
Illustration by Emily Nash
Amid the chatter of customers and tinkling of cutlery in a restaurant in London’s West End, head chef Alex Farrey watches over his kitchen staff as they plate up dishes. His job is one of exact measures and narrow time windows, made harder by the fact he has type 1 diabetes, and must control his glucose levels as precisely as he controls his kitchen.
The disorder means that his body does not produce insulin — the hormone that helps to control blood glucose levels. High levels of blood glucose can cause problems in the vascular system, eyes, kidneys, feet and nerves. If blood glucose is too low, it can make people feel weak; they may begin to tremble; and if left unchecked, it can lead to loss of consciousness, organ failure and death.
“It’s a pain having to take glucose readings and inject myself with insulin, and having to measure and record everything that I eat,” Farrey says. Like the roughly 400,000 people in the UK with type 1 diabetes, Farrey has to frequently measure the level of glucose in his blood and inject himself with insulin every time it gets too high – and he must do this as many as six times a day. “I’m used to it now but when I was a kid it was tough, especially missing out on things my friends were doing because their parents didn’t feel comfortable helping me with my blood readings or injections.”
“What we call ‘diabetes burnout’ is a big problem in type 1 diabetes,” says Kotryna Temcinaite, a research communications officer at charity Diabetes UK. “People have to manage their condition every day and can never take a holiday from measuring their blood glucose.”
What we call ‘diabetes burnout’ is a big problem in type 1 diabetes. People have to manage their condition every day and can never take a holiday from measuring their blood glucose
While insulin has helped people like Farrey to manage their disease, researchers are working on ways they can make it better. “Insulin is not a very good drug — it’s actually very bad,” says Danny Chou, a diabetes researcher at the University of Utah in Salt Lake City, Utah. “With other drugs, if a doctor gives you one pill, that’s good; two pills, that’s good; three pills it’s OK, not worse. With insulin, if you don’t have enough it’s bad and if you have too much it’s worse. It can push you into hypoglycaemia and kill you.”

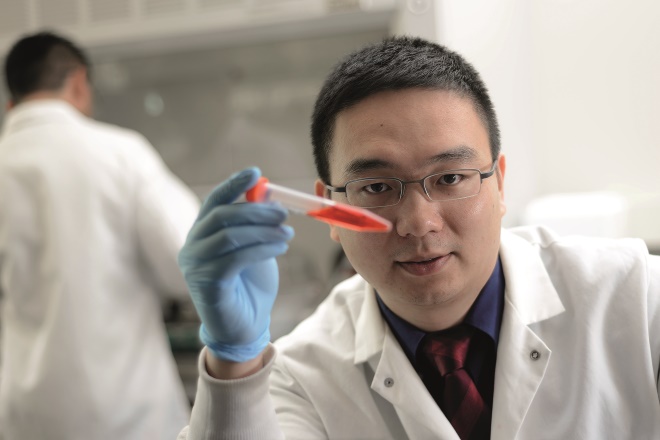
Source: Courtesy of Danny Chou
Danny Chou, a diabetes researcher at the University of Utah in Salt Lake City, is working on a strategy to modify insulin so it binds to serum albumin and detaches when blood glucose is high
Scientists like Chou want to make an insulin that would need to be injected only, say, once a day and would become active only in the presence of high glucose concentrations. In this way, so-called glucose-responsive or smart insulins would mimic the action of the insulin-producing beta cells in the pancreas of a healthy individual.
“For most people with type 1 diabetes, a glucose-responsive insulin really approaches what they consider would be a miracle treatment for the disease,” says Julia Greenstein, vice president of research at JDRF, a US-based international public charity that funds research and advocacy efforts including Chou’s, into type 1 diabetes. “The idea of not having to constantly count carbs and figure out the dose of insulin to give yourself would make a huge difference.”
For most people with type 1 diabetes, a glucose-responsive insulin really approaches what they consider would be a miracle treatment for the disease
The prospects of a smart insulin making a difference to patients’ lives is one firmly for the future — most research projects are at the basic chemistry level, with researchers trying to show a proof of principle that such a treatment is possible. Thereafter, they will have to prove that their treatment is safe and that the large loads of injected insulin will be active only when needed and not cause hypoglycaemia. Justifying the potentially high prices to payers might also be a sticking point given other technologies that might soon be available to people with type 1 diabetes.
A false start
In terms of promise, 2010 was an exciting year for type 1 diabetes. There was news that SmartCells — a US start-up that had developed a candidate smart insulin drug — had been snapped up by drug giant Merck & Co for US$500m to take it into clinical testing. The technology was developed by SmartCells co-founder and chief executive officer Todd Zion, a former researcher at the Massachusetts Institute of Technology (MIT) in Cambridge, Massachusetts, with funding from JDRF. It used nanoscale molecular engineering to make insulin bio-available only when a sugar-sensitive protein called lectin sensed the presence of glucose.
After the acquisition, Merck entered the candidate drug, which it called MK-2640, into a phase 1 clinical trial that finished at the end of 2016[1]
. In email correspondence, the company confirmed that due to a lack of efficacy in that trial it had terminated the development of MK-2640. Merck says that it is moving forward with a back-up candidate but it is too early to give additional details. Zion was also unavailable for comment.

Source: Shutterstock.com
Development of Merck’s candidate smart insulin MK-2640 has been terminated because of a lack of efficacy in phase I trials, but the company is moving forward with a back-up candidate
Merck’s is not the only project in the pipeline. Though details are not publicly available, JDRF’s Greenstein is aware that other drug giants are interested in developing smart insulin and the charity remains committed to the concept. In May 2014, it put out a request for applications for research projects to be co-funded with French pharmaceutical company Sanofi.
In February 2016, JDRF and Sanofi announced US$4.6m to support four basic research projects with different strategies to develop glucose-responsive insulin. Esther Latres, JDRF’s director of translational development, says that smart insulin projects fall into two broad categories. “You can modify the insulin so that it auto-activates in response to glucose or you can combine insulin with a polymer that releases it on detection of glucose,” she says. “At this point, we are spreading our funding across a portfolio to determine the best strategy and type of smart insulin for further development and testing in human clinical studies.”
Modifying insulin
Chou and colleagues’ project is one of the four funded by JDRF and Sanofi. Chou’s strategy is to modify insulin so it binds to serum albumin, a protein abundant in human blood plasma, and detaches and becomes bioactive only in the presence of high blood-glucose concentrations. It is a simple idea that will be difficult to execute, he explains, because insulin is a tricky molecule to modify.
“There are three potential sites you can modify on insulin, and you can pretty much only modify one site and not the other two if you want to preserve the bioactivity of the molecule,” he says. “We want to add a hydrophobic lipid onto the insulin molecule so it can bind to the serum albumin, but to control that binding interaction in a glucose-sensitive way we need a glucose sensor.”
There are three potential sites you can modify on insulin, and you can pretty much only modify one site and not the other two if you want to preserve the bioactivity of the molecule
To sense the concentration of glucose in the blood the team is using phenylboronic acid, a synthetic molecule that recognises and binds sugar molecules such as glucose and fructose. Specificity of a sensor to glucose — and not fructose — is important because if another sugar type triggers insulin release at low blood-glucose concentrations it would cause potentially lethal hypoglycaemia. “Glucose is the most abundant type of sugar in the blood, so because of this dominance we think we can get a pretty good specificity,” says Chou.
Much of Chou’s work has used chemical methods to tweak the insulin molecule. In 2015, he showed that a synthetic insulin molecule could rapidly respond to and reverse high blood-glucose concentrations in diabetic mouse models over 13 hours — the best performing of their insulin derivatives did so better than native insulin[2]
. It was the first time that a modified insulin molecule was shown to respond to glucose in vivo.
The team has since improved its insulin-modification technique, using enzymatic rather than chemical approaches. Chou says an enzymatic approach is more precise and has described the technique in a paper still under review for publication. The team is refining and testing different glucose-responsive insulin analogues in biological systems for efficacy with one eye on specificity to glucose. “That phenylboronic acid is not that specific to glucose may or may not be a problem,” says Chou. “We’ll be looking at that to modify and tweak it to make it better.”
Delivering unmodified insulin
Zhen Gu is a biomedical engineer at the joint department of biomedical engineering at the University of North Carolina at Chapel Hill and North Carolina State University and used to be a post-doctoral researcher, along with Chou, at MIT. His research is another of the projects funded by JDRF and Sanofi, and it aims to design a polymer that encapsulates unmodified insulin and releases it in the presence of high blood-sugar levels.
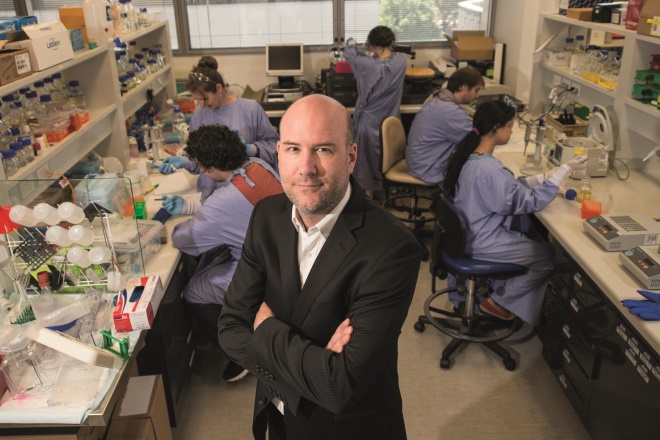
Source: Courtesy of Zhen Gu
Zhen Gu, biomedical engineer at the joint department of biomedical engineering at the University of North Carolina at Chapel Hill and North Carolina State University, is developing a nanoparticle formulation that responds to a hypoxic local environment by disintegrating and releasing its unmodified insulin cargo
He is developing a nanoparticle formulation that responds to a hypoxic local environment by disintegrating and releasing its insulin cargo. To create a hypoxic environment only when glucose concentrations are high, he is using an enzyme called glucose oxidase, which converts glucose to gluconic acid, and in doing so reduces the concentration of local oxygen.
As well as the speed at which insulin is released, the ease with which the smart insulin is administered is a focus of Gu’s laboratory. The team has developed a microneedle array patch, a stamp-sized patch with eyelash-thick microneedles that delivers the glucose-responsive vesicles loaded with insulin and glucose oxidase intradermally. In 2015, Gu and colleagues showed that their patch could effectively regulate blood glucose in mice with chemically induced type 1 diabetes[3]
. They are testing and refining their technology in larger animals (currently in minipigs).
Another JDRF-Sanofi grant recipient is Christoph Hagemeyer, who heads up the nanobiotechnology laboratory at Monash University in Melbourne, Australia. His goal is to make a compound that can deliver insulin as soon as the body needs it to be able to respond rapidly to the sugar spikes that occur after a meal. In this way, he sees smart insulin not only being able to ease the logistical burden on patients, but also to help improve the accuracy of glucose control.
Source: Ger / Hynesite Photography
Christoph Hagemeyer, head of the nanobiotechnology laboratory at Monash University in Melbourne, Australia, is aiming to make a compound that can deliver insulin as soon as the body needs it to be able to respond rapidly to the sugar spikes that occur after a meal
He offers an analogy to describe the clumsiness of current insulin use, with doses calculated and injected on the basis of blood-glucose readings. “Imagine you’re going down the highway in a car and you can only do full throttle acceleration or full-on braking — you are also blindfolded and can only see the road every five minutes,” he says. “That’s how diabetics manage their disease — it’s never in real time. The aim of our project is to be not necessarily where the beta cells are but we want to be close to the action so we can increase the speed of response to rising glucose levels.”
Imagine you’re going down the highway in a car and you can only do full throttle acceleration or full-on braking — you are also blindfolded and can only see the road every five minutes; that’s how diabetics manage their disease
Like Chou, Hagemeyer is using a borate system to sense glucose. He is remaining tight-lipped on the specifics of his compound until he receives patents, but says he will pick from three potential nanomaterials for his insulin-carrying scaffold. “It might be that we make something just to help with the after-dinner glucose spikes first, because slow-release insulin formations can help people cope with the rest of the day,” he says. For route of administration, he suggests that it might first be an injection but that, ideally, he would like it to be oral. However, variances in digestion and absorption rates will complicate the accuracy of dosing. “We’re about three to five years away from testing in larger animal models so we’re not getting ahead of ourselves. Our focus now is on getting the basics right.”
Back to basics
Given the potential dangers involved in overdosing with insulin, safety is fundamental. That means showing a proof of principle that not only is the concept possible but that a glucose-responsive insulin treatment can respond selectively to glucose and at only the desired concentrations.
Source: Courtesy of John Fossey
Researchers in John Fossey’s laboratory at the University of Birmingham are trying to identify the best synthetic glucose-responsive polymers and vesicles to deliver insulin
In John Fossey’s laboratory at the University of Birmingham, two post-doctoral researchers surrounded by basic chemistry equipment describe how nascent their research project is. “It’s literally gooey jelly and crystals and stuff in flasks being stirred and mixed right now,” says Jonathan Kedge, one of the researchers. They are trying to identify the best synthetic glucose-responsive polymers and vesicles to deliver insulin.
One of their tasks is to work out how to incorporate specific glucose sensors into big chemical structures that can entrap insulin. They are working with bis-boronic acids, which have two boronic acid moieties and, if spaced correctly, can theoretically bind to glucose over other sugars present in the blood, such as fructose. Earlier this year, Fossey and colleagues published details of four such novel bis-boronic acids[4]
.

Source: Courtesy of Jonathan Kedge
Jonathan Kedge, one of the researchers in John Fossey’s laboratory, University of Birmingham, is trying to work out how to incorporate specific glucose sensors into big chemical structures that can entrap insulin
“We’d then maybe have a hydrogel mesh that would entrap the insulin and, with a bis-boronic acid trigger, would fall apart in the presence of glucose and release the insulin,” says Lukasz Banach, another researcher in the laboratory. In unpublished work, they have shown a proof of principle that this hydrogen mesh, when combined with a mono-boronic acid, can release a previously loaded fluorescent dye. The next step is to develop a molecular construct that releases insulin in a dose-responsive way to the surrounding glucose concentration. The Fossey Lab receives funding from the UK’s Engineering and Physical Sciences Research Council, the Wellcome Trust and JDRF.
The bigger picture
Including the four projects it funds with Sanofi, says JDRF’s Latres, the organisation’s smart insulin grant portfolio stretches to 14. Most fall into either modified or encapsulated insulin strategies, but some use mathematical modelling to better define the physiological parameters under which glucose-responsive insulins can work and will make these models freely available to all researchers.
“All these projects have risks,” says Latres, referring to either the risk of hypoglycaemia or the immunogenicity of the compounds, “so we need to spread our funding across many projects.” She adds that these products need to be “incredibly specific and incredibly safe”. “If people are going to give themselves a day’s worth of insulin, or maybe even a week’s eventually, there can’t be any leakage.”
If people are going to give themselves a day’s worth of insulin, or maybe even a week’s eventually, there can’t be any leakage
There is another reason for JDRF to spread its bets among different strategies. “In a perfect world, there will be one molecule that can control highs and lows [of blood glucose],” says Greenstein, “but it’s possible that the first compound to succeed might just control peaks and another might just prevent hypoglycaemia, so an effective treatment might take a mix of different strategies.” On the cost of smart insulin as a barrier to treatment, Greenstein says “we don’t know what it is yet so have no idea about whether it will be expensive. If it’s a simple modification to insulin it could be competitive, but if it’s more complex the acceptability of the price will come down to what payers will think about it in relation to other treatment options.”
On the cost of smart insulin, we have no idea yet if it will be expensive. If it’s a simple modification to insulin, it could be competitively priced
Diabetes UK’s Temcinaite sees future smart insulins as competing with other technologies in development that can remove the burden of glucose monitoring and insulin injections from patients, such as artificial pancreases or beta cell replacement therapy. Artificial pancreases are medical devices that monitor blood glucose and administer insulin as necessary. In September 2016, the US Food and Drug Administration approved the first such system for use, Medtronic’s MiniMed 670G System. No systems have yet been approved elsewhere. Beta cell replacement therapy is a concept being researched in which beta cells might be given to a patient and shielded from the effects of the immune response that destroys native beta cells in people with type 1 diabetes.

Source: Courtesy of Kotryna Temcinaite
Kotryna Temcinaite, a research communications officer at charity Diabetes UK, warns that smart insulins are in the early stages of development so it is too early to be able to promise anything to patients
“In the end, it will be down to a patient’s personal preference,” says Temcinaite. “If they want to inject themselves once a day or have something implanted under their skin, all these technologies are potentially life-changing.” Though excited by smart insulins, Temcinaite is cautious about being overly optimistic to people with type 1 diabetes. “It’s far too early to be able to promise anything just yet. Smart insulins are still in the early stages of development and we want to avoid giving them false hope,” she says.
“I get that this is all going to take a while,” says Farrey. “And I get that a load of the projects might not even make it, but even the idea of this kind of smart insulin and getting rid of all the headache of living with diabetes would be incredible. It would be pretty much a cure. I’m excited for the possibility, for myself but mostly for kids who won’t have to go through all the problems I had to go through.”
References
[1] Merck Sharp & Dohme. A three-part study to evaluate the safety, pharmacokinetics and pharmacodynamics of MK-2640 in healthy participants (part I) and participants with type 1 diabetes mellitus (parts II and III) (MK-2640-001). ClinicalTrials.gov identifier: NCT02269735. Available at https://clinicaltrials.gov/ct2/show/NCT02269735 (accessed November 2017).
[2] Chou DH, Webber MJ, Tang BC et al. Glucose-responsive insulin activity by covalent modification with aliphatic phenylboronic acid conjugates. Proc Natl Sci USA 2015;112:2401–2406. doi: 10.1073/pnas.1424684112
[3] Yu J, Zhang Y, Ye Y et al. Microneedle-array patches loaded with hypoxia-sensitive vesicles provide fast glucose-responsive insulin delivery. Proc Natl Sci USA 2015;112:8260–8265. doi: 10.1073/pnas.1505405112
[4] Zhai W, Male L & Fossey JS. Glucose selective bis-boronic acid click-fluor. Chem Comms 2017;53:2218–2221. doi: 10.1039/C6CC08534B


