View the full infographic here
Musculoskeletal conditions
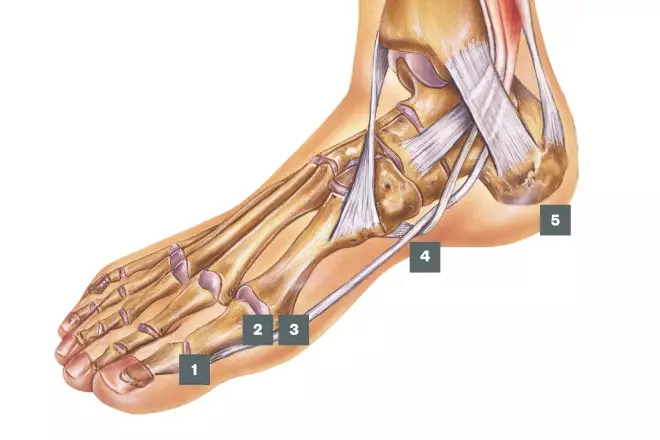
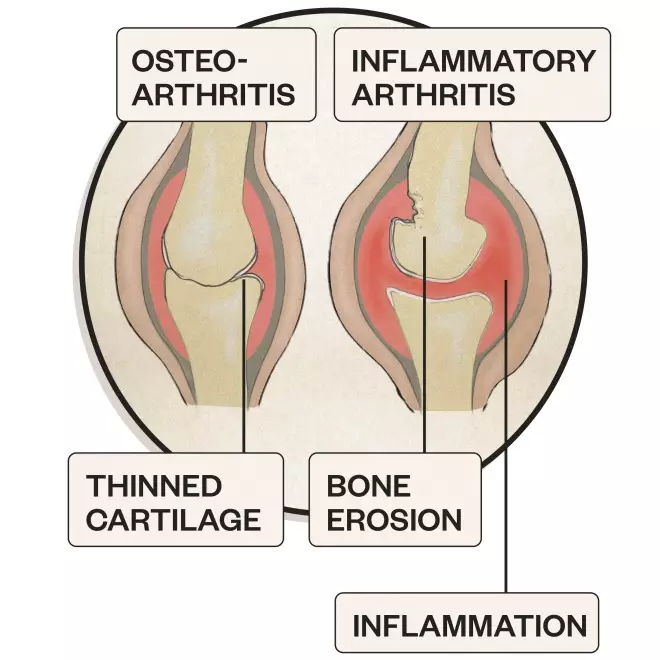
1. Arthritis
Symptoms of arthritis include pain and swelling in a joint or joints, stiffness and reduced range of movement and joint deformity
Causes: Osteoarthritis and inflammatory arthritis
Treatment: Refer to GP
The foot is involved in 80–90% of people with rheumatoid arthritis

2. Bunions
Bunions are bony deformities at the base of the big toe, which often cause it to point inwards
Causes: Family history, arthritis and poorly fitting shoes
Treatment: Offer bunion pads, insoles and painkillers if required. Refer to GP or podiatrist if pain interferes with walking. Surgery may be needed
23% of adults aged 18–65 years and 36% of elderly people aged over 65 years have bunions
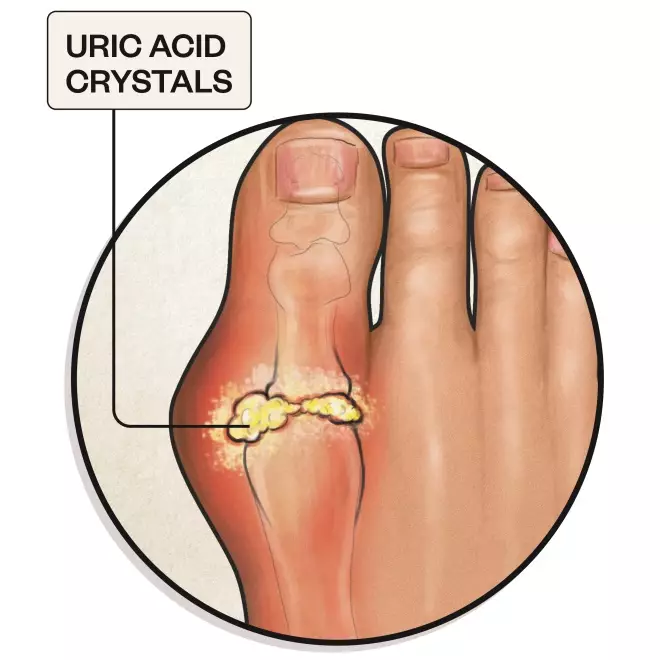
3. Gout
Gout causes severe pain, swelling and stiffness in one or more joints, accompanied by red, shiny skin
Causes: Build-up of uric acid in the blood
Treatment: Refer to GP for treatment of acute attack with non-steroidal anti-inflammatory drugs, colchicine or corticosteroids. Lifestyle changes and prophylactic treatment may be required
Gout affects 2.5% of UK adults and is more common with increasing age, affecting 15% of men and 6% of women over the age of 75 years
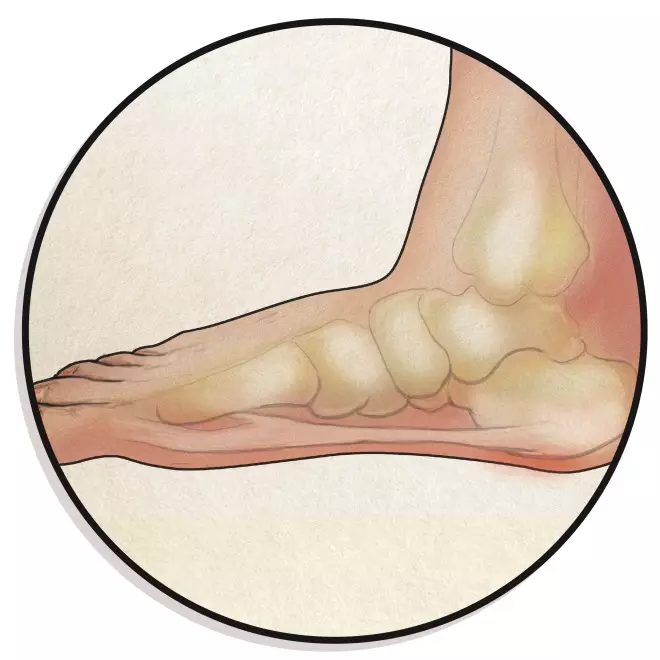
4. Flat feet
Flat feet occur when there are no or low arches, causing possible pain in the feet, ankles, lower legs, knees, hips, or lower back
Causes: Hereditary, arthritis or an injury
Treatment: If painful, refer to GP or podiatrist for stretches and insoles
Flat feet may occur in up to 20% of adults, but many of these have no resulting symptoms
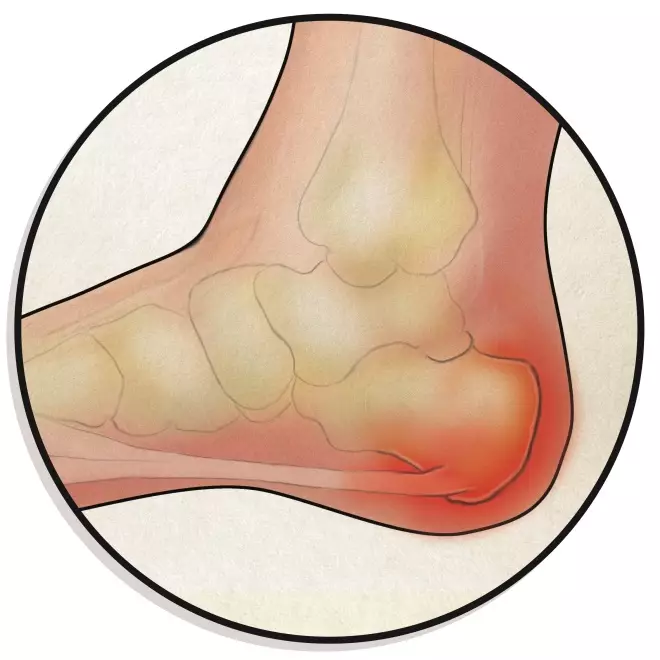
5. Plantar fasciitis
Plantar fasciitis causes heel pain when weight bearing that is worse in the morning but improves on walking
Causes: Inflammation of the plantar fascia caused by sudden or chronic damage
Treatment: Treatment includes rest, good footwear, heel pads, painkillers and exercises. Refer to GP or podiatrist if heel pain persists for several weeks. A steroid injection may be needed in severe cases
10% of people will develop plantar fasciitis at some time in their life
Skin, nail and soft tissue conditions

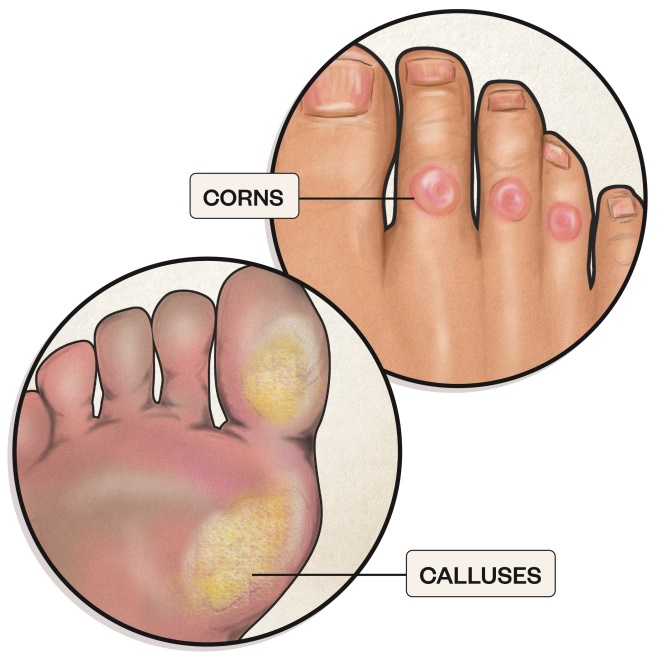
6. Corns and calluses
Corns are small circles of thick skin on the tops and sides of toes or on the soles of the feet and calluses are larger areas of rough, thickened, yellowish skin, often found on the balls of the feet
Causes: Excessive pressure or friction, often from poorly fitting shoes. Certain activities, for example, running
Treatment: Advise patient to remove pressure and apply rehydration cream, corn plasters, pads or salicylic acid products (but not for those with poor circulation or diabetes). If severe, refer to a podiatrist for skin removal
Corns affect between 13–48% of the population

7. Fungal nail infection
Infected nails are thickened, distorted, white, black, yellow or green and sometimes surrounded by inflamed, painful skin
Causes: Fungal infection that thrives in moist, warm conditions. Commonly follows a fungal skin infection
Treatment: Offer antifungal nail laquer or solution. Refer patients who do not respond to topical treatment to a podiatrist or GP
Fungal nail infections affect 3–8% of the UK population

8. Blisters
Blisters are small fluid-filled pockets that form within the upper layers of skin
Causes: Poorly-fitting shoes, heat, chemicals or diseases such as chickenpox
Treatment: Advise patient not to burst the blister. Cover with plaster or gauze if needed. Refer to GP if infected
Heal naturally after 3 to 7 days

9. Diabetic ulcer
A diabetic ulcer is a patch of broken down skin with visible underlying tissue
Causes: High or fluctuating blood sugar levels and poor circulation delay skin repair after minor injury. The peripheral neuropathy means the injury may go unnoticed
Treatment: Refer urgently to the local multidisciplinary diabetes team or GP — patient should be seen within 24 hours
10% of people with diabetes will develop a diabetic foot ulcer
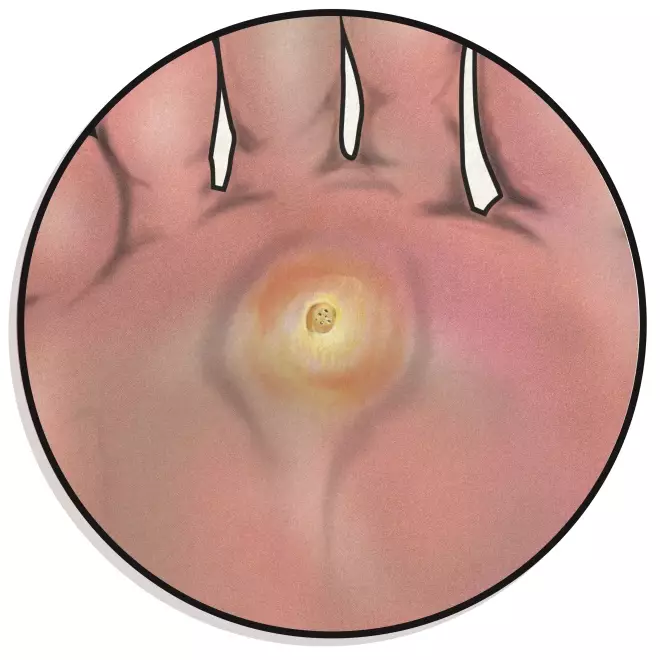
10. Verrucas
Verrucas are areas of flat, rough skin with a cluster of black dots in the centre; approximately 1–10mm diameter. They can appear in pairs or groups
Causes: Human papilloma virus (HPV), transmitted by skin-to-skin contact or via contaminated surfaces
Treatment: Salicylic acid products can speed up the healing process; refer to a podiatrist if treatment is unsuccessful
Half of verrucas in children disappear on their own in a year and two-thirds resolve within two years, but they can take many years to resolve in adults

11. Athlete’s foot
Athlete’s foot causes dry, red, scaly, flaky, itchy and painful skin between the toes, starting with the little toe
Causes: Fungal infection that thrives in moist, warm conditions
Treatment: Advise patient to keep toes clean and dry, and apply antifungal cream, spray or powder. Refer to GP if no improvement after one week of treatment. Likely to recur even after successful treatment
Athlete’s foot is present in about 15% of the UK population

12. Ingrown toenail
Toenails can grow into the skin at the side of the nailbed, causing redness, inflammation and sometimes infection
Causes: Poorly fitting shoes or socks, badly trimmed nails, nail trauma, moist skin
Treatment: Advise patient to keep their feet clean and cut nails straight across. Offer an antiseptic cream or spray, but refer to GP or podiatrist if severely inflamed, bleeding or producing pus. Surgery may be required in severe cases
10,000 estimated new cases of ingrown toenails present in the UK each year
RB provided financial support in the production of this content. The Pharmaceutical Journal retains full editorial control.
UK/SC/0617/0031d
References
Sources: NHS Choices, BMJ, Patient, National Institute for Health and Clinical Excellence, Journal of Foot and Ankle Research, British Journal of Podiatry and Arthritis Research UK.
Editorial adviser: Ivan Bristow, podiatrist and programme lead for BSc (Hons) Podiatry, Faculty of Health Sciences, University of Southampton.
Infographic: AlisdairMacdonald.co.uk