
Hollister
This content was published in 2010. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
The word “stoma” originates from Greek, and means an opening into or out of the body. A stoma is surgically created when part of the bowel or bladder is pulled from the abdominal cavity through the abdominal wall and attached to the skin of the abdomen. The bowel or bladder contents can then be eliminated through the stoma into a removable bag (sometimes called a pouch), which is attached to the body via an adhesive flange (sometimes also called a base plate or face plate).
There are many reasons for stoma formation. Faecal stomas (colostomy and ileostomy) generally need to be made because of cancer, diverticular disease, Crohn’s disease, ulcerative colitis or as a result of an accident. Urinary stomas (urostomy or ileal conduit) are usually created because of cancer or neurogenic bladder (eg, in spina bifida).
When a colostomy is performed part of the colon is removed (resected) or bypassed. The position of the resulting stoma will depend on whether it is created from the ascending, transverse or descending part of the colon. For example, in a descending colostomy (the most common type of colostomy), the stoma is usually on the left hand side of the abdomen compared with the rarer ascending colostomy, where the stoma will be on the right hand side. Colostomies can also be described in terms of the type of surgery that has been performed. Loop colostomies are when the stoma is made from a loop in the bowel. End colostomies are when the end of the bowel (ie, what remains after part of the bowel has been removed) is used to make the stoma.
In the case of an ileostomy, all of the colon, rectum and anus are resected or bypassed. An end ileostomy is created from the distal end of the ileum and will, therefore, be sited on the lower right hand side of the abdomen. In contrast, a loop ileostomy can be situated anywhere along the ileum to bypass the part of the bowel that is causing problems.
Stomas can be permanent (eg, if the end portion of the colon or rectum is diseased and requires removal) or temporary (eg, a stoma might be created to bypass the bowel to rest it in irritable bowel disease or injury). A temporary stoma can be reversed six to 12 weeks after the initial procedure or later,depending on the healing process.
Creation of a urostomy usually involves removal of the bladder or, rarely, bypassing it.The ureters are grafted onto a section of the ileum (approximately 12cm long), which is then used to form a stoma through which urine can drain (ileal conduit). A urostomy is commonly located on the right hand side of the lower abdomen.
Stomas usually look bright red due to a rich supply of blood vessels and can bleed when rubbed. They have no nerve endings, so there should be no pain when handling them.There will be individual differences in the shape and size of a stoma depending on the type of surgery performed and body shape.For example, some will protrude more than others.
It has been estimated that over 100,000people in the UK have a stoma.1
Living with a stoma
Once patients have recovered from surgery, they can resume most normal activities. The doctor or stoma care nurse will provide advice on specific matters but pharmacists can help to reinforce lifestyle advice and to ensure appropriate use, storage and disposal of stoma appliances. Stoma bags and related items will be discussed in further detail in the second part of this article, to be published online on 19 November 2010.
Diet
People with a stoma (“ostomates”) often require dietary advice because bowel function will be affected by surgery. Immediately after a colostomy or ileostomy, the stool tends to be watery and more frequent than before, mainly because the shortening of the bowel results in less water reabsorption. Patients should, therefore, be advised to drink plenty of fluids to avoid dehydration.
The stool will start to firm up as the patient begins to eat solid food and, eventually, most patients will be able to resume a normal diet, which should be balanced, with meals at regular intervals. New foods should be gradually introduced (one at a time) in small portions. As their eating habits develop into a routine patients may be able to adjust their eating and diet to control their stoma output to suit their activities.
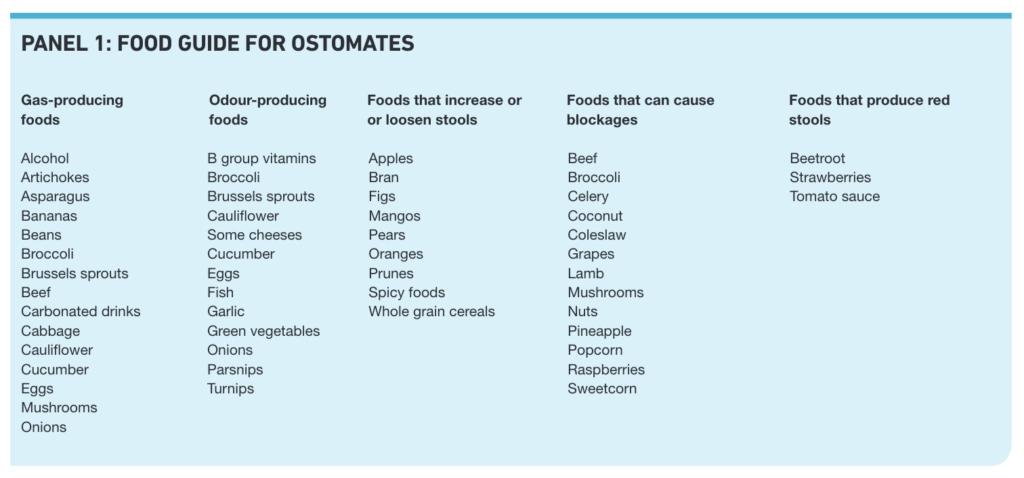
Certain foods can cause problems such as gas, odour, blockage, constipation or diarrhoea in some patients and Panel 1 lists some common examples. Not everyone will be affected in the same way, so patients will need to experiment and learn to manage their diet, avoiding some foods to minimise problems. Patients may also be made aware of foods that produce red stools so that they do not worry that their stoma or bowel may be bleeding.
Some foods can be helpful. Foods that can help dispel gas include peppermint tea, peppermint oil in hot water and fennel. Foods that can help reduce odour include parsley, cranberry juice, yoghurt and buttermilk.
All patients, whatever their stoma type, should drink plenty of fluids and eat fibre-rich food to avoid constipation. (Fibre should be increased slowly, starting with small amounts for the first couple of months, then slowly increasing foods high in fibre, such as vegetables, fruits, whole cereals and wholemeal rice and pasta.)
Food in the ileum might not be fully broken down so people with an ileostomy (“ileostomates”) should eat small mouthfuls and ensure that these are well chewed in order to avoid blockages. They should also take special care with or avoid foods that could cause blockages (see Panel 1). Ileostomates are encouraged to add salt to their food to make up for losses via their stoma.
“Urostomates” (people with a urostomy) need to drink about three litres of fluid a day, including drinks high in vitamin C (eg, cranberry juice) to acidify the urine and reduce mineral deposits. Cranberry juice and vitamin C are believed to help reduce mucous secretions which, in combination with urine, break down the flange, causing leaks and, therefore, skin problems (eg, maceration).
Clothes
Stoma bags are designed to fit discreetly under clothing and they can be worn underneath normal swimming costumes.However, special swimming costumes that disguise the presence of a prominent stoma can be purchased. Patient support organisations (see Signposting) can provide information on where these can be purchased.
Sex life
Most ostomates will be able to resume a normal sex life once they have recovered from surgery, but they may find some sexual positions uncomfortable. For comfort and peace of mind, a smaller bag or stoma cap can be used during sexual activity.
Sexual function in women is not normally affected although some may experience vaginal dryness, which a vaginal lubricant may help. Some men suffer impotence that eventually resolves but bladder removal or nerve damage can lead to permanent impotence. Nerve damage can also cause loss of sensitivity in both men and women.
Sexual problems are more likely to be related to removal of the rectum rather than the stoma itself. Wounds in this area heal slowly. In addition, nerves involved in sexual function are located around the rectum and may, rarely, be damaged during surgery. Patients who are concerned should speak to their stoma care nurse or GP.
Sports
Ostomates can participate in most sporting activities. However, contact sports may pose a risk of injury to the stoma and weight lifting can strain the muscles surrounding the stoma causing a hernia. Ostomates wishing to participate in such activities should first consult their GP or stoma nurse.
Ostomates can swim (and shower or bathe) with or without a bag in place, or they can replace the bag with a plug or a cap. Colostomy and ileostomy bags have a filter (usually charcoal based) to allow gas to escape while absorbing and eliminating odours.Although some bags with protected filters (eg, Hollister AF300) are available, many air filters will need to be covered with a waterproof plaster to prevent water entering.
Travel
Some forward planning and preparation can help prevent problems during travel.
Ostomates going abroad should take supplies to last for the whole visit. This may mean that they need to order extra appliances and accessories. It might be advisable to pack these in hand luggage to avoid a situation where hold luggage goes missing and the patient is left with no immediate supplies.
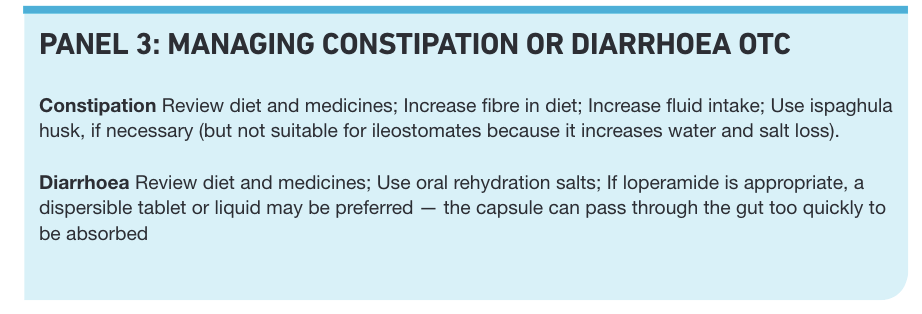
Ostomates should also carry medicines for diarrhoea, including oral rehydration salts, and, particularly if they are travelling by aeroplane, they should get a letter from their GP stating that they need to carry stoma supplies and medicines in their hand luggage.
As will be discussed in our second article, some patients will need to customise their flanges to fit their stoma. Ostomates who travel by aeroplane should pre-cut their flanges, because scissors are no longer allowed in hand luggage.
Ostomates should also be aware that their bag can show up on full body scanners. They can obtain travel certificates that explain what an ostomy bag is from any ostomy patient association or dispensing appliance contractor.
During air travel, gases within the bowel will expand because of the reduced air pressure and this can cause the bag to balloon. Fizzy drinks can aggravate the problem so should be avoided before and during the flight.
Medicines use
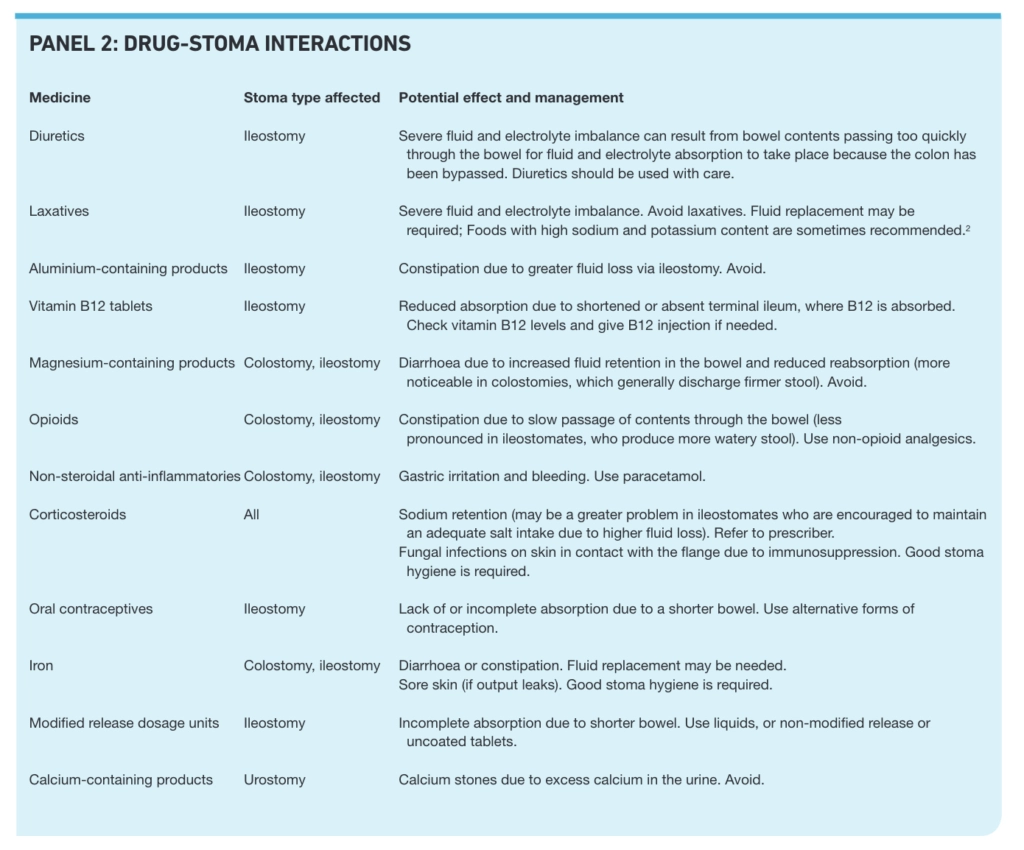
Some medicines can affect the functioning of the stoma and vice versa. Some effects will depend on stoma type. Examples are given in Panel 2.
Pharmacists need to be aware of potential problems so they can advise ostomates appropriately both on prescription medicines or management of minor ailments. For example, most ostomates with pain, should use simple analgesics, such as paracetamol. If non-steroidal anti-inflammatory drugs are used, usual precautions, such as taking with or after food, apply. Opioid analgesics should be will also help to prevent crystals forming.Crystal formation can be treated with half water and half white vinegar wipes, held against the skin for a few minutes between bag changes.
Skin problems
In spite of good stoma hygiene, a variety of skin problems can develop. These include soreness, ulcers, bruising, dermatitis, psoriasis, eczema, granulomas and pressure sores on the peristomal area. Patients experiencing these problems will need review and referral to their stoma nurse or GP. Skin problems will generally be treated with the usual remedies, but the ostomate should always be referred for assessment to determine the cause.
Signposting
- Patient organisations and support groups include The Colostomy Association.(www.colostomyassociation.org.uk), The Ileostomy and Internal Pouch Support Group (www.the-ia.org.uk), the Urostomy Association (www.urostomy association.org.uk) and Ostomyland (http://ostomyland.com).
- Ostomy Lifestyle (www.ostomylifestyle.org) is a source of independent advice for both patients and healthcare professionals.


