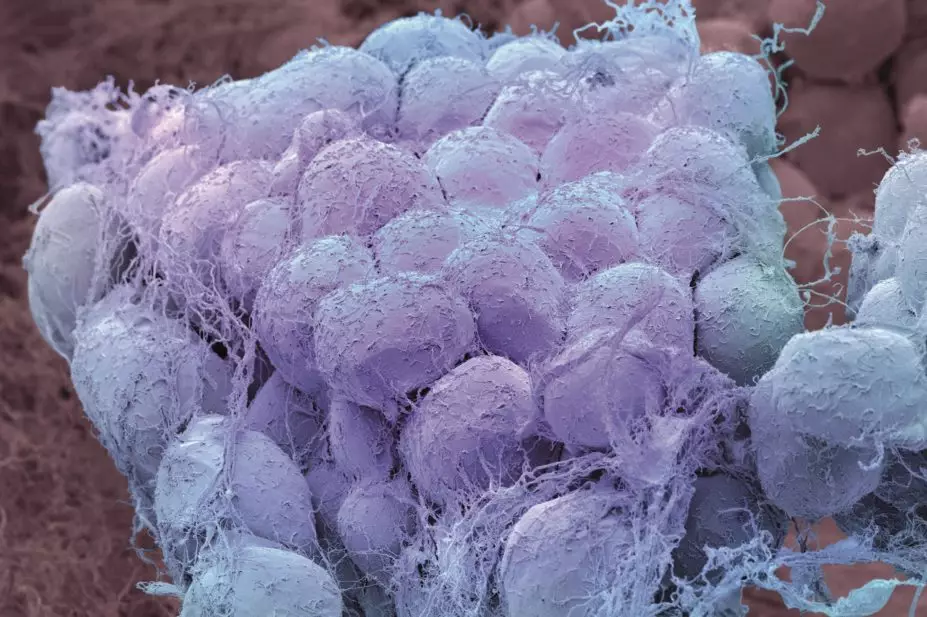
Steve Gschmeissner / Science Photo Library
In this article you will learn:
- How to assess whether a patient is overweight or obese
- Co-morbidities associated with excess weight
- Which medicines are licensed around the world for treating obesity
The causes of obesity are multifactorial and not fully the result of personal responsibility, although poor nutritional intake and sedentary lifestyle play their part. There are strong genetic and epigenetic factors, in addition to the influence of gut hormones, gut microbes and viruses, and environmental factors (such as the promotion of sugar and refined carbohydrates). There is also evidence that psychological and mental health conditions are risk factors for obesity, and vice versa.
The initial stages in obesity treatment focus on diet, physical activity and behavioural techniques. Certain patients who are obese, with or without complications, may be suitable for bariatric surgery — operations that include gastric bypass, sleeve gastrectomy and gastric band, as well as rarer procedures such as biliopancreatic diversion and duodenal switch.
This article focuses on current and emerging drug treatments for people who are overweight or obese.
Epidemiology
According to the World Health Organization, the prevalence of obesity has more than doubled worldwide since 1980; in 2014, more than 1.9 billion adults (39% of all people aged 18 years or older) were overweight, of whom more than 600 million were obese (13% of all adults). The majority of the world’s population live in countries where being overweight and obese causes more deaths than being underweight. Around 42 million children under the age of five years worldwide were overweight or obese in 2013[1]
.
A National Audit Office (NAO) report ‘Tackling obesity in Britain’[2]
estimated that around 6% of all deaths in England in 1998 were caused by obesity — a total of 30,000 per year, compared with approximately 10% attributable to smoking and 1% to road traffic accidents. The NAO analysis showed that many of the deaths caused by obesity were premature, with 9,000 deaths occurring before retirement age. On average, each person whose death could be attributed to obesity lost nine years of life. Since 1998, the prevalence of obesity among English adults increased from 19.4% to over 23.0% (26.0% in men, 23.8% in women[3]
), an 18% increase in relative terms. It therefore seems likely that more than 6% of all deaths in the UK today can be attributed to obesity[4]
. A report by McKinsey Global Institute[5]
stated that obesity is a greater burden on the UK’s economy than armed violence, war and terrorism combined, costing the country nearly £47bn a year.
Assessment
A person’s weight can be assessed by calculating their Body Mass Index (BMI), waist circumference or methods such as bio-impedance analysis (see ‘Body mass index and waist circumference as measures of adiposity’). The best way of identifying a person with excess weight is by observation.
| Body mass index and waist circumference as measures of adiposity | |||
|---|---|---|---|
| Figures are for Caucasians (normal weight figures also given for Asians) | BMI (kg/m2) | Waist circumference (cm) | |
| Men | Women | ||
| Not overweight | <25.0 (18.5–23.0) | <94.0 (<85) | <80.0 (<80) |
| Overweight – pre-obese | 25.0–29.9 | 94.0–101.9 | 80.0–87.9 |
| Overweight – obese | ≥30.0 | ≥102.0 | ≥88.0 |
BMI is ge
nerally considered an adequate research tool but it is flawed in the assessment of an individual, as it does not take into account different body morphologies (e.g. muscle versus adipose); a professional rugby player may have a BMI in the obese range because of their muscular bulk, whereas an otherwise lean individual may have an expande
d abdomen, putting them at high cardiometabolic risk, but have a normal BMI.
Co-morbidities
Possible co-morbidities associated with obesity include type 2 diabetes, and there is evidence linking abdominal obesity to insulin resistance and serious co-morbid disease. The Nurses Health Study[6]
demonstrated an increased risk of diabetes with obesity in women; a relative risk of 93.2 at BMI 35 compared with normal weight. In men, this was assessed by the Health Professionals Study[7]
, which revealed a lesser relative risk of 42.1 at a similar level of BMI.
The Interheart study[8]
demonstrated the importance of abdominal obesity in the pathogenesis of acute myocardial infarction (MI), contributing around 34% of the risk of MI. This risk is closely linked to dyslipidaemia, but once this and other confounding factors are removed, obesity alone contributes 20% of the risk and more than doubles the likelihood of acute MI. Nanchahal et al
[9]
demonstrated an increased prevalence of ten-year chronic heart disease (CHD) risk of >15% with increasing levels of being overweight among men, also demonstrating the link with waist circumference – in this case waist-hip ratio – as opposed to BMI.
Risk of a diagnosis of hypertension is five-fold greater in obese people compared with those of normal weight; more than 85% of cases of hypertension occur in people with a BMI >25. Lipid profile is adversely affected, leading to a profile of small, dense, low density lipoprotein (LDL) particles, low high density lipoprotein (HDL) and raised triglycerides contributing to coronary heart disease.
Other conditions strongly linked to obesity include polycystic ovary syndrome, obstructive sleep apnoea, non-alcoholic steatohepatitis, infertility, mental health problems and a variety of cancers. Obesity increases the risk of endometrial and ovarian cancer, and oestrogen receptor positive, progesterone receptor positive postmenopausal breast cancer. A modest positive association between BMI and cervical cancer has also been found[10]
.
Gastric, oesophageal, colon, prostate, renal cell and hepatocellular cancers have all been linked with excess weight, which can also lead to poorer treatment and increased cancer-related mortality[11]
.
Pharmacotherapy
Drug therapy may be a suitable option for people who have been unsuccessful in losing weight with lifestyle changes. Patients should use medicines in addition to appropriate diet, physical activity and behavioural interventions.
Orlistat is a pancreatic lipase inhibitor that causes around 30% of dietary fat to be excreted unabsorbed in the faeces[12]
. It is available at a dose of 120mg or, in the UK, at 60mg as a P medicine (Alli). It is safe for long-term use, although weight loss is modest (placebo-adjusted weight loss is around 3–4%[13]
). Side effects are common, including oily stools, cramps and occasional faecal incontinence. Risk improvement includes a reduction in the cumulative incidence of diabetes over four years of 37.3% in obese normoglycaemic subjects[14]
, reducing LDL cholesterol by 5–10%, and lowering blood pressure and HbA1c[15]
.
The National Institute for Health and Care Excellence (NICE) supports the use of orlistat in individuals with BMI >30, or >28 with co-morbidities. Treatment should only be continued beyond three months if the person has lost at least 5% of their initial body weight since starting drug treatment[16]
.
The decision to use drug treatment for longer than 12 months, usually for weight maintenance, should be made after discussing potential benefits and limitations with the patient.
More obesity drugs have been withdrawn than licensed by European authorities over recent years (see ‘Withdrawn weight management drugs’).
Withdrawn weight management drugs
Rimonabant was an endocannabinoid receptor blocker that was studied by the Rimonabant in Obesity (RIO) trials, which demonstrated around 8.5–9kg weight loss (around 5kg adjusted for placebo)[17]
. Furthermore, it induced a reduction in HbA1c of up to 1.9% in diabetes[18]
. Early in its lifetime, rimonabant was noted to have links with depressive mood changes. As a result, its licence indications were changed so that a history of depression was an absolute contraindication to its use. Despite its benefits, it was later withdrawn completely because of persistent links with suicidality, rather than being restricted in a similar way to the acne treatment isotretinoin, which has much closer links with depression[19]
.
Sibutramine is a satiety enhancer, which was noted in phase III trials to display a trend in raising blood pressure and heart rate slightly[20]
. Patients taking sibutramine required blood pressure checks every two weeks, and any rise resulted in cessation of treatment. It was also contraindicated in high-risk patients with cardiovascular disease. Treatment was licensed for one year and stopped early in patients who did not respond to treatment.
As part of the licensing commitments, a cardiovascular safety trial – SCOUT[21]
– was carried out. This studied high-risk patients with diabetes and cardiovascular disease who were required to take sibutramine for five years, regardless of whether they responded by losing weight. The initial findings were a possible 16% increase in non-fatal cardiovascular events. This caused the withdrawal of the drug, based on the assumption that anyone who is obese potentially has cardiovascular disease, despite no adverse trends having been noted in the licensed population. However, post-hoc analysis showed that mortality would have been reduced if the SCOUT cohort had been given sibutramine in line with its licence[22]
.
Liraglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist, which is given as a daily subcutaneous injection and has been used as a glucose-lowering agent in diabetes. It has recently been given a positive opinion by the European Medicines Agency (EMA) and is authorised by the US Food and Drug Administration (FDA) as an anti-obesity agent. The EMA states that the mechanism is not entirely understood, but appears to regulate appetite by inducing a feeling of fullness and reducing hunger pains. The EMA recommends it should only be offered to adults with a BMI of more than 30, or 27 if they have a weight-related condition such as type 2 diabetes. Patients should receive a daily 3mg dose, with treatment stopped if body weight has not been reduced by at least 5% after 12 weeks.
In diabetes, as reported by the LEAD series of trials, subjects experienced >5% weight loss during trials. More weight loss was seen with liraglutide 1.2mg and 1.8mg than with active comparators except exenatide[23]
. The SCALE programme has now assessed liraglutide for weight loss in obese patients with or without type 2 diabetes at a higher dose of 3mg daily. In the SCALE maintenance trial, patients who lost at least 5% body weight (up to 6.3kg) in a 12-week intensive diet run-in period then received 3mg liraglutide or placebo daily for 56 weeks. Over 56 weeks, 81% of liraglutide-treated patients maintained this weight loss compared with 49% of placebo-treated patients, and liraglutide-treated patients averaged a further 6.2kg weight reduction, compared with 0.2kg in the placebo arm[24]
.
Several new drugs with prominent weight loss effects and strongly positive risk-benefit profiles have also been turned down in Europe, despite approval in the United States by the FDA.
Lorcaserin is a selective serotonin 2C-receptor agonist and increases satiety. It has been shown to result in a placebo-adjusted weight loss of 3–4kg at one year, alongside improvements in fasting blood glucose, insulin sensitivity, blood pressure, heart rate, total and LDL cholesterol and C-reactive protein levels[25]
.
Diethylpropion and phentermine are sympathomimetic amines, which reduce appetite by eliciting noradrenaline release[26]
. This has been shown to result in a placebo-subtracted weight loss of 7–8kg at 36 weeks[27]
. The potential for addiction or abuse is low, although adverse effects include sympathetic side effects, such as increased heart rate, blood pressure, insomnia, dry mouth, constipation and nervousness, which require close monitoring.
Phentermine was launched in combination with topiramate as Qsymia in the United States in 2012, and induces a placebo-adjusted weight loss of up to 10% of body weight (8–9kg at one year[28]
) alongside risk-factor improvement, including an almost 80% reduction in cumulative incidence of diabetes in an impaired glucose tolerant population, increased HDL, and reduced HbA1c, LDL and blood pressure. Clinical trials that led to its approval include CONQUER, EQUIP, and SEQUEL[29]
. CONQUER[30]
was a 56-week, randomised, double-blind, placebo-controlled, phase III trial in which two Qsymia treatment arms and one placebo arm were initiated in conjunction with a 500 calorie per day dietary deficit. In patients who completed one year of treatment, a reduction in body weight of 12.9kg with phentermine 15mg plus topiramate 92mg, and 9.9kg with phentermine 7.5mg plus topiramate 46mg, was reported compared with 1.8kg in the placebo group. Modest cardiovascular improvements were observed.
Contrave, a combination of the opioid antagonist naltrexone with the dopamine-reuptake inhibitor bupropion, was licensed in the United States in 2014[31]
. Bupropion stimulates the pro-opiomelanocortin (POMC) neuron, which plays a role in the regulation of appetite, while naltrexone prevents inhibition of POMC neurons by blocking the action of ß-endorphin, thus prolonging the effect of bupropion.
This has been shown to result in a placebo-adjusted weight loss of around 6% of body weight at one year.
Drugs that can affect weight
Other glucose-lowering drugs, such as the sodium-glucose co-transporter 2 (SGLT2) inhibitors, induce significant weight reduction, whereas dipeptidylpeptidase-4 (DPP-4) inhibitors and metformin are considered to be weight neutral[32]
. In contrast, other glucose-lowering agents (e.g. insulin, sulphonylureas and pioglitazone) induce weight gain.
Drugs that cause weight gain include corticosteroids, atypical antipsychotics, combined oral contraceptives and beta-blockers. These should be replaced with alternatives if possible.
Professor David Haslam is a GP in Watton-at-Stone and bariatric physician at Luton University Hospital.
References
[1] World Health Organization. Obesity and Overweight. Geneva:WHO 2014.
[2] National Audit Office. Tackling Obesity in Britain. London: NAO 2001.
[3] Health and social care Information Centre. Statistics on Obesity, Physical Activity and Diet — England, 2015. Available at: http://www.hscic.gov.uk/catalogue/PUB16988.
[4] National Obesity Observatory/Public Health England. Available at: http://www.noo.org.uk/NOO_about_obesity/mortality.
[5] McKinsey Global Institute. How the World Can Fight Obesity. Available at: http://www.mckinsey.com/insights/economic_studies/how_the_world_could_better_fight_obesity.
[6] Colditz GA, Willett WC, Rotnitzky A, et al. Weight gain as a risk factor for clinical diabetes mellitus in women. Ann Intern Med 1995;122:481–486.
[7] Chan JM, Stampfer MJ, Rimm EB et al. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care 1994;17:961–969.
[8] Yusuf S, Hawken S, Ôunpuu S et al. Effect of potentially modiï¬able risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. The Lancet 2004;364:937–952.
[9] Nanchahal K, Morris JN, Sullivan LM et al. Coronary heart disease risk in men and the epidemic of overweight and obesity. Int J Obes 2005;29:317–323.
[10] Benedetto C, Salvagno F, Canuto EM et al. Obesity and female malignancies. Best Pract Res Clin Obstet Gynaecol 2015;29(4):528–540.
[11] Vucenik I & Stains JP. Obesity and cancer risk: evidence, mechanisms, and recommendations. Ivana Vucenik and Ann New York Acad Sci. 2012;1271:37–43.
[12] Yanovski SZ & Yanovski JA. Long-term drug treatment for obesity: a systematic and clinical review. JAMA 2014;311:74–86.
[13] Sjöström L, Rissanen A, Andersen T et al. Randomised placebo-controlled trial of orlistat for weight loss and prevention of weight regain in obese patients. European Multicentre Orlistat Study Group. The Lancet 1998;352:167–172.
[14] Torgerson JS, Hauptman J, Boldrin MN et al. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes Care 2004;27:155–161.
[15] Davidson MH, Hauptman J, DiGirolamo M et al. Weight control and risk factor reduction in obese subjects treated for 2 years with orlistat: a randomized controlled trial. JAMA 1999;281(3):235–242.
[16] National Institute for Health and Care Excellence. Obesity. London: NICE 2010.
[17] Van Gaal LF, Rissanen AM, Scheen AJ et al. Effects of the cannabinoid-1 receptor blocker rimonabant on weight reduction and cardiovascular risk factors in overweight patients: 1-year experience from the RIO-Europe study. The Lancet 2005;365(9468):1389–1397.
[18] Rosenstock J, Hollander P, Chevalier S et al. SERENADE: the Study Evaluating Rimonabant Efficacy in Drug-naive Diabetic Patients: effects of monotherapy with rimonabant, the first selective CB1 receptor antagonist, on glycemic control, body weight, and lipid profile in drug-naive type 2 diabetes. Diabetes Care 2008;31(11):2169–2176.
[19] Thomas KH, Martin RM, Potokar J et al. Reporting of drug induced depression and fatal and non-fatal suicidal behaviour in the UK from 1998 to 2011. BMC Pharmacol Toxicol 2014;15:54.
[20] Cheung BM, Cheung TT & Samaranayake NR. Safety of antiobesity drugs. Ther Adv Drug Saf 2013;4:171–181.
[21] James WP, Caterson ID, Coutinho W et al. Effect of sibutramine on cardiovascular outcomes in overweight and obese subjects. N Engl J Med 2010;363(10):905–917.
[22] Caterson ID, Finer N, Coutinho W et al. Maintained intentional weight loss reduces cardiovascular outcomes: results from the Sibutramine Cardiovascular OUTcomes (SCOUT) trial. Diabetes Obes Metab 2012;14(6):523–530.
[23] Niswender K, Pi-Sunyer X, Buse J et al. Weight change with liraglutide and comparator therapies: an analysis of seven phase 3 trials from the liraglutide diabetes development programme. Diabetes Obes Metab 2013;15(1):42–54.
[24] Wadden TA, Hollander P, Klein S et al. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet-induced weight loss: the SCALE Maintenance randomized study. Int J Obes (Lond) 2013.
[25] Chan EW, He Y, Chui CS et al. Efficacy and safety of lorcaserin in obese adults: a meta-analysis of 1-year randomized controlled trials (RCTs) and narrative review on short-term RCTs. Obes Rev 2013;14(5):383–392.
[26] Li Z, Maglione M, Tu W et al. Meta-analysis: pharmacologic treatment of obesity. Ann Intern Med 2005;142:532–546.
[27] Kang JG, Park CY, Kang JH et al. Randomized controlled trial to investigate the effects of a newly developed formulation of phentermine diffuse-controlled release for obesity. Diabetes Obes Metab 2010;12:876–882.
[28] Allison DB, Gadde KM, Garvey WT et al. Controlled-release phentermine/topiramate in severely obese adults: a randomized controlled tria l (EQUIP). Obesity 2012;20(2):330–342.
[29] Garvey WT, Ryan DH, Look M et al. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): a randomized, placebo-controlled, phase 3 extension study. Am J Clin Nutr 2012;95:297–308.
[30] Gadde KM, Allison DB, Ryan DH et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): a randomized, placebo-controlled, phase 3 trial. The Lancet 2011;377:1341–1352.
[31] Wadden TA, Foreyt JP, Foster GD et al. Weight loss with naltrexone SR/bupropion SR combination therapy as an adjunct to behavior modification: the C OR-BMOD trial. Obesity (Silver Spring) 2011;19(1):935–943.
[32] Wilding J. Managing patients with type 2 diabetes and obesity. Practitioner 2015;259(1778):25–8,3.


