This content was published in 2003. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
It is well recognised that the pharmaceutical care needs of elderly patients are different from other patient populations. For example, the elderly tend to take more medicines — the recently published National Service Framework (NSF) for Older People highlights that four in five people over 75 are prescribed one or more medicines, with 36 per cent taking four or more medicines[1].
Multiple diseases and complicated treatment regimens are also common among the elderly. These factors affect the patients’ ability to manage their own medicines, resulting in adverse reactions to drugs, non-compliance and drug wastage. Medicines management, a frequently used term in recent months, is therefore important[2].
With these issues in mind, the pharmacists at Brighton General Hospital have developed, and continue to deliver, a model of pharmaceutical care designed to:
- Reduce polypharmacy;
- Ensure appropriate treatment;
- Help elderly patients understand their medicines.
Overview of changes
Before the current clinical service to the elderly was provided at Brighton, a traditional ward service was in place.
Pharmacists at all levels were ward based and carried out daily ward visits and, if time permitted, attended consultant ward rounds. They did not participate in post-take ward rounds.
Under this system, pharmacists were infrequently involved in multidisciplinary patient-focused activity. Also, pharmacist’s skills and time was not particularly well used. While senior pharmacists were able to intervene on the consultant ward rounds that they attended and, for example, discuss polypharmacy issues, junior pharmacists were less confident in doing so. Instead, junior pharmacists were more likely to liaise with nurses and junior doctors during ward visits.
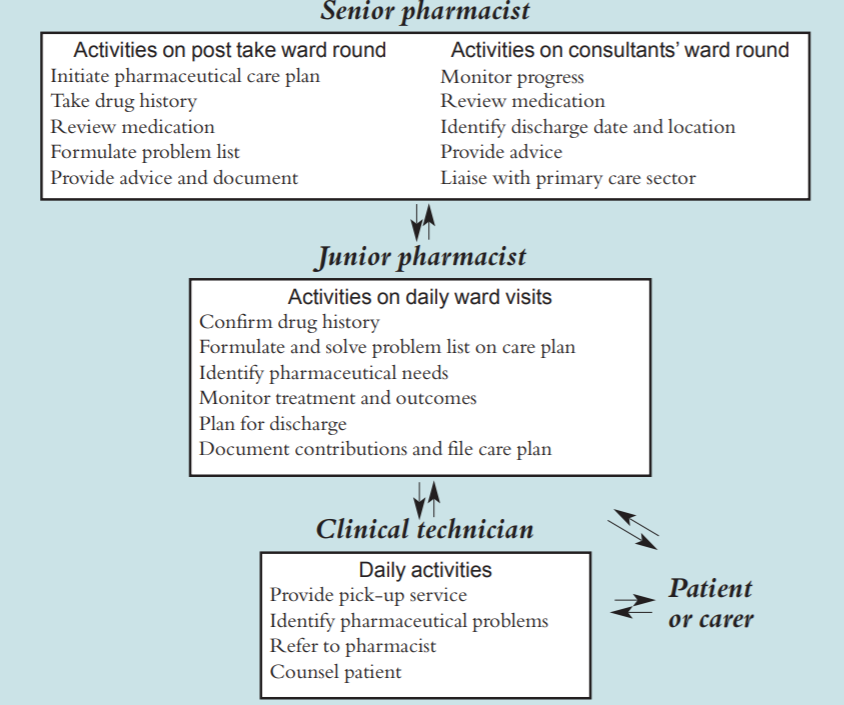
The service was remodelled within the limited resources available, building upon the skills of senior and junior pharmacists. The new service is consultant based. Senior pharmacists routinely participate in consultant ward rounds. They also participate on “post-take” ward rounds for their team. Junior pharmacists now carry out the daily ward visits, feeding back information to senior pharmacists, and receiving support and advice from their senior colleagues (see figure 1 for overview).
Role of senior pharmacists
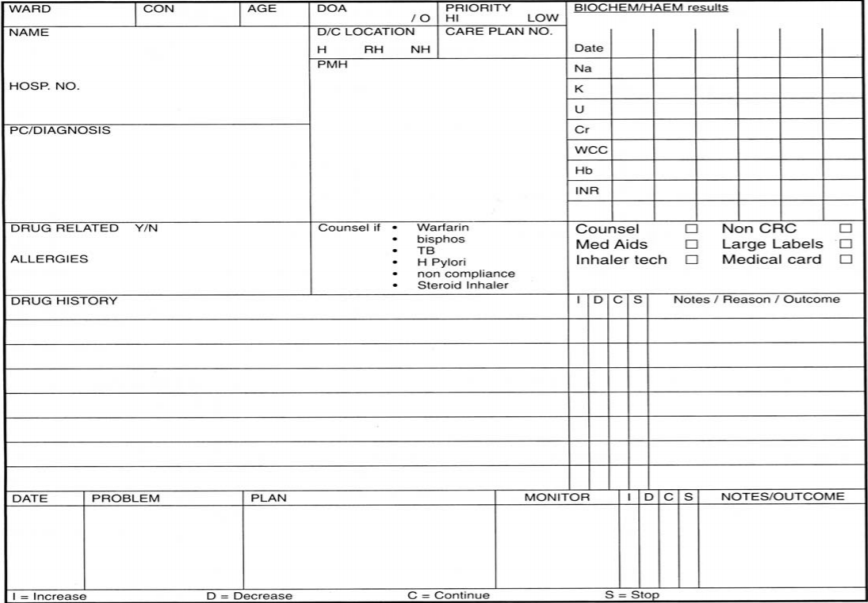
Each senior pharmacist is attached to a consultant team and regularly participates on that team’s ward rounds. While on the ward round, they gather information on investigations, treatment plans and patient progress, which they write on the pharmaceutical care plan (see figure 2). They also obtain discharge details, such as where the patient may be discharged to and when, in order to plan the service.
Newly admitted patients are also seen by senior pharmacists on post-take ward rounds such that each patient is reviewed within 24 hours (except weekends and bank holidays). The senior pharmacist documents the reason behind each admission on the pharmaceutical care plan, paying particular attention if admission is thought to be due to problems with medicines, such as non-compliance, toxicity or treatment failure. They also take a drug history using a number of sources, such as the patient, the patient’s family, general practitioner, nursing home or carer.
The issue of polypharmacy is also addressed by senior pharmacists during ward rounds. This is important since audits at Brighton General Hospital show that the mean number of drugs taken on discharge is 4.7 and intervention data show that up to 25 per cent of pharmacists interventions are querying the need for a drug. Senior pharmacists therefore advise on treatment decisions, and review and obtain information on medication changes at the point of prescribing.
Contributions made are documented on the pharmaceutical care plans, which are then handed over to the basic grade pharmacist who continues thecare. Guidance is given to the basic grade and priority patients and tasks identified.
Role of junior pharmacists
Two junior pharmacists service 100 beds for elderly patients daily by spending a morning or afternoon (approximately three hours) on the wards. They complete any unknown drug histories, gather further clinical information, monitor the outcomes of the treatment decisions and assess any other drug-related problems.
They review all drug charts at least twice weekly, with priority patients, such as those being discharged in the next 24 to 48 hours and those that are acutely ill, being targeted daily.
As part of the discharge process, basic grade pharmacists also assess the compliance needs of each patient. These needs may be addressed through the provision of large print labels, special tops, monitored dosage boxes and patient medication record cards. The latter are routinely given to all patients with more than four medicines who are being discharged home or to a nursing home.
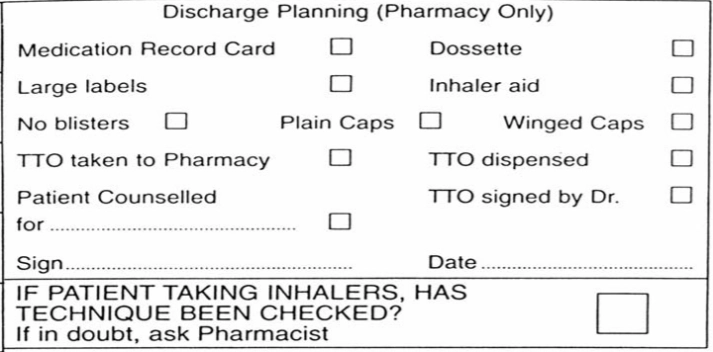
Where appropriate, junior pharmacists assess inhaler technique and make recommendations, such as providing an inhaler aid. They also counsel patients about any changes made to their medicines and advise patients on high risk therapies, such as warfarin. To help junior pharmacists assess individual needs a check list was developed and then modified[3]. The check list is now printed on the drug chart facilitating the dispensing of “to take out medicines” (see figure 3).
The junior pharmacist updates on the patient’s progress to the senior pharmacist before each consultant ward round. They also draw to the attention of the senior pharmacist any points of concern that they feel should be raised with the consultant. Each basic grade is supported by the two senior pharmacists who input into their consultant team’s patients.
Role of the technician
Technicians provide a twice daily “pickup” service to all wards with elderly patients. The technician cross checks the items ordered in the requisition book with the drug chart and then endorses the prescription as dispensed.
Where a pharmacist has checked all the items on the prescription chart for clinical issues, and has endorsed the chart appropriately, the drug is dispensed without any further check by a pharmacist, (except for a check during the dispensing process). This service allows the drug chart to remain on the ward.
A clinical technician has been appointed to aid the clinical pharmacists. They carry out some patient counselling and discharge planning, freeing up pharmacist time.
Training and appraisal
Training is provided to all pharmacists and technicians, coordinated by the clinical tutor on a weekly basis. For junior pharmacists, a mentor (a senior pharmacist) provides accompanied twice weekly visits and supports each basic grade pharmacist during their four month rotation.
Each mentor helps develop the junior pharmacist’s clinical and practical skills, building upon their knowledge and integrating them within the consultant team, so that the junior pharmacist will ultimately be competent and confident enough to attend consultant ward rounds in the senior pharmacist’s absence.
Three assessments are made during the rotation, at the beginning, middle and end to review the progress made. Brighton General Hospital is one of several pilot sites in the south east region for competency based development[4]. This has helped to develop a B to C grade strategy.
Senior pharmacists are reviewed (through observation on an accompanied visit) every six months by the clinical services manager. For technicians, training has been facilitated through the south east accreditation scheme for consultation skills and medicines management. Pharmacists have also provided training to a number of outside care agencies that administer patients’ medicines after discharge.
Benefits
A major benefit of the new system is that senior pharmacists are integrated within the consultants’ teams. This leads to better working relationships with medical and nursing staff, and raises the profile of the pharmacy department. It also means that pharmacists are able to intervene at the point of prescribing and advise prospectively rather than retrospectively. This reduces the potential for medication errors.
Recent intervention data shows that around 40 percent of interventions are made on ward rounds. Regular and focused participation on ward rounds enables senior pharmacists to pick up and record on the care plan information they might not otherwise receive. This includes information on medication changes during patient stays. Information on discharge dates and location helps pharmacists to prioritise the service.
Of particular importance is that by participating on “post-take” ward rounds, senior pharmacists are involved in the admission process.
Pharmacist participation on admission is key because recent audits at Brighton General Hospital have shown that errors primarily occur around admission. Audits have also shown that 33 per cent of all admissions and 69 per cent of all readmissions are drug related. There is also more pharmacist involvement in discharge, contributed mainly by junior pharmacists.
Patients who are counselled before discharge are less likely to be readmitted.
The responses to the satisfaction surveys that pharmacy staff send out annually show that physicians believe the participation of the senior pharmacist in their team’s ward rounds is extremely beneficial. This enthusiasm has supported the establishment of directorate pharmacists within the trust.
The reduction in the number of drug charts off the wards, and the increased availability of pharmacists, is also popular with medical and nursing staff. For the pharmacists themselves, anecdotal evidence suggests that job satisfaction is increased, helping to retain staff.
For junior pharmacists in particular, it is thought that the new system offers them guidance and support from seniors, and that their training needs are more readily identified. Technicians also value their extended role.
Care plans
A key component of the new system is the increased use of pharmaceutical care plans (see figure 2). These are used to document any important information, plan treatment goals, monitor outcomes and record interventions made. They provide a communication link between senior and junior pharmacists, facilitate discharge and help to ensure that all treatment options have been studied. The majority of elderly patients (whose average length of stay is three weeks) now have a care plan (4,000 care plans have been filed during the past three years). They are seen as crucial for priority patients.
Care plans are numbered, entered on a database and filed once the patient is discharged. On readmission these care plans can be retrieved and information can sometimes be accessed before the medical notes are available.The format of the care plan has recently been redesigned to help ensure that patient progress is documented. Training on the importance of documentation in medical notes and on care plans is given on induction to junior pharmacists.
The future
The NSF advocates forging better links with primary care providers. To this end, a new post has been created at Brighton General Hospital that involves working with the local primary care organisation. Audits to target drug-related admissions and strategies to prevent future readmission are to be put in place. Intervention data and the results of satisfaction surveys will continue to be compiled.
Using patients’ own drugs and self administration policies are also being developed across the trust. The role of the clinical technician is to continue and will probably expand to encompass drug history taking and pathology information gathering.
The role of the pharmacist is expanding too. Recently, senior pharmacists have been prescribing warfarin for in-patients under a protocol, as part of a pilot scheme to streamline care and reduce the number of errors involving anticoagulants.
Conclusion
This comprehensive model of care, from admission to discharge, addresses the needs of the elderly by using the skills of each pharmacist to ensure safe, effective, economic prescribing and use of medicines, and delivers some of the key standards set out in the NSF for Older People.
Naomi Burns is clinical pharmacy services manager at Brighton General Hospital and Elma Still was formerly principal pharmacist at Brighton General Hospital.
References
- National Service Framework for Older People. Department of Health 2001.
- Medicines management services – why are they so important? MeReC Bulletin May 2002 ;12:No 6.
- Coombes J, Horne R. A checklist for medication discharge planning. Pharm J 1994;253:161–2.4.
- Davies J.G,Webb D.G, McRobbie D, Bates I. A competency based approach to fitness for practice. Pharm J 2002;268:104–6.