This content was published in 2012. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
Objectives
Studying this article will help you gain a better understanding of:
- The indications for intravenous (IV) fluids in children
- How a child’s fluid requirements are assessed
- Which IV fluids are used for children and what factors guide fluid choice
Considerations around the management of intravenous (IV) fluids for adults have been discussed in a previous Clinical Pharmacist series (2011;3:274). Here, we describe how these considerations can differ when dealing with paediatric patients, with some specific issues relevant to this population.
Indications
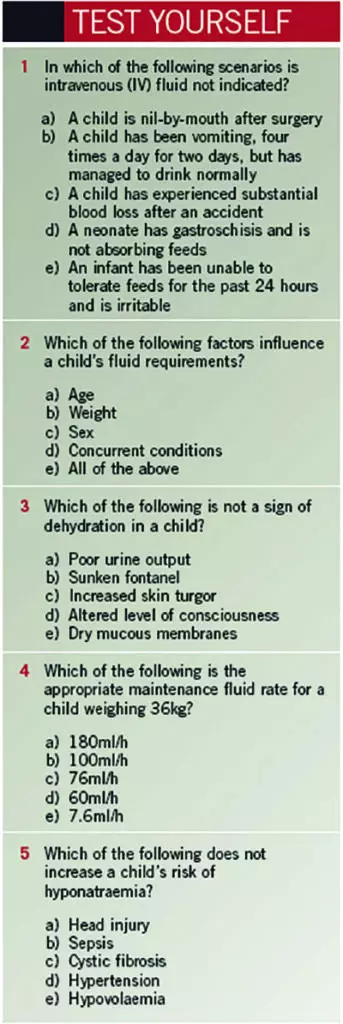
As in the adult population, rehydration for children should be provided enterally wherever possible, using oral rehydration fluids containing replacement electrolytes (eg, Dioralyte).1 IV replacement must only be used if a child cannot tolerate the volume of enteral fluid required, is nil-by-mouth or has an absorption problem.
Although most indications for IV fluid replacement are the same for children and adults (eg, excessive gastrointestinal or urinary losses, loss due to trauma or surgery or increased insensible losses for patients with burns), there are a few indications specific to paediatrics, namely:
- Increased insensible losses in jaundiced neonates undergoing phototherapy to conjugate bilirubin
- Increased insensible losses due to decreased thickness of the stratum corneum, leading to increased loss of fluid through the skin (greater risk in premature neonates)
- Decreased absorption of enteral feeds due to immature gastrointestinal function in premature neonates, or in neonates with gastrointestinal abnormalities such as gastroschisis or malrotation
Assessing fluid requirements
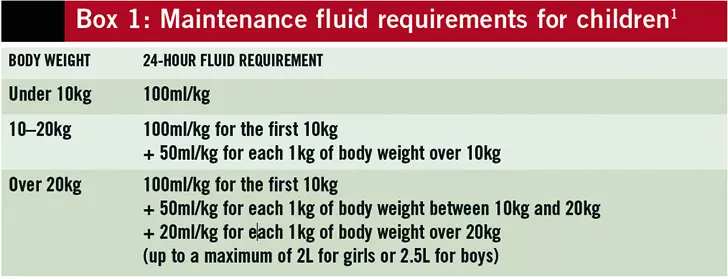
The amount of IV fluid required by a child will depend on the indication, his or her level of dehydration and any concurrent conditions. Maintenance fluid requirements are calculated based on a child’s body weight. Guidance for fluid requirements for patients over one month of age is outlined in Box 1. Neonatal fluid requirements should be calculated by a neonatologist, since both volume and glucose concentration can vary depending on a neonate’s clinical condition.
Identifying dehydration
On physical examination, signs of dehydration include:2, 3
- Thirst
- Reduced skin turgor
- Dry mucous membranes
- Altered respiratory pattern
- Increased capillary refill time
- Altered level of consciousness
- Sunken fontanel (in infants aged under two years)
- Decreased urinary frequency or volume (fewer nappy changes needed than normal)
- Irritability
A child’s degree of dehydration is estimated by assessing these clinical features. His or her fluid deficit can then be calculated — this volume will be added to normal maintenance fluids to correct the dehydration.2
Dehydration is corrected over 24 hours (unless a patient is hypovolaemic, in which case an initial fluid bolus will be given), or over 48 hours for patients with hypernatraemia (serum sodium >140mmol/L) to reduce risk of rapid fall in serum sodium levels (which should not fall by more than 1mmol/L/h).2
Fluid balance
Monitoring of fluid balance — including body weight (measured at baseline, then daily) and fluid input and output — should be undertaken for all children receiving IV fluids.2, 4 For young infants who are not yet toilet trained, nappies are often weighed to estimate the urine output.
Other losses, including nasogastric tube aspirations, ileostomy or colostomy outputs, and estimated insensible losses, are also monitored.
Care should be taken with very small infants, or for children with fluid restrictions, because medicines administered intravenously can provide a large portion of their fluid allowance. This should be taken into account when calculating required fluid volumes.
Fluid choice
Maintenance therapy
The maintenance fluid usually given to well children at low risk of developing hyponatraemia (see below), and with normal renal and cardiac function, is a ready-mixed solution of sodium chloride 0.45% plus glucose 5%.2, 4
Fluid replacement or resuscitation
Intravascular volume depletion should be managed using bolus doses of sodium chloride 0.9%. It is usually given at a rate of 10ml/kg over 30 minutes, but can be given faster if a child is exhibiting signs of shock. Colloid solutions (containing albumin, gelatin or etherified starch) can be used for fluid resuscitation of children who are in shock and who have lost blood or fluid that is high in protein (eg, from pleural or ascitic drains, or from burns).2
Hyponatraemia
Elevated levels of antidiuretic hormone can lead to impaired excretion of free water, and are associated with conditions such as pneumonia, meningitis and sepsis.2, 5 If hypotonic sodium chloride infusion (a source of free water in these cases) is given, a fall in serum sodium may occur.
Hyponatraemia is defined as a serum sodium <130mmol/L.6 Clinical signs of hyponatraemia include headaches, nausea, vomiting, irritability, seizures and apnoea.2, 4
Following the report of several deaths due to hyponatraemia caused by the use of physiologically hypotonic IV fluids, the National Patient Safety Agency in 2007 issued an alert advising that hypotonic fluids, including sodium chloride 0.18% plus glucose 4%, should be removed from paediatric surgical areas and that they should not routinely be used for fluid maintenance in any paediatric patients.2, 4
The risks of developing hyponatraemia are increased in the following conditions:2, 4, 5
- Low serum sodium (<134mmol/L)
- Hypovolaemia
- Peri- and postoperative period
- Hypotension
- Central nervous system infections
- Head injury
- Bronchiolitis
- Sepsis
- Excessive gastric or diarrhoeal losses
- Salt wasting syndromes (eg, cystic fibrosis)
Management
Isotonic fluids (sodium chloride 0.9% plus glucose 5%) should be given in established hyponatraemia. Fluid restriction can also be used — this will reduce the amount of free water and compensate for hyponatraemia.
Monitoring
Hyponatraemia can develop quickly when IV fluids are being given and, therefore, thorough monitoring is required.
In addition to fluid balance, plasma creatinine, urea, sodium and potassium should be measured before treatment starts (if possible) and daily during fluid therapy.
If abnormal results are found, the test should be repeated after four hours and any electrolyte derangements corrected. If clinical signs of hyponatraemia occur, electrolytes should be checked immediately.2, 4,
For discussion
- Are the appropriate intravenous (IV) fluids available in the paediatric areas of your hospital?
- Which factors should you include when assessing fluid requirements in a child?
- How is fluid balance measured by ward staff?
- Which groups of children admitted to your paediatric areas are at risk of hyponatraemia?
Answers
1 b; 2 e; 3 c; 4 c; 5 d
References
- Paediatric Formulary Committee. BNF for Children 2010–11. London: BMJ Group, Pharmaceutical Press and RCPCH Publications; 2010.
- Nunn AJ. Clinical guideline on the administration of intravenous fluids. Alder Hey Children’s NHS Foundation Trust guidelines. June 2009.
- Beattie TJ. Disorders of fluid and electrolyte balance. In: Webb N, Postelthwaite R, eds. Clinical Paediatric Nephrology. New York: Oxford University Press; 2003. pp29–59.
- National Patient Safety Agency. Reducing the risk of hyponatraemia when administering intravenous infusion to children. March 2007. www.nrls.npsa.nhs.uk/resources (accessed 24 March 2012).
- Davies P, Hall T, Ali T, et al. Intravenous postoperative fluid prescriptions for children: A survey of practice. BMC Surgery 2008;8:10.
- Hurdwowar A, Urmson L, Bohn D, et al. Compliance with a pediatric clinical practice guideline for intravenous fluid and electrolyte administration. Healthcare Quarterly 2009;12:129–34.