Riccardo Cassiani-Ingoni / Science Photo Library
In this article you will learn:
- How multiple sclerosis is diagnosed
- The treatment options available to manage acute symptoms
- The disease modifying therapies used in long-term treatment
Multiple sclerosis (MS) is an autoimmune inflammatory disease of the central nervous system (CNS). The cause of MS is unknown, but there is thought to be a combination of environmental and genetic factors. Approximately 2.3 million people worldwide (100,000 people in the UK) are affected by MS. It is the most common cause of non-traumatic disability in young adults, and the average age of clinical onset is 30 years[1]
.
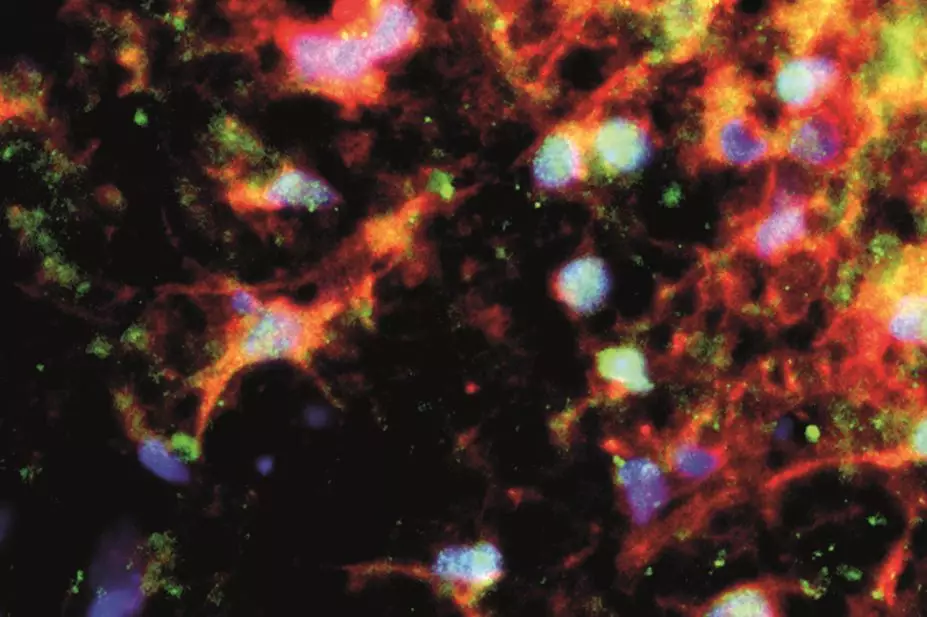
The basic functional unit of nervous tissue is the neuron. A neuron is made up of a nerve cell body plus small branches called fibres. One type of fibre, the dendrite, carries nerve impulses to the nerve cell body. A single fibre, the axon, carries impulses away from the nerve cell body. Some axons are covered with a fatty material called myelin that insulates and protects the fibre. Myelinated axons are called white fibres (because of the colour of myelin) and are found in the white matter of the brain and spinal cord.
In MS the immune system attacks and damages myelin, oligodendrocytes (myelin producing cells) and axons. This in turn interferes with conduction of impulses along the nerve fibre, resulting in a range of disabling neurological symptoms that vary from one person to another depending on where the damage has occurred.
Symptoms of MS include[2],[3]
:
- Balance impairment;
- Motor symptoms – lack of mobility, muscle cramping secondary to spasticity, muscle weakness, paralysis;
- Autonomic symptoms – bladder, bowel and sexual dysfunction;
- Cerebellar symptoms – dysarthria, ataxia, tremor;
- Optic neuritis;
- Constipation;
- Trigeminal neuralgia;
- Fatigue;
- Dizziness;
- Neuropathic pain;
- Emotional lability and depression;
- Cognitive impairment.
The CNS can restore function by remyelinating the axons. After remyelination, function is restored but may not be as quick or as efficient. Permanent loss of function in MS is caused by failure to remyelinate, which in turn leads to axonal loss and neuronal death.
Types of multiple sclerosis
Four disease courses have been identified in MS[4]
.
Relapsing-remitting MS (RRMS) is characterised by clearly-defined periods of worsening neurological function (relapse), which are followed by periods of partial or complete recovery (remission) without apparent disease progression. Around 85% of patients with MS have RRMS at the time of diagnosis.
Secondary-progressive MS (SPMS) occurs in around 60–70% of patients with RRMS, typically 10–30 years after initial onset. SPMS is characterised by gradual disease progression with or without relapses.
Primary-progressive
MS (PPMS) is characterised by steady disease progression and worsening neurological function from onset, with no distinct periods of relapse or remission. Around 10% of MS patients have PPMS.
Progressive-relapsing
MS (PRMS) is characterised by steadily worsening neurological function from the onset with occasional relapses. Around 5% of people with MS have PRMS.
Diagnosis of MS
A diagnosis of MS should be made by a consultant neurologist following radiology on the basis of established criteria (such as the 2010 revised McDonald criteria for diagnosing MS[5]
) after:
- Assessing that clinical attacks are consistent with an inflammatory demyelinating process;
- Eliminating alternative diagnoses (which can vary depending on the presenting symptoms);
- Establishing that CNS lesions have developed at different times (dissemination in time) and are in different locations (dissemination in space) for a diagnosis of relapsing-remitting MS;
- Establishing that progressive neurological deterioration has occurred over one or more years for a diagnosis of primary-progressive MS.
Acute management
MS relapses are defined as new symptoms (or worsening of existing symptoms) that last for more than 24 hours in the absence of infection or any other cause, after a stable period of at least one month.
Relapses occur as a result of immune-mediated inflammatory attacks that cause damage to CNS myelin. Resulting symptoms are usually related to the area(s) of the CNS affected; e.g. damage to myelin on the optic nerve will cause optic neuritis. Triggers for relapse are thought to include infections, live vaccines, stress, the period immediately after childbirth and vitamin D deficiency.
The severity of relapse can range from very mild exacerbations that do not significantly impact on daily activities to severe exacerbations that interfere with mobility and overall ability to function, such as poor balance, severe muscle weakness, and loss of vision.
Mild exacerbations often do not require treatment. For severe exacerbations, high-dose corticosteroids are used to reduce inflammation and limit the duration of the relapse. The most common treatment options are oral methylprednisolone 500mg once daily for five days, or intravenous methylprednisolone 1g daily for three to five days if a relapse is severe enough to warrant inpatient treatment[3]
. Corticosteroids have no impact on disease progression.
Management of MS symptoms[2],[3]
A range of pharmacological and non-pharmacological options are used to manage MS symptoms, depending on which symptoms affect the patient (see ‘Pharmacological management of multiple sclerosis symptoms’). Non-pharmacological options include physiotherapy, exercise, rehabilitation, occupational therapy and cognitive behavioural therapy (CBT).
Pharmacological management of multiple sclerosis symptoms
| Symptom | Treatment options |
|---|---|
Spasticity | Baclofen, benzodiazepines (e.g. diazepam and clonazepam), dantrolene, gabapentin, tizanidine Patients with severe symptoms may be managed by specialist centres with botulinum toxin injections or baclofen intrathecal infusions administered through an implanted pump Sativex, a cannabinoid oral spray (not considered cost effective by the National Institute for Health and Care Excellence) |
Fatigue | Amantadine |
Bladder dysfunction (e.g. increased frequency, urgency and incontinence) | Antimuscarinics (e.g. oxybutynin, solifenacin, tolterodine) Botulinum toxin type A can be considered where antimuscarinics are not effective or poorly tolerated
|
Lack of mobility | Fampridine (not considered cost effective by the National Institute for Health and Care Excellence) |
Oscillopsia (visual disturbance) | Gabapentin, memantine
|
Emotional lability | Amitriptyline
|
Neuropathic pain | Amitriptyline, carbamazepine, duloxetine, gabapentin, pregabalin
|
Constipation | Combination of stimulant, osmotic and bulk-forming laxatives |
Disease-modifying therapy
Disease-modifying therapies reduce the frequency and severity of MS relapses; reduce the accumulation of CNS inflammatory lesions; and may slow the development of disabling symptoms. Most disease-modifying therapies are indicated for relapsing forms of MS[6]
.
People with progressive MS make up more than 50% of the 2.3 million people with MS worldwide. Despite the wide range of treatment options for relapsing-remitting MS, almost no effective disease-modifying treatment options are available for people with progressive MS[7]
.
Identification of potential therapeutic targets for progressive MS has so far been limited by poor understanding of mechanisms underlying disease progression. The International Progressive MS Alliance, a network of national multiple sclerosis societies, is collaborating with researchers to advance research in this area[8]
.
Disease-modifying therapies are available as self-injectable therapies, oral dose forms and intravenous infusions. Prescribing and monitoring of disease modifying therapy is undertaken by specialist MS multidisciplinary teams. Factors that are taken into account when deciding on the choice of disease therapy include: patient preference, disease stage, contraindications, adverse effects, route of administration, treatment frequency and funding arrangements.
Screening conducted prior to starting disease-modifying therapies
| All therapies | Additional tests |
|---|---|
| Teriflunomide: blood pressure, tuberculosis (active and latent) |
Dimethyl fumarate: urinalysis with microscopy (for potential urinary tract infection or proteinurea, which might indicate kidney damage) | |
Fingolimod: electrocardiogram with first dose, ophthalmologic evaluation for those with history of diabetics or uveitis | |
Natalizumab: John Cunningham Virus serology | |
Alemtuzumab: HIV, Hepatitis B and C, urinalysis with microscopy, thyroid function tests, tuberculosis (active and latent) |
Interferon beta and glatiramer are immunomodulatory drugs indicated for relapsing MS. Interferon beta is thought to act by reducing blood-brain barrier disruption and by modulating T-cell, B-cell and cytokine functions, while glatiramer is thought to act by stimulating regulatory T-cells[9]
,
[10],
[11]
. Treatment options include:
- Interferon beta-1a as once a week intramuscular injections (Avonex) or three-times a week subcutaneous injections (Rebif);
- Interferon beta-1b as alternate day subcutaneous injections (Betaferon and Extavia);
- Peginterferon beta-1a, a pegylated form of beta interferon, approved in July 2014 by the European Medicines Agency and in August 2014 by the US Food and Drug Administration, has a longer duration of action and is administered once every two weeks by subcutaneous injection (Plegridy).
Adverse effects associated with interferon beta include injection site reactions, flu-like symptoms, elevated liver enzymes, a decreased white cell count, low mood and leg stiffness. Patients require regular liver function tests and a full blood count, which are typically conducted at two weeks, one month, two months and six months after starting therapy, and every six months thereafter.
Some patients receiving interferon beta develop neutralising antibodies that may limit the efficacy of treatment[12]
. Plegridy is associated with the lowest incidence (less than 1%) of interferon beta neutralising antibodies, compared with around 30% of people receiving Betaferon and Extavia, 25% receiving Rebif and 5% receiving Avonex[13]
.
Glatiramer is administered three times a week as a subcutaneous injection. Common adverse effects include injection site reactions, lipoatrophy, chest pain, palpitations and anxiety. No ongoing blood monitoring is required for patients receiving glatiramer.
Teriflunomide is an oral disease-modifying treatment indicated for relapsing MS. It works by inhibiting dihydroorotate dehydrogenase, an enzyme required for pyrimidine synthesis in proliferating cells. It is taken as one 14mg tablet once a day[14]
.
Adverse effects of teriflunomide include elevated liver transaminases, liver toxicity, hypertension, nausea, diarrhoea, alopecia, and interstitial lung inflammation. Patients on teriflunomide require regular monitoring, with a full blood count and liver function tests typically every two weeks for six months after starting treatment, and every eight weeks thereafter.
Teriflunomide is teratogenic and has a long half-life (18–19 days) due to enterohepatic recirculation; it takes an average of eight months, or up to two years, to eliminate after discontinuation. It is secreted in semen, and contraception is recommended for both men and women taking teriflunomide. Cholestyramine or activated charcoal may be used to facilitate accelerated elimination if patients become pregnant while on therapy or experience a serious adverse effect such as liver toxicity. The British National Formulary recommends stopping treatment with teriflunomide and giving either colestyramine 8g three times a day for 11 days or activated powdered charcoal 50g every 12 hours for 11 days. This accelerated procedure can also be used if the patient wishes to become pregnant, although a post accelerated elimination teriflunomide plasma concentration of less than 20mcg/l and a waiting period of at least one and a half months before conception is necessary.
Dimethyl fumarate is indicated for relapsing MS. It promotes a shift of cytokine secretion patterns from predominantly pro-inflammatory cytokines (i.e. interleukin-6, interleukin-12, interferon gamma and tumour necrosis factor alpha) to predominantly anti-inflammatory cytokines (i.e. interleukin-4, interleukin-5, interleukin-10)[15]
. Dimethyl fumarate is metabolised to monomethyl fumarate, an active metabolite that is eliminated through respiration.
Patients initially start dimethyl fumarate at a dose of 120mg orally twice a day, which is increased after seven days to 240mg twice a day. Treatment is generally well tolerated.
The most frequently reported side effects are flushing and hot flushes, and gastrointestinal adverse effects (e.g. abdominal pain, diarrhoea, nausea and vomiting). These effects are most common during the first month of treatment. Flushing is thought to be a result of dimethyl fumarate’s agonist effect on nicotinic acid receptors, and effects of monomethyl fumarate mediated by prostaglandin E2.
Flushing and gastrointestinal adverse effects may be improved by temporary dose reduction to 120mg twice a day (within the first month) or taking dimethyl fumarate with food. The incidence and severity of flushing can also be reduced by taking low-dose aspirin (e.g. 75mg) 30 minutes before taking dimethyl fumarate.
Dimethyl fumarate may also cause elevated hepatic transaminases (alanine aminotransferase (ALT) ≥ three times the upper limit of normal), primarily during the first six months of treatment, and a decreased lymphocyte count.
Patients on dimethyl fumarate require regular monitoring of full blood count, urea and electrolytes, urinalysis and liver function tests, typically two weeks after starting treatment, then at one month, three months and six months, then every six months.
Fingolimod is indicated for highly active relapsing MS. It is a sphygosine-1-phosphate (S1P) receptor modulator. Fingolimod interferes with a key mechanism that lymphocytes use to exit lymph nodes. This leaves lymphocytes unavailable for entering the CNS to initiate MS lesions. Treatment with fingolimod should be initiated and supervised by a specialist. It is taken as one 500mcg oral tablet once a day[16]
.
Fingolimod is contraindicated in patients with known immunodeficiency, severe active infection, active chronic infections (hepatitis, tuberculosis), severe liver impairment, and active malignancies.
Adverse effects of fingolimod reflect the fact that subtypes of S1P receptors are expressed on various other tissues. These include elevated liver transaminases; macular oedema; reduced white cell count; bradycardia; increased risk of infection (notably from varicella zoster and herpes simplex); minor reduction in forced expiratory volume (fingolimod should be used with caution in patients with severe respiratory disease, pulmonary fibrosis and chronic obstructive pulmonary disease); and haemophagocytic syndrome, a rare but potentially fatal disease.
Fingolimod affects cardiac smooth muscle and is known to cause bradycardia and heart block after the first dose. It is not recommended in patients with:
- Second degree Mobitz Type II or higher degree atrioventricular block, sick sinus syndrome or sinoatrial heart block;
- Significant QT prolongation (more than 470ms in women, more than 450ms in men);
- History of symptomatic bradycardia, recurrent syncope, ischaemic heart disease, cerebrovascular disease, history of myocardial infarction, congestive heart failure, cardiac arrest, uncontrolled hypertension or severe sleep apnoea.
Fingolimod is contraindicated in patients taking class 1a or class III antiarrhythmic medicines; beta blockers; heart rate-lowering calcium channel blockers; and other medicines that may decrease heart rate.
When starting treatment with fingolimod, patients require continuous cardiac monitoring for at least six hours following their first dose. This should be repeated in all patients whose treatment is interrupted for at least one day during the first two weeks of treatment, more than seven days during weeks three and four of treatment, or more than two weeks after one month of treatment.
Patients taking fingolimod require regular full blood count and liver function tests, typically two weeks after starting treatment, then at months one, two, three, six, nine and twelve, then every six months. Due to risk of macular oedema, eye examinations are recommended three to four months after starting treatment.
Natalizumab is a humanised monoclonal antibody indicated for highly active relapsing MS. It selectively targets alpha-4, a cell adhesion molecule expressed on the surface of lymphocytes and monocytes, preventing migration of immune cells across the blood brain barrier into the CNS[17]
.
A 300mg dose of natalizumab is administered by intravenous infusion once every four weeks. Adverse effects include infusion related hypersensitivity reactions, raised liver function tests, reduced white cell count, and increased risk of infection.
Around 6% of people receiving natalizumab develop neutralising antibodies that may limit efficacy of the drug.
Natalizumab increases the risk of progressive multifocal leukoencephalopathy (PML), a central nervous system infection with the John Cunningham Virus (JCV), which may lead to irreversible neurological disability or death. Risk factors for PML include prior exposure to JCV, previous treatment with immunosuppressants, and use of natalizumab for more than two years. Early signs of PML include progressive speech deficits, hemiparesis, or seizures.
Patients on natalizumab require routine monitoring. This typically involves a monthly full blood count, liver function tests every three months, JVC serological testing (if JVC seronegative) every six months, and a magnetic resonance imaging scan for evidence of PML every six months (if JVC seropositive), or every twelve months (if JVC seronegative).
Alemtuzumab (indicated for active relapsing MS) is a humanised monoclonal antibody that targets the surface molecule of CD52 on T-lymphocytes, B-lymphocytes, monocytes and other immune cells. When administered intravenously, alemtuzumab depletes T- and B-lymphocyte populations for extended periods[18]
.
Alemtuzumab is administered as a once daily 12mg infusion for five consecutive days in year one, followed by a 12mg daily infusion for three consecutive days 12 months later. Alemtuzumab is licensed for only two treatment courses.
Adverse effects include infusion-related hypersensitivity reactions (e.g. rash, pruritus, headache, nausea, diarrhoea, chills, flushing, dizziness, dyspnoea and pyrexia); autoimmune conditions (e.g. thyroid disorders, idiopathic thrombocytopenic purpura, nephropathies); lowered blood cell counts; and infections.
All patients given alemtuzumab are prescribed prophylaxis against herpes zoster or oral herpes with oral aciclovir 200mg twice a day starting on the first day of each treatment course, and continued for at least one month.
The risk of infusion-related hypersensitivity reactions is reduced by administering corticosteroids and antihistamines prior to starting each alemtuzumab infusion.
People being treated with alemtuzumab require ongoing monitoring, including a monthly full blood count with differential, serum creatinine, and urinalysis with microscopy for 48 months after the last infusion. Liver function tests are monitored every three months for 48 months after the last infusion.
Treatment with alemtuzumab is not recommended during pregnancy. Women of childbearing age should be advised to use effective contraception during and for four months after treatment. Autoimmune thyroid disease (which is a potential adverse effect of alemtuzumab) increases the risk of miscarriage and fetal defects.
Olivia Moswela is Lead Directorate Specialist Pharmacist, Neurosciences at Oxford University Hospitals NHS Trust.
Declaration of interests: The author has participated in advisory boards for Novartis and Biogen Idec for which she received an honorarium.
References
[1] Browne P, Chandraratna D, Angood C et al. Atlas of multiple sclerosis 2013: a growing global problem with widespread inequality. Neurology 2014;83:1022–1024.
[2] Feinstein A, Freeman J & Lo AC. Treatment of progressive multiple sclerosis: what works, what does not, and what is needed. The Lancet Neurology 2015;14:194–207.
[3] National Institute of Health and Care Excellence. Multiple sclerosis: management of multiple sclerosis in primary and secondary care. London: NICE 2014.
[4] Lublin F, Reingold S, Cohen J et al. Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology 2014;83:278–286.
[5] Polman CH, Reingold SC, Banwell B et al. Diagnostic criteria for multiple sclerosis: 2010 Revisions to the McDonald criteria. Annals of Neurology 2011;69(2):292–302.
[6] Wingerchuck DM & Carter JL. Multiple sclerosis: current and emerging disease modifying therapies and treatment strategies. Mayo Clinic Proceedings 2014; 89(2):225–240.
[7] Ontaneda D, Fox RJ & Chataway J. Clinical trials in progressive multiple sclerosis: lessons learned and future perspectives. The Lancet Neurology 2015;14:208–223.
[8] Thompson AJ. A much needed focus on progression in multiple sclerosis. The Lancet Neurology 2015;14:133–135.
[9] PRISMS Study Group. Randomised, double blind, placebo controlled study of interferon beta-1a in relapsing-remitting multiple sclerosis. The Lancet 1998;352:1498–1504.
[10] PRISMS Study Group. PRISMS-4: long-term efficacy of interferon-β-1a in relapsing MS. Neurology 2001;56:1628–1636.
[11] INFB Multiple Sclerosis Study Group. Interferon beta-1b is effective in relapsing-remitting multiple sclerosis: clinical results of a multicentre, randomised double blind, placebo controlled trial. Neurology 1993;43:655–661.
[12] Giovannoni G, Munschauer 3rd FE & Deisehammer F. Neutralising antibodies to interferon beta during treatment of multiple sclerosis. Journal of Neurology, Neurosurgery and Psychiatry 2002;73:465–469.
[13] Calabresi P, Kieserer B, Arnold D et al. Clinical efficacy and safety of peginterferon beta-1a in relapsing multiple sclerosis: data from the Pivotal phase 3 ADVANCE study. Neurology 2013;80:S31.006.
[14] O’Connor P, Wolinsky JS, Confavreux C et al. Randomised trial of oral teriflunomide for relapsing multiple sclerosis. New Engl J Med 2011;365:1293–1303.
[15] Burnes CB & Deeks ED. Dimethyl fumarate: A review of its use in patients with relapsing – remitting multiple sclerosis. CNS Drugs 2014;28:373–387.
[16] Kappos L, Radue E-W, O’Connor P et al. A placebo controlled trial of oral fingolimod in relapsing multiple sclerosis. New Engl J Med 2010;362:387–401.
[17] Polman CH, O’Connor PW, Havrdova E et al. A randomised, placebo controlled trial of natalizumab for relapsing multiple sclerosis. New Engl J Med 2006;354:899–910.
[18] Brown JWL & Coles AJ. Alemtuzumab: evidence for its potential in relapsing-remitting multiple sclerosis. Drug Design, Development and Therapy 2013;7:131–138.