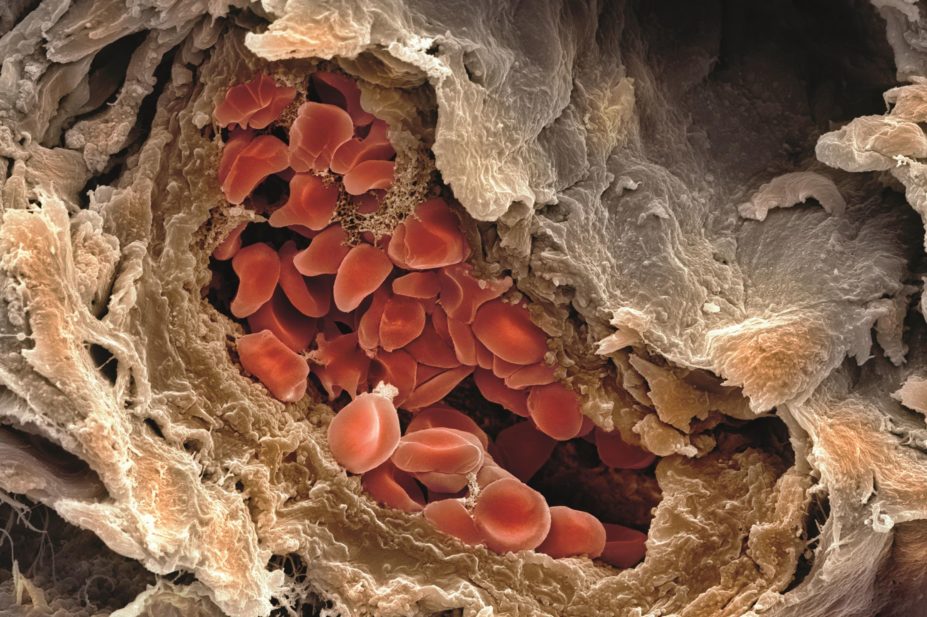
Steve Gschmeissner / Science Photo Library
Currently, approximately 1.3 million patients are prescribed anticoagulant therapy in the UK[1]
, the majority for atrial fibrillation (AF), venous thromboembolic disease (VTE) and mechanical heart valves[2]
. The most common oral anticoagulant is warfarin, but increasing numbers of patients are being treated with the direct oral anticoagulants (DOACs): apixaban, dabigatran, edoxaban and rivaroxaban. A small minority of patients are treated with alternative vitamin K antagonists (VKAs): acenocoumarol (Sinthrome) and phenindione.
Around 10–15% of anticoagulated patients undergo surgery or an invasive procedure each year[3]
,[4]
. Formal bridging anticoagulation involves the substitution of oral anticoagulation with a short-acting alternative, usually low molecular weight heparin (LMWH), during the perioperative period[3]
,[5]
.
Traditionally, patients on warfarin either had their dose adjusted to maintain a lower international normalized ratio (INR), or were converted to intravenous heparin infusion during the perioperative period[6]
. This necessitated protracted hospital admissions while warfarin was restarted and restabilised. Managing heparin infusions is notoriously difficult, requires frequent monitoring using blood tests, and many patients are under or over-anticoagulated. In the past ten years or so, LMWH has increasingly been used for management of these patients: subcutaneous injections of LMWH can be administered by the patient, facilitating earlier discharge from hospital in patients who are otherwise fit to go home.
The emergence of more evidence about the need for bridging anticoagulation therapy and the introduction of DOACs have led to changes in how patients are managed, which is the focus of this article.
Risk stratification
The decision about whether to continue or interrupt anticoagulation depends on the patient’s bleeding and thrombotic risks. Previously published guidelines[3]
,[6]
,[7]
have been based on expert consensus, however a meta-analysis[8]
concluded that bridging increases the risk of post-operative bleeding without reducing the risk of thrombotic events. The evidence base is evolving with the recently published BRIDGE study[4]
and ongoing PERIOP 2 trial (clinicaltrials.gov, identifier: NCT00432796).
Can anticoagulation be continued for the procedure?
This is the first question to ask. If anticoagulation causes significant blood loss, or bleeding into a critical site (e.g. neurosurgery, spinal or ophthalmic surgery), it could ultimately result in a longer period of time without anticoagulation. If the bleeding risk is low, then the usual anticoagulant can be continued (see ‘Table 1: Common procedures in which oral anticoagulant therapy may be continued’).
Specialist guidelines[9]
,[10]
,[11]
,[12]
,[13]
,[14]
largely refer to warfarin, and there is no published trial data relating to DOACs. Where they have been published, consensus/expert guidelines recommend that if a procedure can be performed on warfarin with an INR in the therapeutic range, then it may also be performed on any anticoagulant[9]
,[15]
. If the anticoagulant is a VKA, a pragmatic approach is to check the INR a week prior to the procedure to allow for any necessary dose adjustments to be made, with a further INR check on the day before, or day of, the procedure[14]
.
There are some procedures, such as spinal/neurosurgery and radical prostatectomy, where the bleeding risk is very high and full bridging or even prophylactic LMWH may be considered to be too high risk: in the author’s institution these are considered on a case by case basis.
| Table 1: Common procedures in which oral anticoagulant therapy may be continued | |
|---|---|
| Dental procedures | |
| Low risk of post-operative bleeding complications
|
| Opthalmology | |
| |
| Cardiology | |
| Gastroenterology | |
| |
Sources: British Dental Journal | |
What is the thrombotic risk?
If anticoagulation cannot be safely continued, the thrombotic risk determines how the anticoagulation is managed (i.e. whether or not bridging is required).
Atrial fibrillation
The BRIDGE study is the first to have examined whether bridging is required in patients with AF by comparing bridging with a placebo[4]
. It demonstrated that in patients with a CHADS2 score of 4 or less, bridging provided no benefit in terms of stroke, myocardial infarction, VTE or death, and resulted in increased rates of both major and minor bleeding[3]
,[5]
. Previous practice has been to risk stratify (see ‘Table 2: Thrombotic risk stratification for mechanical heart valves and VTE’), but these new results will result in a major change in practice. Patients with a CHADS2 score of 5–6 were under-represented in the BRIDGE study and high risk procedures, such as cardiac surgery, carotid endardectomy, major cancer surgery and neurosurgery, were excluded[4]
. Clinicians may therefore continue to use bridging for these patients with AF.
Mechanical heart valves
Patients with mechanical heart valves are at risk of valve thrombosis and stroke, and warfarin or other VKAs are used for anticoagulation. The daily thrombosis risk of a non-anticoagulated heart valve is approximately 0.01%[17]
, although the risk is greater with older more thrombogenic valves and mitral valves rather than aortic valves[17]
.
Venous thromboembolism
Many patients who have had an idiopathic VTE (i.e. a VTE with no provoking event such as surgery, immobility or illness) continue on long-term anticoagulation to prevent recurrence. Without anticoagulation, the incidence of recurrence is approximately 20% in five years, with a 2.6% incidence of fatal pulmonary embolism[18]
. ‘Table 2: Thrombotic risk stratification for mechanical heart valves and VTE’ describes the thrombotic risk stratification for patients with mechanical heart valves and VTE.
| Table 2: Thrombotic risk stratification for mechanical heart valves, atrial fibrillation (AF) and venous thromboembolism (VTE) | |||
|---|---|---|---|
| Thrombotic risk if not anticoagulated (% per year) | Mechanical heart valve[3] ,[5] | AF[4] | VTE[3] ,[5] |
| Low risk (<5%) | Bileaflet aortic valve with no additional risk factors | CHADS2 0–4 | VTE over 3 months ago†|
| Moderate (5–10%) | Bileaflet aortic valve prosthesis and one or more of the following risk factors: AF, prior stroke or transient ishaemic attack (TIA), hypertension, diabetes, congestive heart failure, age >75 years | VTE within the past 3–12 months†, non-severe thrombophilia (e.g. heterozygous factor V Leiden or prothrombin gene mutation), recurrent VTE, active cancer (treated within 6 months or palliative) | |
| High (>10%) | Any mitral valve prosthesis, any caged-ball or tilting disc aortic valve prosthesis, recent (within 6 months) stroke or TIA | CHADS2 5–6 | VTE within previous 3 months, severe thrombophilia (e.g. deficiency of protein C, protein S, or antithrombin; antiphospholipid antibodies; multiple abnormalities) |
CHADS2: congestive heart failure, hypertension, age 75 years or over, diabetes mellitus, and stroke or TIA (two points); †British Committee for Standards in Haematology (BCSH) consider VTE > 3 months ago to be low risk. American College of Clinical Pharmacy (ACCP) consider VTE > 12 months ago to be low risk, and 3–12 months ago to be moderate risk. | |||
Anticoagulant bridging
Depending on the outcome of the thrombotic risk assessment, the following action may be needed:
- Low thrombotic risk, or AF with CHADS2 score 0–4: no bridging required: use prophylactic LMWH only;
- Moderate thrombotic risk: consider bridging (weigh up bleeding risks)[3]
– some hospitals use bridging for all moderate risk, some work on a case-by-case basis; - High thrombotic risk: bridging required.
Even if formal bridging is not required, many surgical procedures will still require the use of prophylactic anticoagulation for the prevention of VTE (e.g. low dose LMWH)[19]
. The highest risk procedures are major cancer surgery in the abdomen or pelvis (e.g. surgery for bowel, liver, stomach or prostate cancer), hip fracture repair, hip replacement and knee replacement[19]
: the National Institute for Health and Care Excellence (NICE) recommends that all patients, regardless of previous anticoagulation exposure, should receive extended post-operative VTE prophylaxis (i.e. low dose anticoagulant for up to 35 days post-operatively)[19]
. In patients who are usually anticoagulated, the prophylactic anticoagulation should continue post-operatively until their usual treatment has resumed and they are fully anticoagulated. This isn’t true bridging, but may be referred to as such.
Bridging for warfarin
‘Table 3: Low molecular weight heparin (LMWH) doses’ outlines suggested LMWH doses, and ‘Table 4: Suggested pre- and post-operative management of LMWH for bridging’ outlines the pre- and post-operative management of LMWH for bridging and warfarin.
| Table 3: Low molecular weight heparin (LMWH) doses | |||
|---|---|---|---|
*May be split twice daily, to the nearest whole syringe | |||
| LMWH | Prophylactic dose | Intermediate dose (greater than prophylactic, but less than therapeutic) | Full therapeutic dose |
| Dalteparin | 5,000 units once daily | 5,000 units twice daily | 200 units/kg/day* |
| Enoxaparin | 40mg once daily | 40mg twice daily | 1.0mg/kg twice daily or 1.5mg/kg once daily |
| Tinzaparin | 4,500 units once daily | 4,500 units twice daily | 175 units/kg |
| Table 4: Suggested pre- and post-operative management of LMWH for bridging (as used in the author’s institution) | ||
|---|---|---|
| Day -5 | Last dose of warfarin[3] ,[4] | |
| Day -4 | No warfarin | |
| Day -3 | ||
| Day -2 | INR check: If INR <2.0, start full dose LMWH | No warfarin If INR >2.5 give vitamin K†|
| Day -1 | LMWH in morning only (half dose e.g. dalteparin 100 units/kg)* | No warfarin |
| Day 0 (surgery) | Prophylactic LMWH at least six hours post-op | |
| Day 1 | Prophylactic LMWH | Warfarin restarted at the patient’s usual dose on day 1 |
| Day 2 | Prophylactic LMWH | |
| Day 3 | Intermedicate or full dose LMWH | |
| Day 4 | Intermedicate or full dose LMWH | |
| Day 5 onwards | Full dose LMWH: stop when INR >2.0 | |
†Phytomenadione 1mg orally; *At least 24 hours pre-operatively, to allow safe use of spinal/epidural analgesia[20] | ||
Post-operatively, full dose anticoagulation with LMWH should not be started until at least 48 hours after a high bleeding risk procedure or 24 hours after a minor procedure with low bleeding risk[3]
. Prophylactic LMWH only should be given until then. As further safeguards against bleeding, some centres use an intermediate dose of LMWH on days +3 and +4 post-operatively, and/or spit full dose LMWH into two daily doses[3]
. Whatever regime is used, it is imperative LMWH is not started, or the dose increased, until the clinicians are satisfied that there is no concern about bleeding. The assessment will include examining the wound site, the amount of fluid collecting in surgical drains, the expected bleeding, and monitoring of the patient’s haemoglobin levels. In some circumstances (e.g. where it is likely that a patient may return to the operating theatre) it may be appropriate to continue prophylactic LMWH for longer than the usual regime.
If the patient has epidural analgesia in situ, LMWH should not be increased above prophylactic doses because of the risk of spinal haematoma causing neurological dysfunction[20]
. If treatment doses are given, then the epidural catheter must not be removed for at least 24 hours after the last dose: however this is not usually recommended[20]
.
In patients with severe renal impairment (i.e. a calculated creatinine clearance less than 30ml/min), LMWH is usually not appropriate[21]
,[22]
. In these circumstances it may be necessary to use an infusion of unfractionated heparin instead[3]
. This provides full treatment dose anticoagulation and should be stopped 4–5 hours pre-operatively and restarted at least 24–48 hours post-operatively depending on the bleeding risk of the procedure. In the meantime, prophylactic LMWH may be used (some units use adjusted doses for renal impairment).
Warfarin is commonly restarted at the patient’s usual dose, usually on the day after surgery[3]
. It may be appropriate to give a double dose on the first day[3]
, but loading doses should be avoided as they introduce the risk of over-anticoagulating the patient in a short time post-op. By continuing the patient’s usual dose, the INR only needs to be checked every 3–4 days, facilitating early discharge from hospital as soon as the patient is otherwise fit to leave. When the INR reaches 2.0, LMWH can be stopped (even if the target INR range is higher): this will usually be within 5–10 days of restarting warfarin.
Warfarin in patients at low thrombotic risk
These patients can have a prophylactic dose of LMWH both pre- and post-operatively until the patient has restarted warfarin and their INR has reached over 2.0. AF patients with a CHADS2 score of 0-4 may stop LMWH when they are discharged from hospital, provided the procedure they underwent does not require extended thromboprophylaxis[19]
.
Direct oral anticoagulants
The direct oral anticoagulants have an almost immediate onset of action (peak levels are achieved within 2–4 hours of a dose), and they do not usually require any routine monitoring apart from periodic renal and liver function tests[23]
,[24]
,[25]
,[26]
,[27]
. This potentially makes the perioperative management more straightforward if anticoagulation needs to be stopped. The last dose of DOAC should be timed to achieve normal coagulation status by the time of surgery[15]
(see ‘Table 5: Timing of last pre-operative doses of direct oral anticoagulants’). The timing depends on the patient’s renal function, as all the DOACs are cleared renally to some extent (dabigatran significantly more so than the factor Xa inhibitors)[23]
,[24]
,[25]
,[26]
. It is important to note that the DOACs are not licensed with renal function below those listed in ‘Table 5: Timing of last pre-operative doses of direct oral anticoagulants’: if the patient has acute kidney injury or chronic renal impairment with a creatinine clearance (CrCl) less than the lower cut off, then it may be necessary to delay surgery for a longer period of time until coagulation tests suggest that clotting has normalised[28]
.
| Table 5: Timing of last pre-operative doses of direct oral anticoagulants (DOACs)[15] | |||
|---|---|---|---|
| Class | Drug | Time of last dose pre-operatively | |
| High bleeding risk | Low bleeding risk | ||
| Factor Xa inhibitors | Apixaban | CrCl >50 CrCl 15–49 | CrCl >50 CrCl 15–49 |
| Edoxaban | CrCl >30 CrCl 15–29 | CrCl >30 CrCl 15–29 | |
| Rivaroxaban | CrCl > 30 CrCl 15–30 | CrCl >30 CrCl 15–30 | |
| Direct thrombin inhibitor | Dabigatran | CrCl >80 CrCl 50–79 CrCl 30–49 | CrCl >80 CrCl 50–79 CrCl 30–49 |
Post-operatively, the usual DOAC should not be re-started until there are no concerns about bleeding: in practice this will be 24–48 hours post-op depending on the procedure. Prophylactic dose LMWH should be given in the meantime[24]
,[25]
,[26]
. LMWH and DOAC should not overlap: they should be switched directly by giving the DOAC when the next dose of LMWH would have been due[23]
,[24]
,[25]
,[26]
. If the patient remains nil by mouth for an extended period, the LMWH doses can be escalated in the same manner as for patients on warfarin, and then switched to DOAC when the patient is able to take medicines orally.
Emergency surgery
There is not always enough time to manage a patient’s anticoagulation pre-operatively if a patient needs emergency surgery.
For patients on warfarin, 5mg of vitamin K given intravenously will significantly reduce the INR within 6–8 hours[29]
(giving a bigger dose will not speed up the effect, and oral administration acts more slowly). If surgery cannot be delayed that long, prothrombin complex concentrate (PCC) should also be given for a more rapid reversal[5]
(see ‘Box 1: Prothrombin complex concentrate’).
Post-operatively, patients may be managed in the same way as elective patients, bearing in mind that it may take longer for the INR to return to therapeutic range because of the effect of having had a large dose of vitamin K immediately pre-op.
Box 1: Prothrombin complex concentrate
- Beriplex and Octaplex[5]
- Vitamin K dependent clotting factors II, VII, IX and X and also Protein C and Protein S (vitamin K dependent anticoagulants)
- Dose range 25 units/kg to 50 units/kg depending on INR[30]
.- Some units use a standard dose of 30 units/kg regardless of INR to simplify and avoid delays[31]
.
- Some units use a standard dose of 30 units/kg regardless of INR to simplify and avoid delays[31]
- Coagulation is normalised <30 minutes
- Duration of effect is limited by half life of coagulation factors
- Shortest is factor VII: approx 6 hours
- IV vitamin K must also be given to maintain effect
- Prothrombotic — only suitable for emergency use
At the time of writing, dabigatran is the only DOAC to have a specific reversal agent: idarucizumab was licensed in December 2015[32]
. It is a humanised monoclonal antibody that selectively binds dabigatran 300 times more potently than dabigatran binds to thrombin. It has an almost immediate onset of action (less than ten minutes), and is licensed for reversal of dabigatran in emergency surgery and in life-threatening or uncontrolled bleeding[32]
. The manufacturers suggest that dabigatran can be restarted after 24 hours, but this should always be in conjunction with a clinical assessment of the patient, and post-operatively it would be prudent to wait at least 48 hours after major surgery[32]
.
There are currently no specific reversal agents for the factor Xa inhibitors, but andexanet has been trialled[33]
and is undergoing review by the Food and Drug Administration for licensing in the United States[34]
. Wherever possible, surgery should be delayed, waiting 1–2 half lives, to allow renal excretion of the drug. The use of PCC to reverse factor Xa inhibitors is based on healthy volunteer studies and case reports[35]
. The lack of a specific reversal agent for these drugs should not put patients off being anticoagulated with apixaban, edoxaban or rivaroxaban if they are considered to be the most suitable drug for them. Provided renal and liver function are monitored regularly and doses adjusted as appropriate[27]
, the bleeding risks are similar to or lower than that of warfarin[23]
,[24]
,[25]
,[26]
and the need for emergency surgery is comparatively uncommon.
Rebecca Hammond is an anticoagulation pharmacist at Sheffield Teaching Hospitals NHS Foundation Trust, Northern General Hospital, Herries Road, Sheffield, S5 7AU. Correspondence to:
Rebecca.Hammond@sth.nhs.uk
Financial and conflicts of interest disclosure: The author has received payments from Pfizer (2015) and Bayer (2013) for teaching sessions, run by a Royal Pharmaceutical Society local practice forum, on the subject of VTE management and anticoagulation in AF. Pfizer has also paid the registration fee for attendance at the European Association of Hospital Pharmacists Congress. No writing assistance was utilised in the production of this manuscript.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
References
[1] Support for commissioning: anticoagulation therapy: National Institute for Health and Care Excellence (NICE); 2013. Available at: https://www.nice.org.uk/news/press-and-media/advice-from-nice-supports-improved-commissioning-for-anticoagulation-therapy-for-adults (accessed April 2016).
[2] Baglin TP, Cousins D, Keeling DM et al. Safety indicators for inpatient and outpatient oral anticoagulant care: [corrected] Recommendations from the British Committee for Standards in Haematology and National Patient Safety Agency. British Journal of Haematology 2007;136:26–29. doi: 10.1111/j.1365-2141.2006.06379.x
[3] Douketis JD, Spyropoulos AC, Spencer FA et al. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141:e326S–350S.doi: 10.1378/chest.11-2298
[4] Douketis JD, Spyropoulos AC, Kaatz S et al. Perioperative Bridging Anticoagulation in Patients with Atrial Fibrillation. New England Journal of Medicine 2015;373:823–833. doi: 10.1056/NEJMoa1501035
[5] Keeling D, Baglin T, Tait C et al. Guidelines on oral anticoagulation with warfarin - fourth edition. British Journal of Haematology 2011;154:311–324. doi: 10.1111/j.1365-2141.2011.08753.x
[6] Guidelines on oral anticoagulation: third edition. British Journal of Haematology 1998;101:374–387.
[7] Douketis JD, Berger PB, Dunn AS et al. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008;133:299s–339s. doi: 10.1378/chest.08-0675
[8] Siegal D, Yudin J, Kaatz S et al. Periprocedural heparin bridging in patients receiving vitamin K antagonists: systematic review and meta-analysis of bleeding and thromboembolic rates. Circulation 2012;126:1630–1639. doi: 10.1161/circulationaha.112.105221
[9] Management of Dental Patients Taking Anticoagulants or Antiplatelet Drugs: Scottish Dental Clinical Effectiveness Programme; 2015.
[10] Perry DJ, Noakes TJ & Helliwell PS. Guidelines for the management of patients on oral anticoagulants requiring dental surgery. British Dental Journal 2007;203:389–393. doi: 10.1038/bdj.2007.892
[11] Cataract Surgery Guidelines: Royal College of Ophthalmologists; 2010 September 2010.
[12] Kiire CA, Mukherjee R, Ruparelia N et al. Managing antiplatelet and anticoagulant drugs in patients undergoing elective ophthalmic surgery. The British Journal of Ophthalmology 2014;98:1320–1324. doi: 10.1136/bjophthalmol-2014-304902
[13] Camm AJ, Lip GY, De Caterina R et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation–developed with the special contribution of the European Heart Rhythm Association. Europace 2012;14:1385–1413. doi: 10.1093/europace/eus305
[14] Veitch AM, Baglin TP, Gershlick AH et al. Guidelines for the management of anticoagulant and antiplatelet therapy in patients undergoing endoscopic procedures. Gut 2008;57:1322–1329. doi: 10.1136/gut.2007.142497
[15] Burnett AE, Mahan CE, Vazquez SR et al. Guidance for the practical management of the direct oral anticoagulants (DOACs) in VTE treatment. Journal of Thrombosis and Thrombolysis 2016;41:206–232. doi: 10.1007/s11239-015-1310-7
[16] Birnie DH, Healey JS, Wells GA et al. Pacemaker or defibrillator surgery without interruption of anticoagulation. New England Journal of Medicine 2013;368:2084–2093. doi: 10.1056/NEJMoa1302946
[17] Cannegieter SC, Rosendaal FR & Briet E. Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses. Circulation 1994;89:635–641. doi: 10.1161/01.CIR.89.2.635
[18] Hansson PO, Sorbo J & Eriksson H. Recurrent venous thromboembolism after deep vein thrombosis: incidence and risk factors. Archives of Internal Medicine 2000;160:769–774. doi: 10.1001/archinte.160.6.769
[19] Venous thromboembolism: reducing the risk for patients in hospital NICE guidelines [CG92]: National Institute for Health and Care Excellence; 2010 (updated 2015).
[20] Regional anaesthesia and patients with abnormalities of coagulation: the Association of Anaesthetists of Great Britain & Ireland The Obstetric Anaesthetists’ Association Regional Anaesthesia UK. Anaesthesia 2013;68:966–972. doi: 10.1111/anae.12359
[21] Fragmin 18,000 IU/0.72ml solution for injection summary of product characteristics: Pfizer Limited; [updated 16/10/2013; 03/04/2016]. Available from: http://www.medicines.org.uk/emc/medicine/26892 (accessed April 2016).
[22] Clexane Forte Syringes summary of product characteristics: Sanofi; [updated 24/09/2015; 03/04/2016]. Available from: http://www.medicines.org.uk/emc/medicine/10054 (accessed April 2016).
[23] Xarelto 20mg film-coated tablets summary of product characteristics: Bayer plc; 2015 [updated 17/07/2015; 01/02/2016]. Available from: http://www.medicines.org.uk/emc/medicine/25586 (accessed April 2016).
[24] Eliquis 5mg film-coated tablets summary of product characteristics: Bristol-Myers Squibb-Pfize; [updated 22/01/2016; cited 2016 01/02/2016]. Available from: http://www.medicines.org.uk/emc/medicine/27220 (accepted April 2016).
[25] Limited DSU. Lixiana 60mg Film-Coated Tablets summary of product characteristics 2016 [updated 25/01/2016; cited 2016 01/02/2016]. Available from: http://www.medicines.org.uk/emc/medicine/30506 (accepted April 2016).
[26] Pradaxa 150 mg hard capsules summary of product characteristics: Boehringer Ingelheim Limited; 2016 [updated 20/01/2016; 01/02/2016]. Available from: http://www.medicines.org.uk/emc/medicine/24839 (accepted April 2016).
[27] Suggestions for Drug Monitoring in Adults in Primary Care: London and South East Medicine Information Service, South West Medicine Information Service and Croydon Clinical Commissioning Group; 2014.
[28] Steiner T, Bohm M, Dichgans M et al. Recommendations for the emergency management of complications associated with the new direct oral anticoagulants (DOACs), apixaban, dabigatran and rivaroxaban. Clinical Research in Cardiology 2013;102:399–412. doi: 10.1007/s00392-013-0560-7
[29] Watson HG, Baglin T, Laidlaw SL et al. A comparison of the efficacy and rate of response to oral and intravenous Vitamin K in reversal of over-anticoagulation with warfarin. British Journal of Haematology 2001;115:145-9. doi: 10.1046/j.1365-2141.2001.03070.x
[30] Beriplex P/N 1000 IU summary of product characteristics: CSL Behring UK Limited; [updated 21/01/2014; 01/02/2016]. Available from: http://www.medicines.org.uk/emc/medicine/27570 (accessed April 2016).
[31] Toth P, van Veen JJ, Robinson K et al. Real world usage of PCC to “rapidly” correct warfarin induced coagulopathy. Blood transfusion 2013;11:500–505. doi: 10.2450/2012.0113-12
[32] Praxbind 2.5 g/50 mL solution for injection/infusion summary of product characteristics: Boehringer Ingelheim Limited; [updated 01/12/2015; 01/02/2016]. Available from: http://www.medicines.org.uk/emc/medicine/31243 (accessed April 2016).
[33] Siegal DM, Curnutte JT, Connolly SJ et al. Andexanet Alfa for the Reversal of Factor Xa Inhibitor Activity. New England Journal of Medicine 2015;373:2413–2424. doi: 10.1056/NEJMoa1510991
[34] Portola Pharmaceuticals Announces Biologics License Application for Andexanet Alfa Accepted for Review by FDA [press release]. 17/02/2016 2016.
[35] Dzik WH. Reversal of oral factor Xa inhibitors by prothrombin complex concentrates: a re-appraisal. Journal of Thrombosis and Haemostasis 2015;13:S187–194. doi: 10.1111/jth.12949


