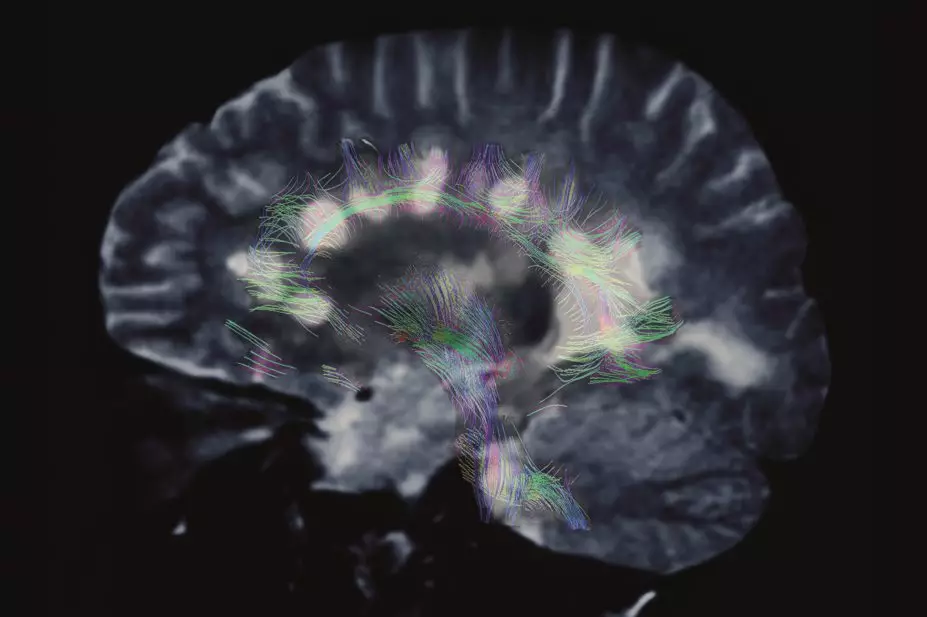
Zephyr / Science Photo Library
Tizanidine is an alpha2-adrenoceptor agonist that is structurally related to clonidine. It acts on the central nervous system, mainly in the spine and brain, to inhibit excitatory interneurons and relax skeletal muscle. Tizanidine is used for the symptomatic relief of spasticity associated with multiple sclerosis or with spinal cord injury or disease, and it is also used in the symptomatic treatment of painful muscle spasm associated with musculoskeletal conditions.
Pharmacodynamic interactions
The most common adverse effects of tizanidine are drowsiness and fatigue, which can be greater when tizanidine is taken with other sedatives. Patients should be warned that concurrent use of tizanidine with alcohol or other medicines that can cause sedation may cause drowsiness, and they should avoid driving and other skilled tasks if they are affected.
Alcohol also increases the patient’s exposure to tizanidine, as measured by the area under the concentration–time curve (AUC), which has been reported to be increased by about 20%. This could further increase the risk of adverse effects[1]
.
Tizanidine can cause dose-related hypotension, which can result in bradycardia, dizziness, light-headedness, and, rarely, syncope. These effects can be minimised by careful titration of the dose (tizanidine is initially started at 2 mg once a day and increased according to response by 2 mg every three to four days, usually to 24 mg a day in three to four divided doses, up to a maximum of 36 mg a day).
The risk of effects related to hypotension is greater in patients taking other medicines that lower blood pressure. Patients who take tizanidine with antihypertensive medicines should be warned to lie down if symptoms such as dizziness or light-headedness develop, and to remain lying down until they end. Tizanidine can cause bradycardia, and this risk may be increased in patients taking digoxin. Patients taking both medicines should be monitored regularly for bradycardia. This is likely to be every two weeks when treatment is started, but otherwise the frequency of monitoring is based on individual factors including the patient’s age, comorbidities and other medicines.
The risk of long QT syndrome associated with tizanidine is unclear. Small in vivo studies have suggested that no increase in the QT interval occurs; however, the UK manufacturer states that prolonged QT interval has been reported in cases of tizanidine overdose, and chronic toxicity studies in dogs have resulted in QT prolongation. The risk of a prolonged QT interval with tizanidine might be increased when taken with medicines that increase its exposure (see below), as well as general risk factors such as older age, female sex and the presence of cardiac disease or metabolic disturbances (such as hypokalaemia).
Patients taking tizanidine and a medicine associated with a high risk of prolonged QT interval (such as quinidine, sotalol or dronedarone) should be monitored regularly using an electrocardiogram (ECG).
Pharmacokinetic interactions
Tizanidine is metabolised substantially by the cytochrome P450 isoenzyme CYP1A2. Any drug that inhibits CYP1A2 is likely to cause an increase in the exposure to tizanidine and may therefore increase its adverse effects.
Fluvoxamine, a selective serotonin re-uptake inhibitor (SSRI), is contraindicated in patients taking tizanidine. This is because fluvoxamine is a potent CYP1A2 inhibitor and has been shown to increase exposure to tizanidine 33-fold if used concurrently[2]
. Broadly speaking, this means that a 2 mg dose of tizanidine effectively becomes a 66 mg dose when used concomitantly — far higher than the recommended dose. Other SSRIs are not considered to inhibit CYP1A2 and are therefore suitable alternatives.
Ciprofloxacin is contraindicated in patients taking tizanidine[1]
[3]
. It is a moderate CYP1A2 inhibitor and has been shown to cause a 10-fold increase in tizanidine exposure, and a consequent increase in sedation and hypotension and bradycardia, particularly when starting treatment[4]
. If ciprofloxacin is the most appropriate antibacterial to use in a patient already taking tizanidine, the dose of tizanidine should be reduced before starting ciprofloxacin, and the patient should be monitored closely for adverse effects.
Other quinolones can also inhibit CYP1A2 to varying degrees, and patients taking tizanidine should be monitored closely for side effects if these medicines are used concomitantly.
Combined hormonal contraceptives are moderate inhibitors of CYP1A2. In a study of 15 women taking an oral combined hormonal contraceptive (gestodene with ethinylestradiol 20 mcg or 30 mcg), the AUC from a single 4 mg dose of tizanidine was 3.9-fold higher than in 15 women not taking a hormonal contraceptive[1]
[3]
. The UK manufacturer of tizanidine predicts that adverse effects might occur even when lower doses of tizanidine are used. Therefore the dose of tizanidine should be reduced before a patient starts taking a combined hormonal contraceptive, and the patient should be monitored for adverse effects[1]
[3]
.
This article has been produced by Stephanie Jones, Harpreet Sandhu and Claire L. Preston on behalf of the Stockley’s Drug Interactions editorial team. The book is available in print through Pharmaceutical Press or electronically with quarterly updates through www.medicinescomplete.com.
References
[1] Zanaflex (Tizanidine hydrochloride). Acorda Therapeutics, Inc. US Prescribing information, November 2013.
[2] Granfors MT, Backman JT, Neuvonen M et al. Fluvoxamine drastically increases concentrations and effects of tizanidine: a potentially hazardous interaction. Clin. Pharmacol. Ther. 2004; 75(4):331–341.
[3] Zanaflex (Tizanidine hydrochloride). Cephalon Ltd. UK Summary of product characteristics, June 2014.
[4] Granfors MT, Backman JT, Neuvonen M et al. Ciprofloxacin greatly increases concentrations and hypotensive effect of tizanidine by inhibiting its cytochrome P450 1A2-mediated presystemic metabolism. Clin. Pharmacol. Ther. 2004; 76(6):598–606.


