This content was published in 2006. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
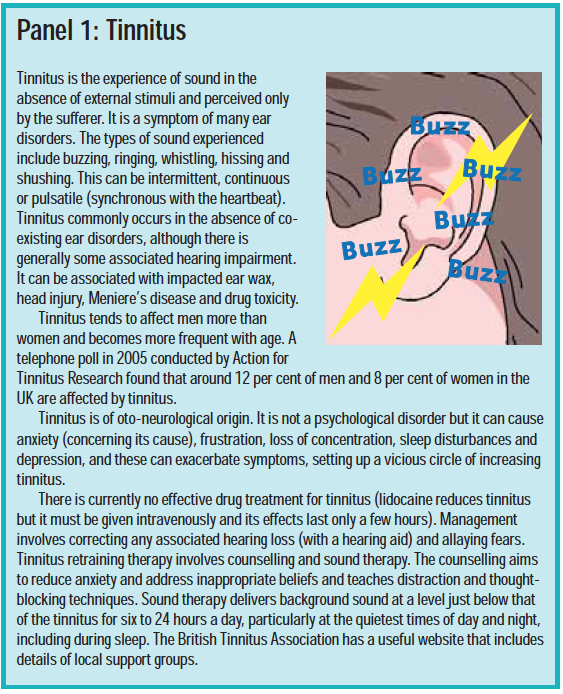
Patients with inner ear disorders may experience disruption of balance and hearing and symptoms such as tinnitus and vertigo. Panel 1 describes tinnitus and Panel 2 describes vertigo.
The inner ear
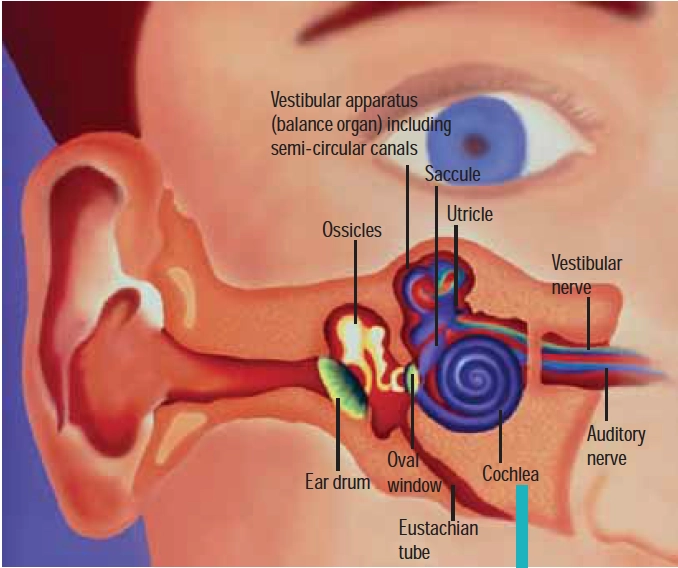
Embedded in bone, the inner ear is a fluid-filled series of chambers, consisting of two parts: the cochlea and the vestibular apparatus. The cochlea is responsible for hearing and consists of a spiral tube about 3.5cm in length. It contains an inner and outer chamber, both of which are filled with fluid. Sound arrives at the oval window via the ossicles and is transmitted through the endolymph in the outer chamber.
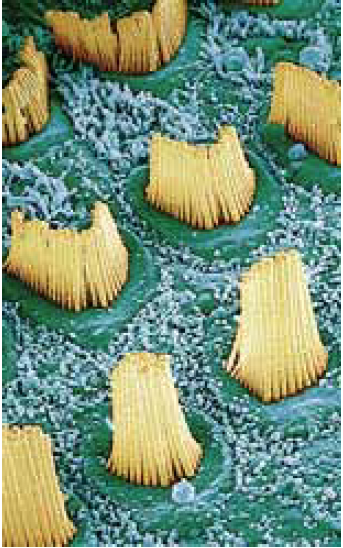
The cochlea’s inner chamber contains the organ of Corti, which is filled with fluid (endolymph) and lined with hair cells. Thousands of tiny hair-like structures, called stereocilia, arise from the hair cells and are projected into the endolymph. The stereocilia respond to different frequencies of sound depending on their location along the spiral tube. Movement of these cells triggers an electrical pulse in the auditory nerve. Hearing impairment is either conductive (where sound cannot pass from the outer to inner ear) or sensorineural (where the problem lies in the cochlea or auditory nerve).
The vestibular apparatus, comprising the saccule, utricle and semicircular canals, is not involved in hearing. It is part of the balance system. Like the cochlea, the canals of the vestibular system are filled with endolymph and have stereocilia projecting into them. When the head is moved, the stereocilia shift and an electrical impulse is sent via the vestibular nerve to the brain, giving vital information about orientation and allowing balance to be maintained.
Identify knowledge gaps
- What are the symptoms of Meniere’s disease?
- How can vertigo be treated?
- List three ototoxic drugs.
Before reading on, think about how this article may help you to do your job better. The Royal Pharmaceutical Society’s areas of competence for pharmacists are listed in “Plan and record”, (available at: www.rpsgb.org/education). This article relates to “common disease states”.
Meniere’s disease
Meniere’s disease is a progressive disorder of the inner ear of unknown cause. Although commonly beginning between the ages of 20 and 50 years, it can occur at any age (it is rare in childhood), and can affect one or both ears.
Meniere’s disease is thought to be connected to a build up of fluid in the membranous labyrinth surrounding the cochlea andvestibular apparatus. The symptoms vary between patients, but are characterised by episodes of vertigo (causing dizziness, nausea and vomiting), dulled hearing, tinnitus and a feeling of pressure in one or both ears. Most patients (70 per cent) also suffer associated headaches. Attacks can be frequent or may only occur every few months, and each one can last from 20 minutes to several hours. Disease progression tends to follow a predictable course. Early on, there are sudden, erratic episodes of vertigo, temporary hearing loss and tinnitus. As time goes on, hearing becomes increasingly affected and there is sensorineural hearing loss of the lower pitches. Sudden attacks of vertigo are at their most severe, although there may be periods of remission (up to several months). In the later stages of the disease, hearing loss becomes more significant and permanent. Tinnitus islikely to remain although the episodes of vertigo can diminish.

The erratic nature of Meniere’s disease can cause great distress and affect quality of life. Sudden attacks of vertigo can cause patients to fall and mean that they should exercise caution when swimming or using ladders etc. People with Meniere’s disease also need to inform the Driver and Vehicle Licensing Agency of their condition.
Management
Management of Meniere’s disease can be complicated because of the erratic nature of attacks. One Cochrane systematic review found little evidence as to the effectiveness of the various treatments used in terms of tinnitus or deafness. Acute attacks of vertigo tend to be managed with prochlorperazine or cinnarizine (see Panel 2). There are advantages with prochlorperazine because it can be administered buccally and rectally for patients whose vertigo is accompanied by nausea and vomiting, but it is associated with more side effects, especially in elderly patients. As with migraine, many Meniere’s patients experience an aura before an attack, and the best results are seen if medicines are taken at this point.
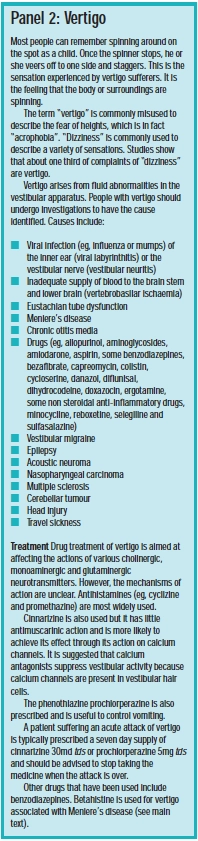
Some patients take prophylactic medicine. Betahistine is commonly prescribed. A recent, randomised controlled study (81 patients) has found a statistically significant reduction in the number and intensity of vertigo attacks in patients taking 16mg betahistine twice daily for three months. Headache was a common adverse effect. The British National Formulary recommends a maintenance dose of 24–48mg daily, with food. Betahistine is thought to work by reducing the fluid pressure in the inner ear.
Ear, nose and throat consultants can try a number of other drugs to manage the symptoms of Meniere’s disease. These include diazepam (which suppresses vestibular activity) and corticosteroids. Occasionally, radicalablative medical procedures (eg, application of topical gentamycin), or surgical procedures to destroy vestibular function but maintain hearing, are necessary to manage severe vertigo.
Some patients find that elements of their diet trigger attacks in a similar way to migraine sufferers, although no direct link between diet and Meniere’s has been found. However, a low salt diet may be helpful and diuretics, in conjunction with salt restriction, are sometimes prescribed. The proposed mechanism behind this treatment is that the diuretic affects the amount of potassium int he endolymph, which may be the cause of hair cell inhibition.
Benign paroxysmal positional vertigo
Benign paroxysmal positional vertigo (BPPV) is a common type of vertigo and can present at any time, although it becomes more common with age. Typically, patients complain of extreme dizziness or a spinning sensation for less than one minute when turning over in bed. There may also be giddiness when tipping the head to look upwards. BPPV is episodic and tends to occur in clusters separated by weeks or months.
BPPV is diagnosed using Hallpike’s manoeuvre. The patient sits on a bed and then lies back quickly to let his head overhang the bed at about 45 degrees from the horizontal. At the same time the head is rotated by 45 degrees. After about 10 seconds, a patient with BPPV will experience vertigo and nystagmus (rapid and jerky eye movements) downwards towards the affected (lower) ear.
BPPV is caused by the presence of calciumcarbonate crystals (otoconia) in the semicircular canals of the inner ear. Many patients are successfully treated with the Epley manoeuver, a sequential movement of the head through four positions. This rotates the semi-circular canal, repositioning the offendingcrystal(s) to where they do not produce symptoms.
If untreated, most patients’ symptoms resolve in between six and eight weeks. This may take longer if the patient is elderly.
Hearing impairment and deafness
There are an estimated 8.7 million deaf and partially hearing people in the UK. About 673,000 of these are profoundly deaf. The most common cause of hearing loss is advancing age — more than 50 per cent of people over 60 years old have some hearing impairment. Progressive loss of hearing that occurs with age is known as “presbyacusis” and higher frequencies are usually most affected. Other common causes of deafness in adults include:
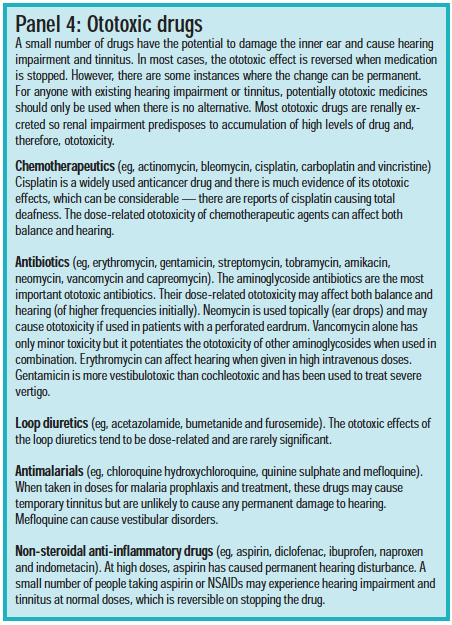
- Adverse drug reactions
- Meniere’s disease
- Acoustic neuroma (a benign tumour)
In children, causes of deafness include inherited conditions, infection in utero(eg,rubella), glue ear, meningitis and head injury.
Conductive hearing loss can be caused byexcessive wax in the ear or glue ear (PJ, 21January, pp83–6). Sensorineural hearing loss may be either sensory (cochlear) or neural (eighth nerve) in origin. Causes of sensory hearing loss include end organ lesions due to acoustic trauma (see Panel 3), viral labyrinthitis, ototoxic drugs (see Panel 4) and Meniere’s disease. Neural hearing loss is frequently due to a brain tumour or other neurological disorder.

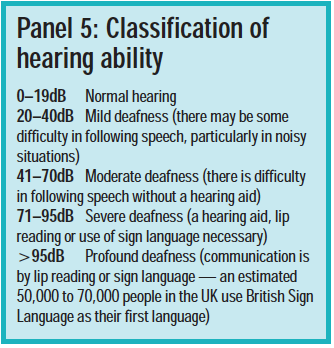
Individuals experiencing impaired hearing should be referred to an audiology clinic for the nature and extent of their loss to be identified. The level of deafness is defined according to the quietest sound, in decibels (dB), which can be heard across a range of frequencies (see Panel 5).
Hearing aids
A hearing aid can only enhance hearing. It does not restore it to normal. About two million people in the UK have hearing aids, but only 1.6 million use them. There are at least another three million people who experience significant hearing difficulties in everyday life and would benefit from a hearing aid.
A wide range of technologies exist for hearing aids, but in its simplest form, each consists of a microphone, an electronic amplifier, a loudspeaker and a battery. The aid can be either analogue (radio waves) or digital. Digital aids use more advanced technology and include a computer that can be programmed to enhance hearing to meet individual needs (ie, focusing on frequencies affected). They may also automatically switch programme according to listening conditions (eg, with or without background noise). Just like their analogue forerunners, digital hearing aids come in behind-the-ear, in-ear, or in-canal models. The problem of “whistling” (feedback) associated with hearing aids has been reduced with digital technology. Hearing aid services are currently being modernised across the UK and digital hearing aids are now available on the NHS, although there can be a long wait. Private hearing aid dispensers offer more choice of device and reduced waiting times. If purchased independently, the price for programmable sophisticated digital technology ranges from £300 to £2,500.
Some ear drops contain ingredients that destroy plastic so some hearing aids should not be used while ear drops are used. Wearing a hearing aid during an ear infection can also present a potential for reinfection.
Cochlear implants
A cochlear implant can give a sense of hearing to severely or profoundly deaf people who have cochlea damage but a functioning auditory nerve. The implant consists of an external and an internal part. The external part is worn on the ear, like a conventional hearing aid, or clipped to the clothes. It includes a sound processor to convert sound into an electrical signal, which it sends to the internal part. The internal part is surgically implanted into the ear and transmits the electrical signal from the external processor to the auditory nerve, bypassing damaged hair cells in the cochlea.
Resources
- Prodigy guidance for Meniere’s disease. Available at: www.prodigy.nhs.uk (accessed 12 January 2006).
- The British Tinnitus Organisation (www.tinnitus.org.uk) provides help and information for people with tinnitus.
- Tidy C. Vertigo. Available at: www.patient.co.uk (accessed 12 January 2006).
- A selection of factsheets and leaflets are available from the Royal National Institute for Deaf People (www.rnid.org.uk).
Action: practice points
Reading is only one way to undertake CPD and the Society will expect to see various approaches in a pharmacist’s CPD portfolio.
- Read the medicines management issues regarding cinnarizine and prochloperazine in the Prodigy guidance for Meniere’s disease and apply these to your practice.
- Next time you dispense betahistine, talk to the patient about how his or her condition has been managed.
- Find contact details for the hearing aid centre closest to you.
Evaluate
For your work to be presented as CPD, you need to evaluate your reading and any other activities. Answer the following questions: What have you learnt? How has it added value to your practice? (Have you applied this learning or had any feedback?) What will you do now and how will this be achieved?
You might also be interested in…
Pharmacists join cast of antimicrobial resistance musical

The engagement imperative
