This content was published in 2013. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
This week in England, the sun rose over a sparkling new NHS. Or, at least, the NHS structure that was set out in the much-contested Health and Social Care Act 2012 is now in place. Ten strategic health authorities and 152 primary care trusts are no more, and a host of new organisations have formally taken up their functions.
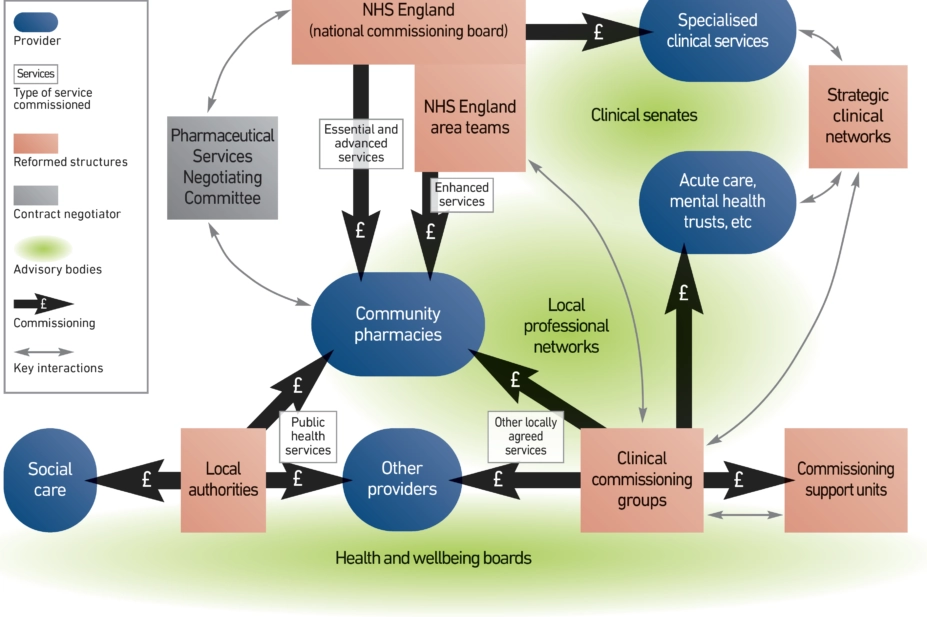
Many of these new bodies are still finding their feet, and much work remains to be done. The Journal plans to set out some of the remaining challenges and opportunities in more detail over the coming weeks. In the meantime, this overview — and the Agenda article on p374 — should help you navigate your way around the new NHS landscape and understand how you can, and should, influence the many changes that are still to come.
NHS England
NHS England — known until last week as theNHS Commissioning Board — is a key part of the new commissioning structure, in charge of handling the £12.6bn primary care commissioning budget, setting the strategy for primary care in England and maintaining a single operating model for service commissioning.
Bringing these responsibilities together under one organisation is intended to ensure national consistency and standards in primary care.
NHS England is the new negotiating partner for the Pharmaceutical Services Negotiating Committee (see Panel) on the terms of the community pharmacy contract, and will continue to use the NHS Business Services Authority for pharmaceutical payments. It is tasked with progressing the “quality, innovation, productivity and prevention”(QIPP) agenda and commissioning certain public health services at a national level, such as immunisation and screening programmes.
Selected patient safety functions formerly fulfilled by the National Patient Safety Agency now reside within NHS England. IT services, including the electronic prescription service and NHS mail, also fall under the commissioning board’s remit, although it is expected to farm these duties out to local bodies.
NHS England area teams
Beneath NHS England’s national structure sit27 area teams that will handle, among other tasks, the day-to-day development and commissioning of pharmaceutical services within their regions.
They are responsible for developing and engaging with local professional networks (LPNs), which are a key means for pharmacists to engage with and inform the commissioning process. Area teams are also in charge of emergency planning, assuring the quality of clinical commissioning groups and managing the national performers list for GPs, dentists and ophthalmic practitioners. Since there is no such list for pharmacists, area teams will work closely with the General PharmaceuticalCouncil to manage pharmacists’ performance.
Local professional networks
Local pharmaceutical, dental and optical networks are a means for professionals in each of these healthcare disciplines to influence commissioning. They are not intended to be stand-alone organisations, but to be integral to NHS England’s area teams and how those teams operate. Each LPN will use a tiered structure to gain access to clinicians offering NHS services inits area, both in primary and secondary care. The networks should be a two-way street: as well as providing clinical leadership, they are a means for care providers to pass their ideas to commissioners. If harnessed effectively, the networks can be used to promote pharmacy’s role in improving medicines use and supporting wellness — through, for example, the healthy living pharmacy model.
Clinical commissioning groups
Clinical commissioning groups are responsible for funding a host of services that do not fall into the public health or pharmaceutical services remit. These include planned hospital care, emergency and out-of-hours care, mental health and learning disability services and a range of community health services, such as rehabilitation and continence services. CCGs can commission from any qualified provider, meaning pharmacies bidding for CCG funds will face competition from other providers, including social enterprises, charities and private companies (which might also employ pharmacists).
Each CCG board includes at least two lay members, one registered nurse and one specialist secondary care doctor. To avoid conflicts of interest, none of the board members is allowed to be employed by any of the commissioned service providers. There are no reserved spots for pharmacists, so the profession will need to be actively engaged with CCG commissioning partners and processes.
By mid-March, NHS England had authorised all 211 of the CCGs to take on their commissioning responsibilities. However, many still have conditions that they need to meet before they will be granted full authorisation— meaning they have not yet satisfied all 119 of the criteria by which they are judged.
Some pharmacists who formerly worked in PCT commissioning or medicines management teams have moved into position sat CCGs; others have moved to commissioning support units (CSUs).
Commissioning support units
CSUs are there to underpin the work carried out by CCGs, by providing them with a range of support services. These include IT and accounting services, business intelligence, management support and analyses of data to establish local health needs.
Thousands of the staff who provided these services as part of SHAs and PCTs have been absorbed into CSUs, which are now hosted by NHS England with the NHS BSA acting as the legal employer — which means staff in the units are still receiving NHS pay and pensions. However, the idea is that by 2016 all the CSUs will become fully autonomous.
There is no model CSU structure, but the units need to be set up in a way that reflects local needs, resources and strategies. CCGs are free to choose whether to contract services from the non-statutory CSUs and must be able to justify their running costs, so the units need to be run commercially.
Health and wellbeing boards
Local authorities are responsible for commissioning public health services from a budget that has been ring-fenced at £5.45bn over the next two financial years. With this, they are expected to co-ordinate local efforts to improve people’s wellbeing and reduce health inequalities by commissioning services in areas such as smoking, obesity, sexual health and drug and alcohol misuse — although they might agree joint commissioning arrangements with CCGs for these services.
Each local authority has a health and wellbeing board (HWB), among whose tasks are producing and maintaining pharmaceutical needs assessments (PNAs). These reviews of local need will be used by NHS England area teams to inform the commissioning of pharmaceutical services and govern market entry and exit.
HWBs will also produce joint strategic needs assessments (JSNAs) and joint health and wellbeing strategies (JHWSs), on behalf of CCGs and local authorities. JSNAs will gauge local health and social care needs, taking into account wider determinants such as employment, transport and housing, andJHWSs will set out plans to build services around these needs and measure improvements.By law, HWBs must include at least one local elected representative and Healthwatch representative, as well as the local authority directors for adult services, children’s services and public health and a representative from each local CCG. There is no legal requirement for pharmacist involvement, but the boards are free to expand their membership to include a range of expertise, so there are opportunities to get involved.
Strategic clinical networks
Hosted and funded by NHS England, strategic clinical networks bring together healthcare professionals from a range of NHS organisations to share best practice and promote innovation in relation to particular disease areas or patient groups, including cancer, cardiovascular disease, mental health and maternity and children’s services.
Their aim is to ensure high-quality and seamless care in these clinical areas, by providing local commissioners with advice that takes into account the overall care pathway and patient journey. In order to minimise variations in care the networks have a single operating framework, covering areas such as accountability, governance and evaluation of effectiveness.
NHS England is providing 12 regional support teams, located within area team offices, to help build and oversee the networks. These will be funded using the £42m that NHS England has put aside to support the strategic clinical networks, along with clinical senates.
Clinical senates
Also hosted and funded by NHS England, clinical senates bring healthcare specialists together to share clinical knowledge and to inform service commissioning and design. However, rather than focusing on a particular health condition, the senates take a broader, more strategic view of healthcare within each of 12 geographical areas.
Clinical senates are expected to maintain close links to professional bodies and royal colleges. This means that pharmacists who are not directly involved in the senates can influence their work through organisations like the Royal Pharmaceutical Society.
Opportunities for pharmacy
Although the organisations outlined inEngland’s new commissioning structure have distinct remits and reporting lines, in reality they all interact with each other in a range of ways. Moreover, there appears to be huge variation in how the new NHS bodies have been implemented across England.
Although this does create a complex system with no single “in” for pharmacists, it also presents manifold opportunities for the profession to get involved, influence decisions and lead change.
If your knowledge or experiences of the reforms differ from those described in this article, we invite you to share these online or in the letters pages of The Journal (letters@pharmj.org.uk).
The negotiator
The Pharmaceutical Services Negotiating Committee will continue to operate much as it did before the reforms, except it will negotiate with NHS England rather than with the Department of Health.
A spokeswoman for the PSNC said it will continue to work with the DoH on medicines-related issues that have not transferred to NHS England, and will seek to work with Public Heath England “to ensure community pharmacy plays a central role in supporting wellbeing and providing public health services”. She added: “We will be continuing to support local pharmaceutical committees and contractors as they work to secure and offer services locally.”


