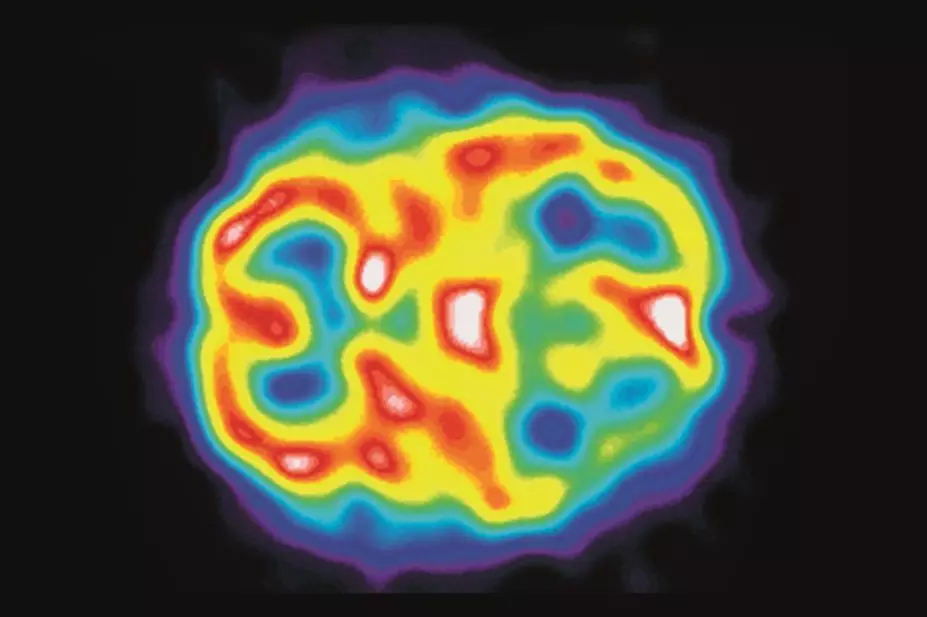
Department of Nuclear Medicine, Charing Cross Hospital / Science Photo Library
Summary
Commonly known as the triptans, 5HT1 receptor agonists are used to treat acute migraine attacks and include almotriptan, eletriptan, frovatriptan, naratriptan, sumatriptan and zolmitriptan. Despite their widespread use, cl
inically relevant interactions with
5HT
1 receptor agonists are not frequently encountered, but a number of interactions are known.
Naratript
an is unlikely to be involved in important pharmacokinetic interactions as half the dose is excreted unchanged and the rest is metabolised
by a variety of isoenzymes. CYP3A4 inhibition
and induction are important interactions for eletriptan and almotriptan, which are both metabolised by CYP3A4.
CYP1A2 inhibition and induction can affect zolmitriptan and frovatriptan. CYP1A2 inducers, such as tobacco smoke, are expected to decrease exposure to frovatriptan and zolmitriptan. Monomamine oxidase A inhibition can affect almotriptan, rizatriptan, sumatriptan and zolmatriptan.
5HT1 receptor agonists are generally contraindicated in patient
s taking ergot derivatives because of a theoretical risk of additive vasoconstriction. Drug interations between selective serotonin-reuptake inhibitors and 5HT
1 receptor agonists causing adverse reactions are possible, although these and interactions causing serotonin syndrome are extremely rare. Serotonin syndrome may also occur with concurrent use of monoamine oxidase A inhibitors and 5HT1
receptor antagonists.
5HT1 receptor agonists, commonly known as the triptans, are used to treat acute migraine attacks. The 5HT1 receptor agonists currently available are almotriptan, eletriptan, frovatriptan, naratriptan, sumatriptan and zolmitriptan. If patients do not respond to one 5HT1 receptor agonist, another can be used. Sumatriptan and zolmitriptan can also be used to treat cluster headache.
Despite their widespread use, clinically relevant interactions with 5HT1 receptor agonists are not frequently encountered. One reason for this could be because migraines most commonly occur in younger patients, who are unlikely to be taking multiple drugs for other conditions[1]
. This article discusses some of the known interactions involving 5HT1 receptor agonists.
Pharmacokinetic interactions
5HT1 receptor agonists are metabolised via various different metabolic pathways and therefore do not all necessarily share the same pharmacokinetic interactions. Naratriptan is unlikely to be involved in important pharmacokinetic interactions because half the dose is excreted unchanged and the rest is metabolised by a variety of isoenzymes.
CYP3A4 inhibition and induction are important mechanisms for potential interactions for eletriptan and almotriptan, which are both metabolised by CYP3A4. A randomised, crossover study in 16 healthy subjects has shown that ketoconazole, a potent CYP3A4 inhibitor, increased the area under the curve (AUC) of almotriptan by 57%[2]
and a pharmacokinetic study conducted by the manufacturer of eletriptan found that ketoconazole increased the AUC of eletriptan 5.9-fold[3]
. CYP3A4 is not the only route of metabolism for almotriptan, so inhibition of this isoenzyme by ketoconazole has a less dramatic effect on its exposure than with eletriptan. Other potent inhibitors of CYP3A4 would be expected to interact similarly (see
Stockley’s Drug Interactions
for a full list).
It is not necessary to adjust the dose in patients taking almotriptan with ketoconazole or other potent CYP3A4 inhibitors. However the US manufacturer (Ortho-McNeil Pharmaceutical) recommends an initial dose of 6.25mg for patients starting almotriptan who are taking potent CYP3A4 inhibitors[4]
.
On account of the marked increase in exposure to eletriptan, concurrent use with ketoconazole or other potent CYP3A4 inhibitors should be avoided[3]
, and the US manufacturer (Pfizer) additionally recommends that eletriptan should not be given within 72 hours of potent CYP3A4 inhibitors[5]
.
Erythromycin, which is a moderate inhibitor of CYP3A4, has been shown to increase eletriptan exposure by 3.6 fold[3]
. Concurrent use should therefore be avoided. Verapamil, another moderate CYP3A4 inhibitor, had a negligible effect on the exposure to almotriptan[6]
, therefore no dose adjustments would seem necessary on concurrent use. Other moderate CYP3A4 inhibitors (see Stockley’s Drug Interactions for a list) would be expected to have a similar effect.
Despite a lack of clinical reports, inducers of CYP3A4 are predicted to decrease the exposure to both eletriptan and almotriptan, potentially leading to a decrease in their efficacy. However, further study is needed.
Other 5HT1 receptor agonists are expected to have little or no interaction with inhibitors or inducers of CYP3A4, as they are not predominantly metabolised by this route.
CYP1A2 inhibition and induction can affect zolmitriptan and frovatriptan. In a crossover study in 16 healthy subjects, cimetidine, a weak non-specific inhibitor of several cytochrome P450 isoenzymes including CYP1A2, increased the AUC of zolmitriptan by 48% and increased the AUC of its active metabolite by 100%[7]
. Based on the effect of cimetidine on zolmitriptan exposure, fluvoxamine (a potent CYP1A2 inhibitor) is expected to increase the plasma concentration of zolmitriptan. The UK manufacturer of zolmitriptan (AstraZeneca UK) consequently recommends a maximum dose of 5mg in 24 hours for zolmitriptan in patients taking CYP1A2 inhibitors[8]
(see Stockley’s Drug Interactions for a list).
Fluvoxamine has been shown to increase the plasma concentration of frovatriptan by up to 49%[9]
. While the increase is not considered clinically important, the manufacturer of frovatriptan (A Menarini Pharma UK) does advise caution and strict adherence to the recommended dose (2.5mg repeated after at least two hours if necessary, with a maximum dose of 5mg in 24 hours)[10]
.
CYP1A2 inducers, such as tobacco smoke, are expected to decrease the exposure to frovatriptan and zolmitriptan. A retrospective analysis of pharmacokinetic data from phase I studies found a lower AUC and maximum plasma concentration of frovatriptan in smokers when compared with non-smokers[11]
. As the observed change was only slight, it is thought that any interaction between frovatriptan with tobacco smoke is unlikely to be clinically relevant. The effect of smoking on zolmitriptan metabolism does not appear to have been studied.
Monoamine oxidase A (MAO-A) inhibition
can affe
ct almotriptan, rizatriptan, sumatriptan and zolmitriptan, which are all metabolised by the enzyme.
Ph
armacokinetic studies have shown that moclobemide, a reversible inhibitor of MAO-A, can affect exposure. The AUC of almotriptan increased by 37%[12]
, the AUC of rizatriptan was increased 2.2-fold[13]
, the AUC of sumatriptan increased 2.3-fold[14]
and the AUC of zolmitriptan increased by 26% (an
d that of its active metabolite incr
eased three-fold)[8]
.
The interactions of moclobemide with rizatriptan and sumatriptan are established and clinically relevant. There seems to be no direct evidence of an interaction between rizatriptan or sumatriptan and non-selective MAO inhibitors (e.g. phenelzine), nevertheless, they would be expected to behave similarly. Consequently, rizatriptan[15],[16]
and sumatriptan[17],[18]
are contraindicated in patients taking, and for two weeks after the use of, selective or non-selective MAO inhibitors.
Although the increase in zolmitriptan exposure is slight, the UK manufacturer (AstraZeneca UK) advises that, if used in patients taking moclobemide or other MAO-A inhibitors, the dose of zolmitriptan should not exceed 5mg in 24 hours[8]
. The US manufacturer (AstraZeneca Pharmaceuticals LP) states that zolmitriptan should be avoided in patients who have taken a MAO-A inhibitor within the last two weeks[19]
.
Moclobemide does not affect the pharmacokinetics of frovatriptan[20]
and would not be expected to affect eletriptan and naratriptan pharmacokinetics as they, like frovatriptan, are not metabolised by MAO-A.
Propranolol, a drug also used in the prevention of migraine, has been shown to affect the pharmacokinetics of rizatriptan, possibly through inhibition of MAO-A. In a series of double-blind, placebo-controlled studies conducted in 51 healthy subjects, the AUC of rizatriptan increased by 67%, and a four-fold increase in AUC was observed in one patient[21]
. The manufacturers of rizatriptan (Merck) therefore recommend a dose of 5mg is used in patients taking propranolol, with a maximum of two (UK advice) or three (US advice) doses in 24 hours[15],[16]
.
Other beta-blockers used for the prevention of migraine (e.g., atenolol, nadolol, metoprolol and timolol) have all been shown in vitro to have no effect on the metabolism of rizatriptan[21]
and are therefore unlikely to have an effect in clinical practice. No clinically important interactions appear to occur between other 5HT1 receptor agonists and beta-blockers.
Pharmacodynamic interactions
5HT1 receptor agonists are generally contraindicated in patients taking ergot derivatives (e.g. ergotamine, dihydroergotamine and methysergide) because there is a theoretical risk of additive vasoconstriction. The UK manufacturers of sumatriptan[18] (GlaxoSmithKline), almotriptan[22] (Almirall), rizatriptan[15]
(Merck Sharp & Dohme) and zolmitriptan[8]
(AstraZeneca UK) state that ergotamine should not be given less than six hours after taking a 5HT1 receptor agonist, and that a 5HT1 receptor agonist should not be taken for at least 24 hours after ergotamine. The UK manufacturers of eletriptan[3]
(Pfizer), frovatriptan[10]
(A Menarini Pharma UK) and naritriptan[23]
(GlaxoSmithKline) recommend that 5HT1 receptor agonists should not be taken less than 24 hours after taking ergotamine or other ergot derivatives.
Selective serotonin reuptake inhibitors (SSRIs) increase the amount of 5-HT (serotonin) at post-synaptic receptors. In theory, 5HT1 receptor agonists may add to the effects of these increased amounts of serotonin. SSRIs have frequently been prescribed with 5HT1 receptor agonists and, while adverse reactions such as dyskinesia, weakness and incoordination have occasionally occurred[24],[25]
a drug interaction causing serotonin syndrome appears to be extremely rare[26],[27]
. Some reports, including from the American Headache Society, conclude that while concurrent use should not necessarily be avoided, patients should be monitored closely[28],[29],[30]
. The US Food and Drug Administration (FDA) recommends that patients given a 5HT1 receptor agonist with an SSRI or a serotonin and norepinephrine reuptake inhibitor (e.g. venlafaxine) should be informed of the possibility of serotonin syndrome and be monitored closely[31]
. Serotonin syndrome may also occur with concurrent use of MAO inhibitors and 5HT1 receptor antagonists[10],[16],[17],[22]
.
This article has been produced by Harpreet K Sandhu, Claire L Preston, and Stephanie Jones on behalf of the Stockley’s Drug Interactions editorial team. The book is available in print through Pharmaceutical Press (www.pharmpress.com) or electronically with quarterly updates through MedicinesComplete (www.medicinescomplete.com).
References
[1] Rolan P. Drug interactions with triptans: which are clinically significant? CNS Drugs 2012;26:949–957.
[2] Fleishaker JC, Herman BD, Carel BJ et al. Interaction between ketoconazole and almotriptan in healthy volunteers. J Clin Pharmacol 2003;43:423–427.
[3] Relpax (Eletriptan hydrobromide). Pfizer Ltd. UK Summary of product characteristics, May 2014.
[4] Axert (Almotriptan malate). Ortho-McNeil Pharmaceutical Inc. US Prescribing information, August 2014.
[5] Relpax (Eletriptan hydrobromide). Pfizer Inc. US Prescribing information, November 2013.
[6] Fleishaker JC, Sisson TA, Carel BJ et al. Pharmacokinetic interaction between verapamil and almotriptan in healthy volunteers. Clin Pharmacol Ther 2000;67:498–503.
[7] Dixon R, French S, Kemp J et al. The metabolism of zolmitriptan: effects of an inducer and an inhibitor of cytochrome P450 on its pharmacokinetics in healthy volunteers. Clin Drug Invest 1998;15:515–522.
[8] Zomig Tablets (Zolmitriptan). AstraZeneca UK Ltd. UK Summary of product characteristics, December 2012.
[9] Wade A, Buchan P, Mant T et al. Frovatriptan has no clinically significant interaction with fluvoxamine. Cephalalgia 2001;21:427.
[10] Migard (Frovatriptan succinate monohydrate). A. Menarini Pharma UK SRL. UK Summary of product characteristics, November 2014.
[11] Buchan P. Effects of alcohol, smoking and oral contraceptives on the pharmacokinetics of frovatriptan. Eur J Neurol 2000;7(Suppl 3):86–87.
[12] Fleishaker JC, Ryan KK, Jansat JM et al. Effect of MAO-A inhibition on the pharmacokinetics of almotriptan, an antimigraine agent in humans. Br J Clin Pharmacol 2001;51:437–441.
[13] van Haarst AD, van Gerven JMA, Cohen AF et al. The effects of moclobemide on the pharmacokinetics of the 5-HT 1B/1D agonist rizatriptan in healthy volunteers. Br J Clin Pharmacol 1999;48:190–196.
[14] Glaxo Pharmaceuticals UK Limited. Data on file. A study to determine whether the pharmacok inetics, safety or tolerability of subcutaneously administered sumatriptan (6 mg) are altered by interaction with concurrent oral monoamine oxidase inhib itors (Protocol C92–050). 1993.
[15] Maxalt (Rizatriptan benzoate). Merck Sharp & Dohme Ltd. UK Summary of product characteristics, March 2014.
[16] Maxalt (Rizatriptan benzoate). Merck & Co., Inc. US Prescribing information, March 2015.
[17] Imitrex Tablets (Sumatriptan succinate). GlaxoSmithKline. US Prescribing information, November 2013.
[18] Imigran Radis Tablets (Sumatriptan succinate). GlaxoSmithKline UK. UK Summar y of product characteristics, August 2014.
[19] Zomig (Zolmitriptan). AstraZeneca Pharmaceuticals LP. US Prescribing information, September 2012.
[20] Buchan P, Ward C & Freestone S. Lack of interaction between frovatriptan a nd monoamine oxidase inhibito r. Cephalalgia 1999;19:364.
[21] Goldberg MR, Sciberras D, De Smet M et al. Influence of β-adrenoceptor antagonists on the pharmacokinetics of rizatriptan, a 5-HT1B/1D agonist: differential effects of propranolol, nadolol and metoprolol. Br J Clin Pharmacol 2001;52:69–76.
[22] Almogran (Almotriptan hydrogen malate). Almirall Ltd. UK Summary of product characteristics, July 2015.
[23] Naramig (Naratriptan hydrochloride). GlaxoSmithKline UK. UK Summary of produ ct characteristics, December 2014.
[24] Abraham JT, Brown R, Meltzer HY. Clozapine treatment of persistent paroxysmal dyskinesia associated with concomitant paroxetine and sumatriptan use. Biol Psychiatry 1997;42:144–146.
[25] GlaxoWellcome. Personal communication, August 1997.
[26] Tepper S, Allen C, Sanders D et al. Coprescription of triptans with potentially interacting medications: a cohort study involving 240,268 patients. Headache 2003;43:44–48.
[27] Shapiro RE & Tepper SJ. The serotonin syndrome, triptans, and the potential for drug–drug interactions. Headache 2007;47:266–269.
[28] Gardner DM & Lynd LD. Sumatriptan contraindications and the serotonin syndrome. Ann Pharmacother 1998;32:33–38.
[29] Joffe RT & Sokolov STH. Co-administration of fluoxetine and sumatriptan: the Canadian experience. Acta Psychiatr Scand 1997;95:551–552.
[30] Evans RW, Tepper SJ, Shapiro RE et al. The FDA alert on serotonin syndrom e with use of triptans combined with selective serotonin reuptake inhibitors or selective serotonin-norepinephrine reuptake inhibitors: American Headache Society position paper. Headache 2010;50:1089–1099.
[31] FDA Information for Healthcare Professionals. Selective serotonin reuptake inhibitors (SSRIs) selective serotonin-norepinephrine reuptake inhibitors (SNRIs) 5-hydroxytryptamine receptor agonists (triptans). 19 July 2006.


