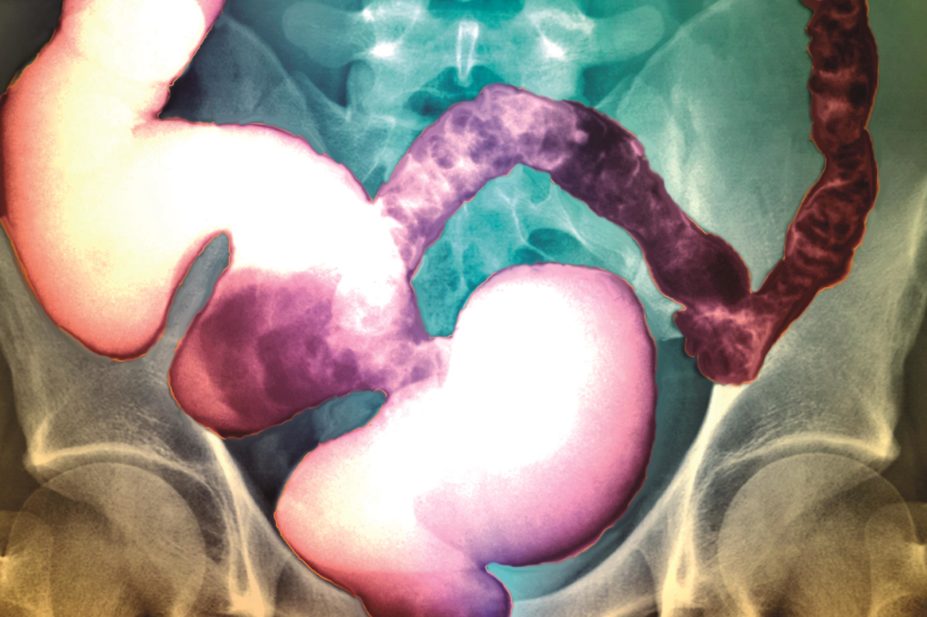
Sovereign, ISM / Science Photo Library
In this article you will learn:
- The licensed uses of the latest medicines used in managing constipation
- How linaclotide, lubiprostone and prucalopride may interact with common medicines
This article focuses on some of the interactions associated with the latest medicines for the management of constipation: linaclotide, lubiprostone and prucalopride.
Linaclotide, a guanylate cyclase-C agonist, is licensed in the UK for the symptomatic treatment of moderate to severe irritable bowel syndrome (IBS) with constipation in adults. In the United States, it is additionally licensed for chronic idiopathic constipation[1]
. It exerts its laxative effect by increasing chloride and bicarbonate secretion into the intestine[2]
.
Lubiprostone is a chloride-channel activator that increases chloride concentration in the intestinal fluid[3]
, increasing fluid secretion and resulting in increased gastrointestinal motility. It is licensed in the UK for chronic idiopathic constipation in adults, and in the United States it is additionally licensed for opioid-induced constipation in adults with non-cancer pain and for IBS with constipation in women aged over 18 years[4]
.
Prucalopride is a selective serotonin 5-HT4-receptor agonist that stimulates colonic motility. It is licensed in the UK and Canada for chronic constipation in women in whom laxatives have failed to provide an adequate response; it is not licensed in the United States[5],[6]
.
Pharmacodynamic interactions
Patients can develop diarrhoea as a side effect of medicines used for the management of constipation. Diarrhoea can affect the absorption, and therefore the efficacy, of many other medicines a patient may also be taking.
The manufacturers of linaclotide and prucalopride advise that the efficacy of oral contraceptives used concurrently may be reduced if severe diarrhoea occurs as a side effect of treatment. If diarrhoea is severe or prolonged, additional contraceptive methods (e.g. condoms) should be used[2],[5]
. Women using oral contraceptives who have severe diarrhoea for more than 24 hours should follow the instructions and precautions for a missed contraceptive pill (which varies depending on the type of contraceptive pill taken)[7]
.
The manufacturer of linaclotide also advises that diarrhoea may reduce the efficacy of any concurrent medicines with a narrow therapeutic range, such as levothyroxine. The concurrent use of non-steroidal anti-inflammatory drugs (NSAIDs), other laxatives and proton pump inhibitors with linaclotide can also increase the risk of diarrhoea
[2]
.
Linaclotide has been found to cause more gastrointestinal adverse events and looser, more frequent stools when taken after a high-fat meal compared with taking it in a fasting state. Linaclotide should therefore be taken 30 minutes before a meal[2]
.
Studies have found that taking lubiprostone with food decreases the maximum serum concentration of lubiprostone by 55%, but does not alter its overall exposure. The clinical relevance of this change is unclear; however, the manufacturer advises that taking lubiprostone with food may reduce any nausea, which is a possible side effect of treatment[3]
.
The efficacy of lubiprostone may be reduced by diphenylheptane opioids (i.e. methadone)[4]
. This effect is dose-dependent (i.e. the greater the dose of methadone given, the greater the reduction in lubiprostone efficacy). An in vitro study found that methadone inhibited the activation of chloride channels in the gastrointestinal tract by lubiprostone, which would oppose its mechanism of action[8]
. The clinical relevance of this theoretical interaction has not been established, although health professionals should consider using an alternative treatment for constipation in patients taking methadone.
The 5-HT4-receptor agonist effect of prucalopride results in the release of acetylcholine. Therefore, the concurrent use of antimuscarinics (e.g. atropine) may antagonise the prokinetic effect of prucalopride, whereas concurrent use of acetylcholinesterase inhibitors (e.g. donepezil) may potentiate the effect[9]
. The clinical relevance of these interactions has not been established. Until more is known, the possibility of an interaction should be considered if a patient has an unexplained change in response to prucalopride while also taking an antimuscarinic.
Pharmacokinetic interactions
A large amount of the data regarding the possible pharmacokinetic interactions of linaclotide, lubiprostone and prucalopride comes from in vitro studies. Although this is a useful guide, in vitro results do not always reflect what happens in clinical use. This data should therefore be interpreted with caution until clinical studies establish an effect.
In vitro studies suggest that linaclotide (and its active metabolite, des-tyrosine), lubiprostone and prucalopride do not affect the cytochrome P450 enzyme system[2],[3],[5]
. Therefore, potential drug interactions via these mechanisms are unlikely to occur in vivo.
Linaclotide is metabolised to its primary active metabolite des-tyrosine within the gastrointestinal tract, and both compounds are undetectable in the plasma after therapeutic doses[2]
minimising the likelihood of a pharmacokinetic interaction. In addition, linaclotide is not an inhibitor or a substrate of P-glycoprotein[1]
, and so in vivo interactions via this mechanism are not expected.
While prucalopride does not inhibit P-glycoprotein when it is taken at its recommended doses, it may be a weak P-glycoprotein substrate[5]
(i.e. it is transported out of the cell by P-glycoprotein). Ketoconazole has been shown to increase prucalopride exposure by 40%[5]
, possibly by inhibition of renal P-glycoprotein, and the manufacturer notes other potent inhibitors of P-glycoprotein (e.g. ciclosporin and verapamil) would be expected to interact similarly[5]
. This small increase in prucalopride exposure is unlikely to be clinically relevant, and prucalopride dose adjustments are not necessary when using these medicines concurrently. However, this interaction should be considered if the patient experiences increased adverse effects related to prucalopride (e.g. nausea, fatigue, dizziness) when taking these medicines.
There has been a report of a 40% increase in maximum concentration and a 28% increase in the area under the curve (a measure of total exposure) in erythromycin when used concurrently with prucalopride. The pharmacokinetics of prucalopride were unaffected. The increases reported were considered to be most likely caused by the interindividual variability of the pharmacokinetics of erythromycin rather than an interaction[6]
.
However, as erythromycin (particularly when given intravenously) has been associated with an increase in the QT interval, any increase in erythromycin concentrations caused by prucalopride may further increase the risk of QT prolongation. Monitoring with an electrocardiogram should be considered in patients with risk factors for QT interval prolongation (e.g. older age, female sex, cardiac disease, hypokalaemia) if they are taking erythromycin concomitantly with prucalopride.
The manufacturers of prucalopride previously advised caution on concurrent use with medicines that prolong the QT interval, although studies have now shown that, at therapeutic doses, prucalopride alone does not increase the QT interval compared with placebo[6]
.
As yet, no pharmacokinetic interactions have been reported for linaclotide or lubiprostone.
This article has been produced by Rebekah Raymond, Harpreet Sandhu and Claire L Preston on behalf of the Stockley’s Drug Interactions editorial team. The book is available in print through
www.pharmpress.com
or electronically with quarterly updates through www.medicinescomplete.com.
References
[1] Forest Pharmaceutical Inc. Linzella (Linaclotide). US Prescribing information. July 2014.
[2] Almirall Ltd. Constella (Linaclotide). UK Summary of product characteristics. March 2014.
[3] Sucampo Pharma Europe Ltd. Amitiza (Lubiprostone). UK Summary of product characteristics. October 2013.
[4] Sucampo Pharma Americas LLC. Amitiza (Lubiprostone). US Prescribing information. April 2013.
[5] Shire Pharmaceuticals Ltd. Resolor (Prucalopride succinate). UK Summary of product characteristics. July 2014.
[6] Janssen Inc. Resotran (Prucalopride succinate). Canadian product monograph. August 2014.
[7] Faculty of Sexual and Reproductive Healthcare Guidance. Drug interactions with hormonal contraception: Clinical Effectiveness Unit. January 2011.
[8] Cuppoletti J, Chakrabarti J, Tewari K et al. Methadone but not morphine inhibits lubiprostone-stimulated Cl- currents in T84 intestinal cells and recombinant human ClC-2, but not CFTR Cl- currents. Cell Biochem Biophys 2013;66:53–63.
[9] European Medicines Agency. CHMP assessment report for Resolor. Procedure No. EMEA/H/C/1012.


