggesting revisions to the educational supervision requirements for PIPs in training, from a designated medical practitioner to a designated prescriber practitioner.
“If a trainee thinks that being supervised by a doctor would be most helpful to them then they should be supervised by a doctor, but if they feel that a pharmacist would be more appropriate, that would be an option,” explains Damian Day, head of education at the GPhC.

Source: General Pharmaceutical Council
Damian Day, head of education at the GPhC, hopes that changing the educational supervision requirements for PIPs in training will break down some of the barriers to more pharmacists becoming independent prescribers
“Giving this responsibility to practising PIPs would also give them the opportunity to train the next generation and share their experience in the workplace,” he adds.
Giving this responsibility to practising PIPs would give them the opportunity to train the next generation and share their experience in the workplace
It is hoped that making this change will break down some of the existing barriers to more pharmacists becoming IPs.
Some of these barriers were highlighted in the GPhC’s 2016 survey — both to carrying out the training to become an IP and to using the qualification once trained. They include: an absence of support from other healthcare professionals and managers; a lack of understanding about the role of PIPs; and a limited amount of funding and financial incentive available for pharmacists to train and then to offer the service in their day-to-day practice. Respondents also cited a lack of confidence in diagnosing conditions and a lack of time and interest invested by their designated medical practitioner.
Sectorial differences
A recent report from researchers at the University of Nottingham school of pharmacy highlighted the value of having community PIPs (CPIPs) relieve pressure on GPs and primary care teams.
However, a key challenge identified by the researchers was the limited supply of qualified CPIPs to include in the study and, consequently, the authors suggest that further upskilling of community pharmacists to IP status may benefit overall development of the sector.
“The publication from Nottingham has shown clearly that with the right training and support, the community pharmacist was rapidly embraced by the primary healthcare team with the majority maintaining employment once the project was completed,” says Jacqui Kinsey, director of prescribing education at Keele University and committee member of the Association for Prescribers.
We should be developing prescribing roles for those in the community pharmacy
However, she adds that this did necessitate the pharmacist leaving their community pharmacy role. “We should be developing prescribing roles for those in the community pharmacy,” she says.
Some community pharmacists have managed to forge roles as prescribers, but not without difficulties. Paul Blake, a community pharmacist working in a community centre on Walney Island in Barrow-in-Furness in Cumbria, says that there are many challenges to becoming an IP, particularly for community pharmacists.

Source: Courtesy, Paul Blake
Paul Blake, a community pharmacist working in a community centre on Walney Island in Barrow-in-Furness, Cumbria, says that he would like to see more of a peer-support network for community PIPs
“Finding a GP mentor, funding for the course, getting your employer to agree for you to have the time to do the course, then you need to get the funding to prescribe – there are a number of barriers,” he says.
Blake became a PIP as part of a local scheme that has been running since September 2016, with the aim of taking pressure off GPs and improving patient access to medicines for problems beyond the scope of the minor ailments scheme. As the only PIP in the area, Blake prescribes for a number of acute conditions, including uncomplicated urinary tract infections, tonsillitis, impetigo, otitis media and externa, and eczema.
However, he says that being based in community pharmacy brings a number of challenges in terms of carrying on business as usual.
“It requires determination and time management,” he says.
“You’ve got medicines use reviews, the new medicine service, prescriptions, smoking cessation, etc. Then on top of that people will turn up and ask me to clinically assess and prescribe.”
Although Blake has access to patient records through the Healthcare Gateway Shared Record Viewer, an independent web portal that provides healthcare professionals with instant access to the Medical Interoperability Gateway (MIG), it all takes up time.
“While I’m doing that people might be waiting for prescriptions – you need to have a good team and the pharmacy needs to be running well in order to take on a role like this,” he says.
Blake adds he would like to see more of a peer support network for community PIPs. “Sharing a learning experience would be a good thing for the service to develop further,” he says.
Kinsey says that community pharmacists find they have limited scope to use their prescriber qualification.
Government and political factors have not yet fully grasped what the community pharmacist can offer to the multidisciplinary healthcare team
“Government and political factors have not yet fully grasped what the community pharmacist can offer to the multidisciplinary healthcare team,” she says.
“Pharmacists in other settings may find fewer barriers to becoming a prescriber. Like nurses, pharmacists working in a hospital setting are already seen as a valued member of the healthcare team,” she says. “They have a recognised role in supporting junior doctors to make safe prescribing decisions and are recognised as the expert in medicines.”
It is therefore an easier road to become a prescriber because some of the barriers have already been broken down, says Kinsey.
Rhian Deslandes, a lecturer at the school of pharmacy and pharmaceutical sciences at Cardiff University, who researches pharmacist independent prescribing, agrees.

Source: Courtesy, Rhian Deslandes
Rhian Deslandes, a lecturer at the school of pharmacy and pharmaceutical sciences at Cardiff University, says that there are a number of challenges for community pharmacists wanting to becomes PIPs, including access to medical records
“The role [of community pharmacists] is evolving and that might change further with the contract over the years but there are other challenges, in terms of access to medical records and allowing them the time and management to do that role.”
She adds that for pharmacists working in GP practices, many of those barriers are dealt with. “Patient records are there, booking and consultation systems are all in place.”
Although not a pharmacist himself, Marc Krishek’s work as education and training lead at North East London Local Pharmaceutical Committee has made him aware of the barriers affecting community pharmacists wanting to carry out a greater clinical role. One of these, he says, is not having full access to the patient record.
Pharmacies do not have the complete care record, which is important if you’re prescribing under an NHS contract
“Pharmacies have got the summary care record but not the complete care record, or read-and-write access to those records, which is important if you’re prescribing under an NHS contract — you want to see patient details and medication history,” he explains.
Krishek’s local pharmaceutical committee believes that community pharmacists should be able to do whatever GP practice pharmacists can do. The trouble, he says, is that they do not have access to the same support network and community pharmacists are not being thought of in the same way when it comes to national funding.
“In hospital, pharmacists have senior clinicians they can turn to for advice and support for their decisions; in a GP surgery you’ve got GPs to refer to.” He believes that a clearer vision is needed for the role of community pharmacists.
Source: Courtesy, Marc Krishek
Marc Krishek, education and training lead at North East London Local Pharmaceutical Committee, says that if pharmacists are to take on IP roles the whole pharmacy team needs to be upskilled in order to continue to support patients
However, being a PIP in hospital is not without its barriers, as Michalla Nathanson, a nutrition, women and children’s pharmacist at Homerton Hospital has found out. She finally persuaded her manager to allow her to undertake the course in January 2017, but has not yet used her qualification.
“I am still not prescribing because, despite every effort, my job description has not been changed to include IP,” she explains.
According to Nathanson, she is one of only four pharmacists to undertake the course at Homerton, and none of these pharmacists currently prescribe.
“There has been active encouragement by clinicians within the trust to have IP pharmacists,” she says.
“The reluctance to instigate this is down to pharmacy department management — clinicians here do not understand why the IP pharmacists aren’t prescribing or why more pharmacists are not undertaking the course.”
The support and infrastructure is simply not there, she adds.
As Krishek points out, it is not just about individual prescribers, the whole pharmacy team needs to be on board.
If pharmacists are taking on IP roles they also need to upskill the whole pharmacy team
“If pharmacists are taking on IP roles, they also need to upskill the whole pharmacy team,” he says.
“If your pharmacist is going to provide a greater clinical service and support behaviour change, they need a team of staff behind them who can support the patient.”
In GP practices
While independent prescribing in community pharmacies is just getting off the ground, just a short walk along the high street PIPs are already a valued part of the primary healthcare team in general practice.
Rachel Hall qualified initially as a supplementary prescriber but became an independent prescriber as soon as she could. Now she is the diabetes lead and partner in a GP practice in Bristol and says she uses her qualification “all day, most days”.

Source: Courtesy, Rachel Hall
Rachel Hall says she was initially apprehensive about becoming a PIP but over the years she has built up her expertise and now GPs come to her for advice about how to manage patients
“I was a bit apprehensive about it at first — I thought it was a big area to choose and a steep learning curve. Looking back now I’m really glad [I became an IP],” says Hall.
“All the GPs come to me for advice about how to manage patients. I’ve built up that expertise over the years, being well supported by primary care colleagues such as diabetic specialist nurses, and diabetologists at the local hospital. It’s been a great role.”
Although at first, Hall says, she needed to build trust among the practice partners and there was some reluctance from the nurses to accept her role because they were concerned she was going to take more interesting work away from them.
She emphasises that, as a PIP, support from doctors and other healthcare professionals is essential.
There are times when you need advice from a GP to manage a patient safely
“Some of these patients are really complex — their condition may not be to do with their medication — there are times when you need advice from a GP to manage that patient safely. And that’s what it’s all about — trying to deliver safe, effective care and not working in isolation,” she says.
Magnus Hird, who works in general practice in Blackpool, also had a lot of support from his medical colleagues when he decided to become a PIP and his qualification has allowed him to develop his role over the years.
“It’s a better experience for patients, there’s no more hanging around — it’s more streamlined. I don’t have to interrupt someone in the middle of their surgery to sign a piece of paper,” he explains.
Hird adds that he can see how community pharmacy could easily manage people with long-term illnesses who are relatively stable.
“But we just don’t commission that as a service yet in the health system — so we need to look at that model commissioning-wise, because the healthcare system is stretched to capacity and we’re not using some of the capacity that is out there,” he adds.
Prescriber-ready graduates
Professional healthcare organisations as well as individuals such as the chief pharmaceutical officers should all be acting as advocates to make it possible for all pharmacists to be able to prescribe early in their careers, if not at the point of registration, says Kinsey.
“I do believe that the pharmacist’s knowledge in pharmacology and therapeutics learned through their undergraduate degree ideally places them among the other healthcare professions to take on prescribing roles,” she says.
“This knowledge should be recognised along with further support and opportunities to encourage community pharmacists to gain the prescribing qualification, so that their role becomes more integrated into existing healthcare systems,” she adds.
Hird believes that all pharmacists should be prescriber ready when they graduate, as a minimum. It is important to instil some of the competencies that being a prescriber needs early on, he says.
I think [prescribing] is something we should be aiming for as a normal skill for pharmacists to have
“I think it’s something we should be aiming for as a normal skill for pharmacists to have,” he says.
Hall says that the pharmacy degree needs to become much more clinically focused with built-in work placements to enable pharmacists to build their experience, more in line with the way that doctors train.
“I don’t think pharmacists should be IPs from the moment they qualify because you need to have some work experience in the real world before you do that,” she says.
HIV specialist Richardson also has concerns about pharmacists being full IPs immediately after graduating, but she agrees that the role needs to be normalised to move it forward.

Source: Courtesy, Claire Richardson
“If everyone came out with a prescribing qualification then it would just be so normal for pharmacists to be prescribers, like doctors,” says Claire Richardson, lead pharmacist in HIV and sexual health
“Part of your responsibility when prescribing is that you are competent in that area … I don’t think you should be able to prescribe straight away,” she says.
“But then again, maybe it’s just a complete change in mindset — if everyone came out with a prescribing qualification then it would just be so normal for pharmacists to be prescribers, like doctors.”
As the role of pharmacists continues to grow it is clear that independent prescribing will form a key part of that evolution and, while individuals such as Richardson, Hird and Hall are reaping the benefits of their advanced roles, it is important to address the barriers that are preventing other pharmacists from progressing too.
While the outcome of the GPhC’s consultation may help to address some barriers, it is clear that there are others, such as lack of access to patient records, the availability of peer-support networks and a lack of support from pharmacy management, which must be overcome to ensure all pharmacists can reach their desired potential.
- This article was amended on 2 March 2018 so that the number of independent prescribers includes those pharmacists who are registered as both supplementary and independent prescribers, rather than those only registered as independent prescribers, as stated previously.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
References
[1] General Pharmaceutical Society. Prescribers survey report. May 2016. Available at: https://www.pharmacyregulation.org/sites/default/files/gphc_prescribers_survey_report.pdf (accessed February 2018)
[2] Department of Health. The NHS Plan: a plan for investment, a plan for reform. July 2000. Available at: http://webarchive.nationalarchives.gov.uk/20121102184216/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4002960 (accessed February 2018)
[3] NHS Scotland. Achieving excellence in pharmaceutical care: a strategy for Scotland. August 2017. Available at: http://www.gov.scot/Resource/0052/00523589.pdf (accessed February 2018)
[4] NHS Wales and Welsh Government. Non-medical prescribing in Wales. May 2017. Available at: http://www.awmsg.org/docs/awmsg/medman/Non%20Medical%20Prescribing%20in%20Wales%20Guidance.pdf (accessed February 2018)