
Shutterstock.com
The guidance and advice on COVID-19 contained within this article was correct at the time of publication. Guidance has now been updated and there are currently no restrictions in place in the UK. For more information, see: https://www.gov.uk/coronavirus
Clinical presentation of COVID-19 is that of a respiratory infection and symptoms range in severity from fever, fatigue and persistent cough, to pneumonia – a serious infection of the lungs that occurs owing to inflammation and fluid-filled alveoli[1],[2],[3]
.
Although the rate of pneumonia among patients with COVID-19 is not yet clear, it is widely understood that it leads to some of the most serious consequences[4]
.
Recognising pneumonia and suspected COVID-19
It is necessary to distinguish between symptoms that suggest viral infection and those that suggest bacterial or viral pneumonia. However, the overlap in symptom presentation can make it difficult to distinguish and differentiate COVID-19 from pneumonia.
Common symptoms of pneumonia can include:
- Cough;
- Difficulty breathing;
- Rapid heartbeat;
- Fever;
- Sweating and shivering;
- Loss of appetite;
- Chest pain
[3].
Less common symptoms include headache, fatigue, muscle or joint pain, and a general feeling of confusion.
Although a new, persistent cough and a high temperature are the most common symptoms of COVID-19, some patients also develop upper respiratory tract infection, loss of smell and taste, and symptoms such as headache or conjunctivitis [5]
,[6],[7],[8]
. This helps demonstrate the similarities in symptoms between COVID-19 and pneumonia.
As of 19 May 2020, testing for COVID-19 is carried out in the hospital setting to inform a patient’s clinical diagnosis, but also outside of the hospital setting for:
- All essential workers including NHS and social care workers with symptoms;
- Anyone aged over 65 years with symptoms;
- Anyone with symptoms who cannot work from home;
- Anyone who has symptoms of coronavirus and lives with any of those identified above
[9]
.
If COVID-19 is suspected, the patient should be advised to self-isolate and implement strict social distancing measures (see Box 1).
Box 1: Public Health England guidance on self-isolation
Guidance from Public Health England states that if a patient with possible COVID-19 lives with others, and is the first in the household to have symptoms, they must stay at home for 7 days; all other household members who remain well must stay at home and not leave the house for 14 days[10]
.
If anyone else in the household starts displaying symptoms, they need to stay home for 7 days from when their symptoms appeared, regardless of when they started the original 14-day isolation period.
Where possible, any vulnerable individuals (such as older people and those with underlying health conditions) should leave the house and stay with friends or family for the duration of the home isolation period. However, this is not always possible; in this case, patients should be advised to stay away from these individuals as much as possible[10]
.
Owing to the overlap of presenting symptoms between pneumonia and COVID-19, pharmacists should explain to the patient that they do not have two separate conditions; instead, having COVID-19 has likely led to their respiratory symptoms and pneumonia, or that they could have COVID-19 and community-acquired pneumonia.
Self-isolation with suspected infection
Patients with suspected COVID-19 should be told not to present in person to pharmacies or their GP[10],[11]
. However, it is possible that a patient, or their carer, can speak to the pharmacy team by phone or, in some cases, via video call (a practice adopted by some community pharmacies in response to the pandemic)[12]
.
Differentiating between viral and bacterial pneumonia
When a patient is being assessed, it is necessary for the prescriber to distinguish between viral and bacterial pneumonia; however, this is not straightforward and the need for a remote consultation makes this more difficult.
Eliciting a history of symptom presentation will help with differential diagnosis. For example, if a patient describes having a high temperature; a new, continuous cough; and an absence of any other symptoms, they should be referred to the NHS 111 online screening service, which will explain their next steps, and advise them to contact their GP if necessary[13]
.
On 3 April 2020, the National Institute for Health and Care Excellence (NICE) published a rapid guideline on managing suspected or confirmed pneumonia in adults in the community to ensure best practice treatment during the COVID-19 pandemic[14]
. These recommendations are subject to change as the knowledge base and expert experience develops. The main differences between bacterial and COVID-19-related pneumonia are summarised in the Table. As of 11 May 2020, no NICE rapid guidelines have been produced on managing children with pneumonia and COVID-19.
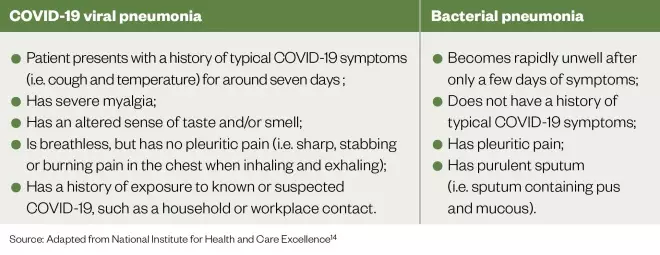
Source: Adapted from National Institute for Health and Care Excellence[14]
Assessing severity and referral
Normally, a patient would receive a physical examination as part of an objective assessment. However, NICE recommends that, during the COVID-19 pandemic, diagnosis of community-acquired pneumonia is informed by symptoms, such as:
- A temperature above 38°C;
- A respiratory rate above 20 breaths per minute;
- A heart rate above 100 beats per minute;
- New confusion[14]
.
It may not be possible or may be difficult to determine all these symptoms remotely, but it is important to determine whether the patient has shortness of breath. The Centre for Evidence-Based Medicine suggests asking the patient to describe the problem with their breathing in their own words, and assess the ease and comfort of their speech while they do so[15]
. This can be achieved by asking questions such as:
- “Are you so breathless that you are unable to speak more than a few words?”;
- “Are you breathing harder or faster than usual when doing nothing at all?”;
- “Are you so ill that you have stopped doing all of your usual daily activities?”[15]
.
It is important to understand whether there is a decline in the patient’s ability to breathe, as some, such as those with COPD, may already have existing conditions that affect their breathing. Asking “What could you do yesterday that you cannot do today?” or “What makes you breathless now that did not make you breathless last week?” may reveal the extent of the deterioration[15]
.
Although prior NICE guidance indicates that the CRB65 mortality prediction tool should be used to aid severity assessment of pneumonia and subsequent treatment, this has not been validated in people with COVID-19 and requires blood pressure measurement, which may be difficult or undesirable[14]
.
During the COVID-19 pandemic, NICE recommends that healthcare professionals are vigilant for red flag symptoms of pneumonia, which indicate that an urgent hospital referral is required:
- Severe shortness of breath at rest or difficulty breathing;
- Coughing up blood;
- Blue lips or face;
- Feeling cold and clammy with pale or mottled skin;
- Collapsing or fainting;
- Becoming difficult to rouse;
- Little or no urine output[14]
.
However, even if a patient does not have these red flags they may still require hospital care. Box 2 provides further considerations and criteria for hospital referral and admission[14],[16]
.
Box 2: Hospital referral and admission during the COVID-19 pandemic
It is important that pharmacists understand the reasons why a patient may or may not be admitted to hospital. This is important because concerned patients and family members or carers may be confused by the decisions made regarding their care. The decision to refer a patient to secondary care during the pandemic will depend on the following factors:
- The severity of symptoms and presence of any red flag symptoms;
- The benefits (e.g. availability of diagnostic tests, including X-rays) and disadvantages (e.g. the potential spread of COVID-19 and loss of contact with family) of admission;
- The care required (e.g. potential respiratory support);
- The patient’s wishes;
- Local NHS resources (e.g. hospital capacity)[14]
.
Older people, and those with comorbidities, frailty, impaired immunity or a reduced ability to cough and clear secretions, are more likely to develop severe pneumonia. As this can lead to respiratory failure and death, the National Institute for Health and Care Excellence recommends that the usual recommendations for these groups before the COVID‑19 pandemic are followed, and that hospital admission should be considered irrespective of COVID-19[14]
.
Hospital admission will also be required if the patient has severe pneumonia and requires oxygen, including if they are symptomatic with one of the following:
- Respiratory rate >30 breaths/minute;
- Severe respiratory distress;
- Peripheral capillary oxygen saturation of ≤93% on room air[16]
.
Patients and their carers should be advised that if they are struggling to breathe, or appear distressed on breathing while at rest, they should immediately call an ambulance. Paramedics will be able to accurately assess the patient and determine whether they should be admitted to hospital. If the patient is struggling to breathe, or symptoms worsen, but they are not in a severe state of distress, they should contact NHS 111 or their GP for further directions. This may still result in an ambulance being called.
Although it may be necessary and prudent to refer patients to hospital, if the decision is that the patient is not referred or admitted, then there is a need to manage them at home.
Even if the patient assessment indicates that they can be effectively managed in the community, it would be important to advise patients when they would need to seek additional advice (e.g. if symptoms worsen).
Managing pneumonia at home
The aim of managing symptoms of pneumonia at home is to reduce the impact of symptoms and aid recovery, while reducing admission and consequent pressure on hospital services.
Asking patients to record their symptoms in a diary will help both them and healthcare professionals understand the severity and how they will recover. In addition, assessing the patient’s breathing can help in determining whether their symptoms are worsening, remaining steady or improving. However, patients must understand the need to speak to a healthcare professional if their condition deteriorates or is not improving as expected.
In addition, patients should be advised that drinking plenty of fluids can help prevent dehydration from fever and that there is a need to get plenty of rest, which will aid the time course of recovery[17]
.
Breathlessness
An important initial step is to help manage a patient’s breathlessness. A patient who is breathless as a result of their chest infection may feel anxious at not being able to breathe normally; this can lead to further anxiety that, in turn, worsens breathlessness. Adopting techniques that reduce the sensation of breathlessness can have the combined effect of improving this symptom and helping the patient relax. Patients can be advised to:
- Adopt pursed-lip breathing (inhaling through the nose for several seconds then exhaling slowly through pursed lips for four to six seconds);
- Relaxing the shoulder and reducing the hunched posture;
- Sitting upright to increase peak ventilation and reduce airway obstruction;
- Leaning forward with arms bracing a chair can increase ventilatory capacity[18]
.
Antibiotics
In general, antibiotics should only be used when treating pneumonia with suspected bacterial infection, rather than that of viral origin. They should not be offered to patients when symptoms are mild or there is reason to suspect COVID-19 or viral pneumonia. When the pneumonia is suspected to be bacterial, or if the cause is unknown and the symptoms are concerning, then oral antibiotics will be necessary[14]
. Regardless of the cause, pharmacists will need to refer these patients to their GP or an NHS prescriber.
The first-line antibiotic is doxycycline 200mg, given immediately then 100mg once per day for a total of five days. Alternatively, the patient can be prescribed amoxicillin, given as 500mg three times per day for five days. If the patient is being managed at home and the medicine has been dispensed from a pharmacy, it should be emphasised that they should take the medicine as soon as possible, regardless of the time of day they collect/receive their medicine[14]
. For example, if a patient is prescribed amoxicillin and only receives their prescription in the evening then they should take their first dose immediately, followed by the normal dose at the specified intervals until their prescription runs out.
It is important to consider the following consultation points for these antibiotics:
- Doxycycline — patients who have been prescribed doxycycline should be warned to avoid exposure to direct sunlight during their treatment. Although many patients will not feel well enough to leave the house, some individuals may want to sit outside in the sun during their recovery and would be at a higher risk of sun damage as a result of the antibiotic. Doxycycline should also be taken with meals, as studies indicate that, although absorption of doxycycline is not notably influenced by simultaneous ingestion of food or milk, it can cause gastric disturbances which are minimised by the presence of food;
- Amoxicillin — ensure the patient has no known allergy to penicillin
[19],[20],[21]
.
It is important to note that patients who have viral pneumonia, potentially caused by COVID-19, may have a secondary bacterial infection. Although this is more common in those placed on ventilators, it can occur in patients being managed at home[22]
. This further highlights the need for patients to contact a healthcare professional if their symptoms worsen.
Recovery from pneumonia
Patients with pneumonia of either origin can have a significant recovery period. Although minor symptoms, such as elevated temperature, may disappear after a week, other symptoms can last much longer; for example, it could take:
- Four weeks for chest pain and mucous production to subside;
- Six weeks for a reduction in cough and breathlessness;
- Three to six months for fatigue to pass[23]
.
Although the specific timeframe for symptom recovery for COVID-19 is unknown, informing patients of the time periods for pneumonia recovery could be beneficial in helping them cope with their diagnosis and have realistic expectations about their ability to function after the infection resolves.
Patients can become anxious and depressed that they are still feeling fatigued several weeks after infection. Reassure them that slow recovery is normal, particularly after a severe pneumonia, owing to the systemic nature of the illness. Patients should be reminded to contact their GP if they are not seeing any improvement in their symptoms after a week or if they think their symptoms are getting worse.
As recovery can take several months, patients should be advised to rest at first and to not do more than they feel comfortable with. When they feel well enough to do more, they should be advised to do so gradually; for example, starting with moving around for a couple of minutes each day, increasing the duration of activity as their tolerance develops.
The British Lung Foundation also recommends “exercising the lungs” — taking long, slow breaths or blowing into water through a straw can help clear mucous from the lungs[23]
. More information on breathing techniques are available from the Association of Chartered Physiotherapists in Respiratory Care.
Best practice
It is essential to consider the following:
- How pneumonia is a serious consequence of COVID-19, but has different symptoms which allow for the conditions to be distinguished from each other;
- Timely referral to NHS 111 or a prescriber can ensure the most appropriate treatment for the patient;
- There is a need to answer a patient’s questions about their condition as they are likely to have concerns about symptoms and duration;
- Discussing breathlessness with the patient, and how to manage it, can help pharmacists track the patient’s condition and help them manage their symptoms effectively;
- Communication with the patient and GP may be difficult during this time, but is for effective patient care.
Acknowledgements
The author would like to thank Anna Murphy, Grainne d’Ancona and Toby Capstick for reviewing this article
References
[1] Beeching NJ, Fletcher TE & Fowler R. Coronavirus disease 2019 (COVID-19). 2020. Available at: https://bestpractice.bmj.com/topics/en-gb/3000168 (accessed May 2020)
[2] Stewart K, Connelly D & Robinson J. Everything you should know about the coronavirus outbreak. Pharm J 2020;304(7937). doi: 10.1211/PJ.2020.20207629
[3] BMJ Best Practice. Overview of pneumonia. 2020. Available at: https://bestpractice.bmj.com/topics/en-gb/1113 (accessed May 2020)
[4] Nanshan C, Zhou M, Dong X et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7
[5] Centers for Disease Control and Prevention. Symptoms of coronavirus. 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html (accessed May 2020)
[6] Arashiro T, Furukawa K & Nakamura A. COVID-19 in 2 persons with mild upper respiratory tract symptoms on a cruise ship, Japan. Emerg Infect Dis 2020;26(6). doi: 10.3201/eid2606.200452
[7] American Academy of Ophthalmology. Important coronavirus updates for ophthalmologists. 2020. Available at: https://www.aao.org/headline/alert-important-coronavirus-context (accessed May 2020)
[8] WebMD. Coronavirus and COVID-19: What You Should Know. 2020. Available at: https://www.webmd.com/lung/coronavirus (accessed May 2020)
[9] Public Health England. Coronavirus (COVID-19): getting tested. 2020. Available at: https://www.gov.uk/guidance/coronavirus-covid-19-getting-tested (accessed May 2020)
[10] Public Health England. Stay at home: guidance for households with possible coronavirus (COVID-19) infection. 2020. Available at: https://www.gov.uk/government/publications/covid-19-stay-at-home-guidance/stay-at-home-guidance-for-households-with-possible-coronavirus-covid-19-infection (accessed May 2020)
[11] NHS. What to do if you or someone you live with has symptoms of coronavirus. 2020. Available at: https://www.nhs.uk/conditions/coronavirus-covid-19/self-isolation-advice (accessed May 2020)
[12] The Pharmaceutical Journal. COVID-19 latest: Police in Wales to offer reassurance and advice on pharmacy safety during pandemic. Pharm J 2020;304(7937). doi: 10.1211/PJ.2020.20207843
[13] NHS. Check if you have coronavirus symptoms. 2020. Available at: https://www.nhs.uk/conditions/coronavirus-covid-19/symptoms-and-what-to-do (accessed May 2020)
[14] National Institute for Health and Care Excellence. COVID-19 rapid guideline: managing suspected or confirmed pneumonia in adults in the community. NICE guideline [NG165]. 2020. Available at: https://www.nice.org.uk/guidance/ng165/chapter/3-Diagnosis-and-assessment (accessed May 2020)
[15] The Centre for Evidence-Based Medicine. Are there any evidence-based ways of assessing dyspnoea (breathlessness) by telephone or video? 2020. Available at: https://www.cebm.net/covid-19/are-there-any-evidence-based-ways-of-assessing-dyspnoea-breathlessness-by-telephone-or-video (accessed May 2020).
[16] World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected. 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/clinical-management-of-novel-cov.pdf?sfvrsn=bc7da517_10&download=true (accessed May 2020)
[17] National Institute for Health and Care Excellence. Pneumonia in adults. Quality standard [QS110]. 2016. Available at: https://www.nice.org.uk/guidance/qs110/chapter/Quality-statement-1-Mortality-risk-assessment-in-primary-care-using-CRB65-score (accessed May 2020)
[18] NHS. Pneumonia: treatment. 2019. Available at: https://www.nhs.uk/conditions/pneumonia/treatment (accessed May 2020)
[19] Joint Formulary Committee. British National Formulary. 79 edn. London: BMJ Group and Pharmaceutical Press; 2020
[20] NHS. Doxycycline. 2018. Available at: https://www.nhs.uk/medicines/doxycycline (accessed May 2020)
[21] eMC. Doxycycline 100mg capsules. 2019. Available at: https://www.medicines.org.uk/emc/product/4063/smpc (accessed May 2020)
[22] Antibiotic Research UK. Coronavirus (COVID-19). 2020. Available at: https://www.antibioticresearch.org.uk/coronavirus (accessed May 2020)
[23] British Lung Foundation. Recovering from pneumonia. 2019. Available at: https://www.blf.org.uk/support-for-you/pneumonia/recovery (accessed May 2020)


