
istockphoto.com
Forget laughter. And maybe even drugs. Exercise is the best medicine, or so many doctors say.
No other medical intervention can influence overall well-being as positively as physical activity. Countless epidemiological and clinical studies have demonstrated this, and now public health agencies around the globe — including the World Health Organization (WHO), the UK Chief Medical Officer and the US Department of Health and Human Services — are recommending that adults do at least 150 minutes of moderate aerobic activity (that which maintains an increased heart rate) or 75 minutes of vigorous physical activity each week, or some combination thereof. An hour or more of daily exercise is suggested for children and adolescents.
Source: University of Tennessee at Chattanooga University Relations
Gregory Heath, an exercise scientist at the University of Tennessee at Chattanooga, says evidence for the benefits of exercise is overwhelming
These best-practice guidelines have been informed by a number of systematic reviews showing that a minimum threshold of aerobic activity leads to diverse benefits, including lowering the risks of heart problems, metabolic disorders, cancer, depression and other chronic diseases. Physical inactivity is estimated to be responsible for around 9% of premature deaths; eliminating this sedentariness could theoretically increase the life expectancy of the world’s population by around eight months[1]
.
“The evidence is overwhelming,” says Gregory Heath, an exercise scientist at the University of Tennessee at Chattanooga. Exercise is “one of the least appreciated, underused therapeutic tools available to the human race”.
Exercise is one of the least appreciated, underused therapeutic tools available to the human race
Generally speaking, the more you exercise, the more health benefits you get. But researchers around the world are trying to determine whether there is an optimal dose of aerobic exercise. For example, is it possible to overdo it? And is it important to do something that gets the heart racing or can a gentle stroll be as beneficial?
Scientists also want to determine how those benefits come about: what effects physical activity has on organs and tissues at the cellular and molecular level. This may help guide exercise recommendations for people at different stages of life, as well as in developing targeted regimens for people with particular health problems.
Run for your life
Two studies published in the June 2015 issue of the journal JAMA Internal Medicine begin to provide answers to some of these questions. One study considered close to a decade of mortality data from more than 200,000 Australian adults. It found that engaging in at least some vigorous exercise, such as jogging or cycling, provided more of a reduction in mortality than only doing moderate activity, for instance walking or gardening[2]
. The study authors, led by Klaus Gebel from James Cook University in Cairns, Australia, and Adrian Bauman from the University of Sydney, reckoned that two minutes of moderate activity may not equal one minute of vigorous activity, as far as health benefits go. They concluded that healthcare professionals should put greater emphasis on encouraging high-intensity exercise.

Source: National Cancer Institute
Hannah Arem, an epidemiologist who investigates physical activity at the US National Cancer Institute, says exercise guidelines are ”pretty spot on”
In the other study, a team led by Hannah Arem, an epidemiologist who investigates physical activity at the US National Cancer Institute in Bethesda, Maryland, pooled data from six large cohort studies including a total of more than 660,000 adults. Each person was tracked for 14 years on average. By looking at the mortality records, Arem and her colleagues showed that people who did some aerobic exercise, but did not get up to the recommended minimum level, reduced their risk of premature death by 20% compared with people who did not exercise at all. People who met the guidelines fared even better, with a 31% lower risk of death compared with those who never lifted a toe[3]
.
The health benefits from increasing exercise levels peaked at about three times the recommendations, equivalent to a little more than an hour on average each day. But for people who embrace fitness to that extent “the additional benefit is pretty marginal”, notes Arem. These optimal exercisers were only 8% less likely to die than people who merely met the minimum recommendations. At greater levels of activity, the reduction in mortality risk tapered off: exercise fiends with activity levels ten times the recommended dose did not accrue additional protection against premature death — but, notably, they were not at undue risk either. The Australian study similarly found no significant danger of extreme activity levels.
Given the challenges of getting people to exercise at all, Arem feels that her findings support and validate today’s consensus for suggested amounts of physical activity. “The guidelines are pretty spot on,” she says.
Most exercise recommendations concentrate on the overall time spent engaging in activity, rather than when or how often you get active. But this tends to overlook the flipside of exercise — sedentariness. Some studies support the idea that it does not really matter whether people exercise in many short spurts or in longer workouts less often, if it adds up to their recommended time allotment. But a January 2015 meta-analysis of 47 articles showed that sitting for long periods is linked with deleterious health outcomes regardless of the extent of other physical activities[4]
. “Exercise is great, but if you sit for too long those risks [of sedentariness] might predominate,” says study author Avi Biswas from the University of Toronto, Ontario.
Exercise is great, but if you sit for too long those risks of sedentariness might predominate
Acting on evidence like this, an international group of experts, convened at the behest of Public Health England and a British community interest company, published a white paper in June 2015 calling on people to avoid staying seated during the workday. The guidelines recommend breaking up the day with two to four hours of standing or short activity breaks[5]
.
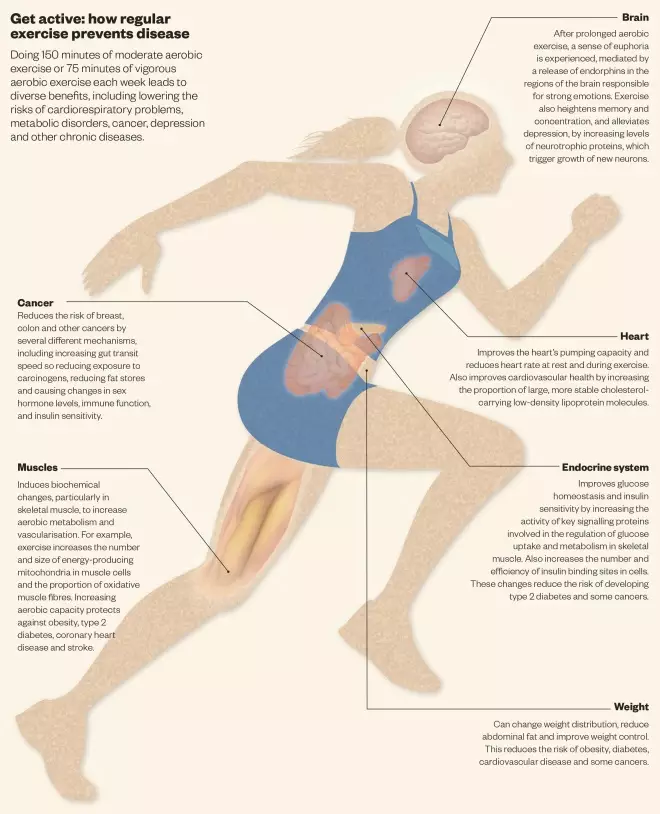
Get active: how regular exercise prevents disease
Source: British Journal of Pharmacology and Scientific American
Doing 150 minutes of moderate aerobic exercise or 75 minutes of vigorous aerobic exercise each week leads to diverse benefits, including lowering the risks of cardiorespiratory problems, metabolic disorders, cancer, depression and other chronic diseases
Walk the walk
Weight loss is the most obvious advantage of physical activity. But aerobic exercise leads to many other long-term physiological changes, too. It helps reduce blood pressure, improves the body’s ability to use insulin and favourably tips the balance of cholesterol profiles. Muscles and bones grow stronger, and the capacity of blood vessels to distribute oxygen is improved.
And regular activity may be as good for the brain as it is for the body. The benefits for mind and mood are many, but include improved cognitive performance as a result of increased blood flow, and the growth of new neurons and synapses caused by the production of growth factors, such as brain-derived neurotrophic factor (BDNF). Not to mention the release of endorphins, hormones and other chemicals responsible for ‘runner’s high’ — the feeling of euphoria brought on by intensive exercise.
Some of these effects emanate from the brain, but others originate in the muscles. For example, in 2014, researchers at the Karolinska Institute in Sweden showed that in mice exercise triggers skeletal muscles to produce an enzyme that helps metabolise a stress chemical called kynurenine. The enzyme breaks kynurenine down into a metabolite that cannot cross the blood–brain barrier, protecting the brain from stress-induced changes associated with depression[6]
. In humans, the researchers also saw increased expression of this enzyme in muscles after frequent endurance training.
Despite studies like this, for the most part the cellular and molecular mechanisms by which physical activity alters organs and tissues remain poorly understood. So, in June 2015, the US National Institutes of Health (NIH) launched a US$170m, five-year programme to catalogue and characterise the ‘exercise responsome’ — all the biological molecules affected by physical activity in some way.
In addition to mapping the molecular changes that occur after people exercise, “at the end of the project NIH will deliver to the scientific community a database that researchers from around the world can access to develop and test their own ideas about how these molecules contribute to health”, says Joan McGowan, director of the Division of Musculoskeletal Diseases at the NIH’s National Institute of Arthritis and Musculoskeletal and Skin Diseases. “All of this information will be linked to the general background of the people who contributed it — their age, race and ethnicity, sex, and whether they were exercising regularly at the beginning of the study.”
“Science operates on the principle that the more you know the better informed your recommendations could be,” says Darrell Neufer, director of the East Carolina Diabetes and Obesity Institute in Greenville, North Carolina. Neufer was consulted by the NIH and is the lead author of a recent article describing the outcomes of a 2014 workshop that helped shape the new funding scheme[7]
. “The ultimate hope is that we can use this information to either better design exercise prescriptions or to identify new ways that cells function that could be targeted with other approaches, including pharmaceuticals.”
Of course, many of the same benefits of aerobic training can be achieved with drugs. Statins similarly reduce levels of low-density lipoprotein ‘bad’ cholesterol and modestly increase high-density lipoprotein concentrations. Beta-blockers, like regular physical activity, will slow the heart rate and lower blood pressure. Anticoagulants and exercise both cut the risk of developing a stroke. Antidepressants also regulate levels of key neurotransmitters.
Drugs and exercise are rarely tested head-to-head for effectiveness. But Huseyin Naci, a health policy researcher at the London School of Economics, and John Ioannidis, director of the Stanford Prevention Research Center in California, have compared mortality rates across 305 randomised controlled trials looking at either exercise or drug interventions for chronic conditions such as heart disease, diabetes and stroke. They found that the two approaches led to similar reductions in mortality[8]
.

Source: Charles Guerra
Pedro Hallal, a physical activity epidemiologist at the Federal University of Pelotas, Brazil, says that exercise does not carry the side effects common with many medicines
However, tipping the balance in exercise’s favour, many experts point out that physical activity offers all the protection of multiple drug classes in one simple intervention. “You would need to have 12 or 13 different drugs to mimic all the effects of exercise,” says Pedro Hallal, a physical activity epidemiologist at the Federal University of Pelotas in Brazil. Plus, exercise does not carry the kinds of side effects that are common with many medications. And physical activity is good for mental well-being and other health indicators not necessarily linked to death.
You would need to have 12 or 13 different drugs to mimic all the effects of exercise
Naci says he is now comparing exercise and drugs for non-mortality outcomes. One problem, he says, is that the evidence base for exercise pales in comparison to the amount of data available about the efficacy of many top-selling pills for controlling chronic disease. Naci and Ionnidis’s recent review included around 340,000 study participants; only about 1 in 20 received an exercise intervention. “That’s a huge asymmetry in the existing research enterprise,” says Naci.
There is an obvious explanation for this asymmetry. Most drug trials are sponsored by pharmaceutical companies hoping to sell a product. Exercise does not have the same potential for profit, so it receives less scrutiny in controlled trials. Nonetheless, a growing number of doctors are calling for exercise to be treated more like a drug, prescribed to patients who need it.
Prescription for success
Through an initiative called ‘Exercise is medicine’, primary care physicians and other healthcare providers are routinely beginning to track levels of physical activity at every clinic visit and to ‘prescribe’ customised exercise regimens. The project was launched in 2007 by the American Medical Association, based in Chicago, Illinois, and the American College of Sports Medicine (ACSM), based in Indianapolis, Indiana, and now has a presence in more than 43 countries worldwide.
There is evidence that this approach can be helpful. For example, a team led by Richard Grant, a research scientist at Kaiser Permanente in Oakland, California, recently piloted a programme to collect exercise information systematically, along with traditional health metrics, and add it to patients’ electronic medical records. They found that this spurred doctors to discuss exercise options more with patients, which led to a small but significant reduction in weight among those who were overweight, as well as improved control of blood sugar among individuals with diabetes[9]
. According to Grant, this programme, dubbed ‘Exercise as a vital sign’, “is now standard of care at all practices within Kaiser Permanente” across the state of California.
In the UK, for more than a decade the NHS has offered exercise referral schemes in which patients, after assessment by their family doctors, can receive discounted or free access to gym sessions, yoga classes or other forms of physical activity. And in Canada, medical societies in some provinces are now handing out specially designed prescription pads that include checkboxes for doctors to note patients’ exercise patterns, with additional space to indicate the frequency and duration of physical activity.
Ultimately, getting people to meet exercise recommendations will require buy-in from all parties involved in healthcare and well-being — doctors, patients, medical providers, community organisations and more. “The real difficulty and challenges are going to be the same as taking any drug. It’s adherence,” says Adrian Hutber, a physiologist who leads the ‘Exercise is medicine’ programme at the ACSM. “If you can get the adherence, you’ll really start getting change.”
- Correction: on 21 July at 6pm (BST), the graphic ‘Get active: how regular exercise prevents disease’ was updated to correct the statement that exercise reduces the risk of breast, colon and other cancers by increasing “gut transit speed” and not, as it originally read, “gut transit time”.
References
[1] Lee IM, Shiroma EJ, Lobelo F et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. The Lancet 2012;380:219–229.
[2] Gebel K, Ding D, Chey T et al. Effect of moderate to vigorous physical activity on all-cause mortality in middle-aged and older Australians. JAMA Internal Medicine 2015;175:970–977.
[3] Arem H, Moore SC, Patel A et al. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Internal Medicine 2015;175:959–967.
[4] Biswas A, Oh PI, Faulkner GE et al. Sedentary time and its association with risk for disease incidence, mortality, and hospitalization in adults: a systematic review and meta-analysis. Annals of Internal Medicine 2015;162:123–132.
[5] Buckley JP, Hedge A, Yates T et al. The sedentary office: a growing case for change towards better health and productivity. Expert statement commissioned by Public Health England and the Active Working Community Interest Company. British Journal of Sports Medicine [In Press: Online] 2015. Available from: doi:10.1136/bjsports-2015-094618.
[6] Agudelo LZ, FemenÃa T, Orhan F, Porsmyr-Palmertz M, Goiny M, Martinez-Redondo V et al. Skeletal muscle PGC-1α1 modulates kynurenine metabolism and mediates resilience to stress-induced depression. Cell 2014;159:33–45.
[7] Neufer PD, Bamman MM, Muoio DM, Bouchard C, Cooper DM, Goodpaster BH et al. Understanding the cellular and molecular mechanisms of physical activity-induced health benefits. Cell Metabolism [In press: Online] 2015. Available from: doi:10.1016/j.cmet.2015.05.011.
[8] Naci H & Ioannidis JP. Comparative effectiveness of exercise and drug interventions on mortality outcomes: metaepidemiological study. BMJ 2013;347: f5577.
[9] Grant RW, Schmittdiel JA, Neugebauer RS et al. Exercise as a vital sign: a quasi-experimental analysis of a health system intervention to collect patient-reported exercise levels. Journal of General Internal Medicine 2014;29:341–348.


