Courtesy of Dansac Ltd
This content was published in 2010. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
In our previous article (PJ, 6 November 2010, pp515–8), we described different types of stoma, problems common to people with stomas (“ostomates”) and lifestyle advice that pharmacists can reinforce. Having a stoma can be challenging — both physically and psychologically — and, typically, patients will see a stoma nurse for advice and care both before and after surgery. After surgery, the stoma nurse will usually give patients a selection of stoma bags to try (often before the patient is discharged), allowing them to choose the type that best suits their dexterity and lifestyle. The nurse will take into account factors such as the type of stoma, its position, stomal output, skin type, desired change frequency and ease of use. Once a bag is deemed acceptable, the nurse can arrange for further supplies, either through a dispensing appliance contractor (DAC) or a pharmacy.
Appliances and accessories
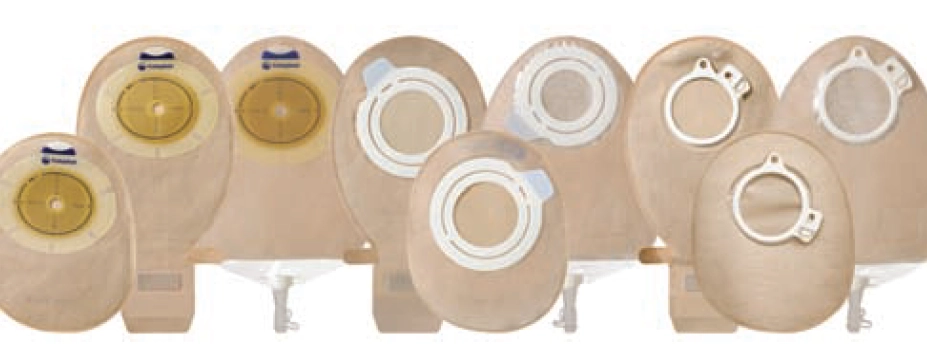
Stoma bags are designed to fit over the stoma to collect stool or urine while preventing leakage and odour. The bags, [which are usually slightly larger than an adult hand,] are attached to the skin surrounding the stoma by adhesive on the flange (also called a base plate or face plate).
Two basic types of bag — closed and drainable — are available depending on the type of stoma, which in turn affects the output. Panel 4 describes typical output for different stomas and the recommended bag type.
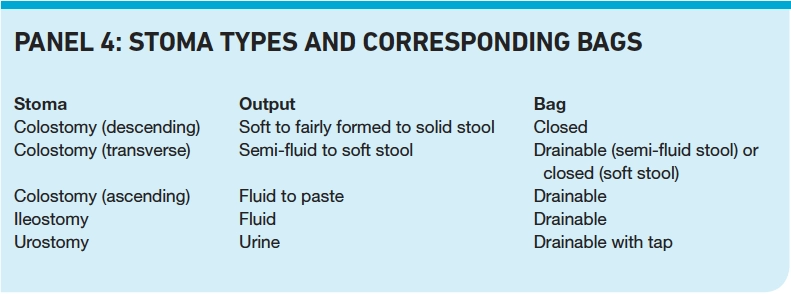
Colostomy bags can be closed or drainable. Drainable bags are more suited to output produced by ileostomates, which has high water content. They are emptied and resealed with reusable plastic clips or soft wire ties but newer bags have integrated fastenings. Urostomy bags are drainable, with a tap for emptying urine. They can be used with night drainage bags, which have a larger capacity.
Bags can also be clear or opaque. Clear bags can be useful immediately following creation of the stoma, allowing the stoma nurse and patient to monitor output. They also allow patients to see their stoma when they are changing bags and gain confidence in fitting them correctly. Some patients may prefer opaque stoma bags that have a splitfilm backing that acts as a peep hole (eg, Pelican, Salts, Coloplast).
The flange and bag can exist as an integrated unit (one-piece system) or separately (two-piece system), where the bag is attached to the flange either by a clip or adhesive. This means the bag can then be changed without removing the flange and two-piece systems may be preferred by patients who experience pain or skin irritation from frequent bag changes.
Most bags are flat and are suitable for most ostomates. Convex-shaped bags are available for those whose stomas are retracted (ie, below the skin surface). They press on the skin tissue around the stoma, causing it to protrude more, and support the peristomal tissues to form a more normal shape, improving the seal and preventing leakage under the flange.
Some ostomates prefer to manage their stoma output using irrigation. This is only suitable for those with an end colostomy and involves clearing the colon of stool with water introduced through the stoma using an irrigation set. This allows control over the stoma output and dispenses with the need for a pouch. Instead, patients can wear a stoma cap (available on prescription) or dressing during the day giving them more control over their activities. However, ostomates should only consider irrigation after an informed discussion with their stoma care nurse and the surgeon because damage can be caused by using incorrect methods.
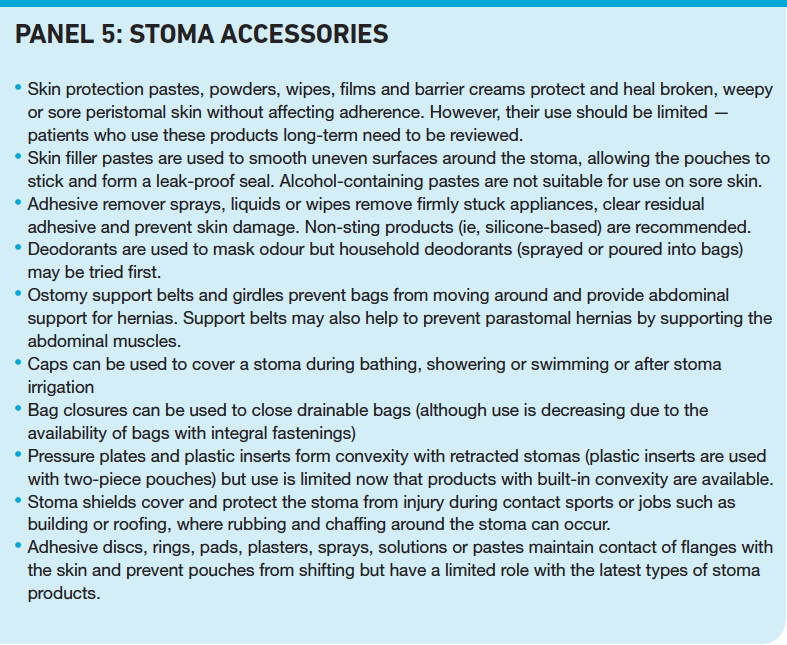
In addition to bags, ostomates can require a variety of accessories to help them manage their stoma. Examples are given in Panel 5.
Reflect
- Why might a patient choose to wear a clear stoma bag?
- How often should stoma bags be changed?
- What appliances might ostomates require and why?
Before reading on, think about how this article may help you to do your job better.
Skin care
Between each change of one-piece system, patients should ensure that they clean the skin and stoma thoroughly to remove any adhesive residue or faecal matter. They can use warm water with soft wipes or kitchen towel. “Baby wipes” are generally not suitable for routine use because they can contain irritants. Soap is not usually necessary. Patients should wipe the skin dry with a fresh wipe before changing the system or applying any skin protective, barrier creams or fillers where these are needed.
If body hair needs to be removed from around the stoma, this should be done after cleaning and before applying any products. Scissors or an electric shaver can be used but hair remover creams and razor blades should be avoided because they can irritate the skin.
Disposal of used bags
The contents of pouches can be emptied into a toilet and, if possible, the bags should be rinsed out with water. Closed bags can be cut at the bottom to release the contents. Drainable bags are emptied by opening the closure or tap at the bottom of the bag. The bag, along with any wipes used during a bag change, can be wrapped tightly in a plastic bag and disposed of in normal household waste. Some colostomy bags are now available with an inner pouch that can be flushed down the toilet (eg, Freestyle vie, NovaLife 2).
Prescribing and dispensing
Stoma appliances and accessories that are prescribable on the NHS are listed in Part IXC of the Drug Tariff for England and Wales and Part 6 of the Drug Tariff for Scotland. Prescriptions should accurately describe the brand and size of the pouches to be supplied to the patient. Patients with permanent stomas are exempt from prescription charges (patients in England need to obtain a prescription charge exemption certificate, FP92A [EC92A in Scotland]), but those with temporary stomas are not.
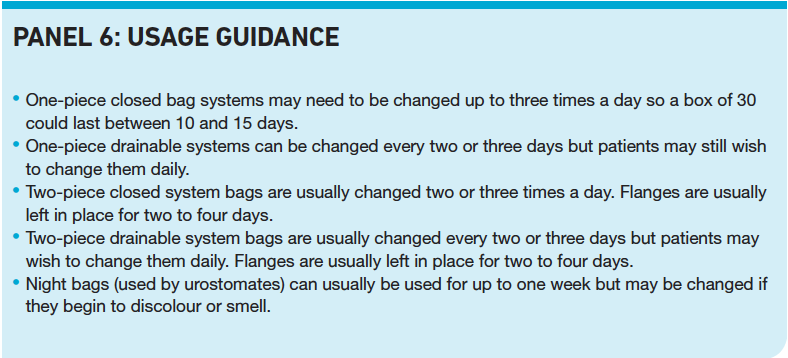
Pharmacists should advise patients to order their supplies one to two weeks before they are due to run out to allow time for delivery. Repeat dispensing can help ensure an uninterrupted supply and help the pharmacist to spot changes in patterns of use and intervene to ensure quantities supplied are sufficient to meet the patients’ needs. For most patients one or two months’ supply on a single prescription will be sufficient to meet normal requirements. It is ultimately for patients to decide how often they change their bags but Panel 6 gives an idea of how often different bags are changed and, therefore, the sorts of quantities that would be needed.
Stoma products have a limited shelf life because plastic items and skin care products can deteriorate at high temperatures so patients should be advised to avoid stock piling and to store their appliances in a cool, dry place. Patients should be made aware that they can obtain emergency supplies. This may be arranged through DACs if the pharmacy does not hold stock.
Supply standards
From 1 April 2010 supply arrangements for stoma appliances in England and Wales changed and, by 31 December 2010, pharmacies (and DACs) wishing to dispense these appliances must be compliant with the new essential service standards, which include:
- The pharmacy must offer a home delivery service
- The pharmacy must supply wipes and stoma disposal bags if required
- The pharmacy must be able to provide expert clinical advice, as well as advice on use, storage and disposal of appliances, and keep records of advice given
More detailed information (eg, when appliances are delivered the packaging must not indicate the contents) and a checklist for compliance are available on the Pharmaceutical Services Negotiating Committee and Community Pharmacy Wales websites. Contractors who do not wish to dispense stoma appliances or cannot make a supply must have arrangements in place for referral (with patient consent) or signposting to another supplier. Inducements for referral are not permitted.
In Scotland, finalised arrangements for the supply of stoma appliances in the community have been in place since 2006. The minimum standards are similar to requirements in England and Wales (eg, home delivery must be offered and disposal bags and wipes provided with each supply of qualifying items) but are under further consultation.
No specific guidance is given on the training required to give advice to ostomates in England and Wales. However, the Scottish sevice standards document3 gives an idea of what a suitable training programme should include. For example, it recommends that pharmacy staff should understand “pancaking” (PJ, 6 November 2010, p517) and be familiar with ways of reducing it.
Advanced services
In England and Wales, contractors may also provide two advanced services to ostomates: customisation and appliance use reviews. In Scotland, provision of customisation is a minimum standard for supply.
Customisation
After surgery the size and shape of the stoma can change, [especially in the first six to eight weeks], so the size of the opening on the flange will need to be adjusted. For stomas with a regular shape, stoma bags with a precut flange opening in the correct size can be ordered. For irregularly shaped stomas or those that are still changing in size, bags are available with a cut-to-fit opening, which can be customised to the correct shape and size, using a template of the stoma. Templates are usually made by the stoma nurse or patient by producing an outline of the stoma on a card.
Patients can customise the opening themselves (with scissors) but some, especially those with reduced dexterity or with irregularly shaped stomas, might request a DAC or their pharmacist to do this. Customisation involves cutting a hole in the base plate to the exact size and shape of the stoma and can be done with scissors or cutting devices (eg, lasers). Customisation includes assembling two-piece appliances (ie, clipping a bag to the base plate) and applying additional items (eg, soft-tie closures).
In England and Wales a fee of £4.32 is paid for every qualifying prescription item dispensed. To provide this advanced service, contractors must satisfy certain conditions. For example, they must notify the NHS Business Service Authority and the primary care organisation using the correct forms. Further details, forms and templates are available on the PSNC and CPW websites.
Pharmacists should be aware that mouldable skin barriers, which eliminate the need for cutting, are available. These modified adhesives fit snugly around the stoma regardless of size and shape. They are currently only available in two-piece systems.
Contractors who cannot provide customisation are required to refer the prescription (with the patient’s consent) to another supplier or to provide the patient with the details of two other suppliers who may be able to provide the service.
Appliance use reviews
Appliance use reviews (AURs) can be performed in the pharmacy or in a patient’s home by a pharmacist or a nurse. The aim is to improve the patient’s use and knowledge of the appliance, so an AUR would include advice on storage and disposal. Patients who might be suitable for an AUR (or referral if AURs are not provided) include those who:
- Routinely over-order stoma supplies
- Have been using skin protective pastes, powders, wipes, films and barrier creams long-term
- Currently use pressure plates or shields; they may benefit from the use of the newer products with built in convexity
- Are using adhesive discs, rings, pads or plasters; newer products may be more appropriate
- Are using products that are about to be discontinued
- Are anxious or are experiencing significant psychological difficulties; they should be referred to their stoma nurse or GP
Contractors are paid £28 for AURs conducted in pharmacies and £54 for those in patients’ homes. There is a limit of one AUR per 35 qualifying prescriptions. Details of conditions that must be satisfied before AURs can be conducted are available on the PSNC website. One condition is that the contractor must send the PCO evidence of qualifications and details of competency with respect to the use of stoma appliances. However, the Department of Health has not specified what qualifications are acceptable and it may be up to individual PCOs to decide.
DECLARATION OF INTEREST
Jo Sica is employed by Hollister Ltd and works in the NHS as a clinical nurse specialist, stoma care.
References
- Herlufsen P, Olsen AG, Carlsen B, Nybaek H, Karlsmark T, Laursen TN et al. Study of peristomal skin disorders in patients with permanent stomas. British Journal of Nursing 2006;15:854–62.
- United Ostomy Association. Diet and nutrition guide. Available at www.ostomy.org (accessed on 2 November 2010). 3 NHS Scotland. Service standards relating to provision of stoma care appliances to patients in the community. Available at www.sehd.scot. nhs.uk (accessed on 28 October 2010).
Resources
- Useful patient information sheets, “eating with a colostomy” and “eating with an ileostomy”, have been produced by Addenbrookes Hospital and are available at www.cuh.org.uk.
- Information on the role of stoma nurses can be found on the World Council of Enterostomal Therapists UK website (www.wcetuk.org.uk).
Further reading
- Porrett T, Daniel N. Essential coloproctology for nurses. London: Whurr Publishers Ltd; 1999.
- Lyon C, Smith AJ. Abdominal stomas and their skin disorders. 2nd Ed. London: Martin Dunitz Ltd; 2010.
- Burch J. Stoma care. London: Wiley Blackwell; 2008.
- Black P. Holistic stoma Care. London: Balliere Tindall; 2000.
Practice points
Reading is only one way to undertake CPD and the regulator will expect to see various approaches in a pharmacist’s CPD portfolio.
- Perform a strengths-weaknesses opportunities-threats analysis. Does is make sense for you to provide stoma services?
- Ensure your SOPs reflect the new stoma service requirements and that staff are suitably trained where appropriate. If you do not provide services, who will you signpost or refer patients to?
- Find out who your local stoma nurses are.
Consider making this activity one of your nine CPD entries this year.
CPD articles are commissioned by The Pharmaceutical Journal and are not peer reviewed.