Science Photo Library
In this article you will learn:
- The current pharmacological strategies for management of patients with type 2 diabetes
- The status of newer therapies targeting the incretin axis and renal glucose handling
- The status of newer, longer-acting insulins
Diabetes affects around 382 million people worldwide[1]
and the numbers are increasing. In the UK, more than 2.8 million people have type 2 diabetes with an estimated cost to the NHS of £12bn a year[2]
. On account of rising obesity and changes in the ethnic make up of the UK population, the number of people in the UK with diabetes is expected to rise by over 50% by 2030[3]
. This represents a huge societal and financial burden on healthcare systems.
Type 2 diabetes is a metabolic disorder characterised by persistent hyperglycaemia caused by the body’s own resistance to endogenous insulin and an inevitable gradual failure of pancreatic beta cells to respond and produce sufficient insulin to meet demand. Genetic factors predispose people to developing type 2 diabetes, but it is strongly linked with obesity and modern inactive and unhealthy lifestyles. People from ethnic minorities in the UK are more likely to have type 2 diabetes than the general population[3]
. Family history is an important risk factor and twin studies have shown higher concordance for diabetes in monozygotic compared with dizygotic twins[4]
. More than 65 genetic variants have been identified that increase the risk of a person developing diabetes[5]
, but it is not currently possible to use this information clinically to ascertain an individual’s risk. Interventions aimed at modifiable risk factors, such as reducing obesity and increasing exercise, do however reduce the risk of developing diabetes[6],
[7]
.
The morbidity from type 2 diabetes predominantly relates to its microvascular and macrovascular complications. Patients with type 2 diabetes are at higher risk of stroke and cardiovascular disease as well as renal impairment, retinopathy and peripheral nerve damage. Data from the 2012–2013 National Diabetes Audit showed that in patients with diabetes, the risk of stroke increased by 62.6%, angina by 138.8%, heart attack by 94.2% and end-stage renal failure requiring renal replacement therapy by 272.3%[8]
.
While the control of blood sugars, blood pressure and cardiovascular risk can improve outcomes[9]
, current treatment options are not without problems, frequently leading to weight gain and increased risk of hypoglycaemia. This article will discuss the current management options and potential future therapies for patients with type 2 diabetes.
Current management
UK strategies for the management of type 2 diabetes are currently based on evidence from The UK Prospective Diabetes Study (UKPDS), a large prospective study in patients newly diagnosed with type 2 diabetes that spanned over three decades[9]
. The results of this study established that improving glycaemic control significantly reduced the rate of diabetes complications, including retinopathy, neuropathy, nephropathy and diabetes related deaths. Data from the study showed that for every 1% reduction in glycated haemoglobin (HbA1C), there was a 35% reduction in microvascular complications and a 25% reduction in diabetes-related deaths[10]
. Importantly, the reduction in diabetes-related risk shows a ‘legacy effect’; the improved outcomes for those with better controlled blood sugars persisted for many years after the study had finished, even though the difference in glycaemic control ceased after the trial ended[11]
. Early diagnosis and more aggressive treatment of blood glucose levels is therefore associated with improved clinical outcomes.
Metformin is unequivocally the first-line treatment in patients with type 2 diabetes. It belongs to the biguanide class of drugs and acts by increasing hepatic insulin sensitivity. It also increases the uptake of glucose into peripheral cells, reduces hepatic glucose production and aids weight loss[12]
. Metformin can induce gastrointestinal side effects such as abdominal bloating, cramps, nausea, vomiting and diarrhoea, which can be mitigated by starting metformin at a low dose. The British National Formulary recommends starting at 500mg of metformin once daily for at least a week prior to titrating the dose up to a maximum to 2g daily in divided doses[13]
. Caution is advised when used in patients with impaired renal function or other conditions that may increase the risk of lactic acidosis, such as acute heart failure or shock[13]
. However, a Cochrane review of trials that included patients on metformin suggests that the potential risk of developing lactic acidosis is often overstated[14]
.
Sulfonylureas (e.g. gliclazide, glimepiride, meglitinides) are commonly used as second-line agents in patients with type 2 diabetes, but can also be used as an alternative first-line treatment instead of metformin if the patient is not overweight, or is unable to tolerate metformin. Sulfonylureas can also be added to metformin if glycaemic control is inadequate. Sulfonylureas act by binding to a specific receptor on pancreatic beta cells, leading to increased secretion of endogenous insulin. The main side effects of sulfonylureas are weight gain and hypoglycaemia[15]
, and risk is increased in people with mild to moderate renal impairment and severe hepatic impairment[16]
.
Thiazolidinediones (e.g. pioglitazone) are an alternative second-line or a third-line therapy, although they have increasingly lost favour because of their adverse effects. The National Institute for Health and Care Excellence (NICE) recommends that they should be considered as second-line therapies, in addition to metformin, if the risk of hypoglycaemia with sulphylureas would be unacceptable, for example if a patient lives alone in vulnerable circumstances or if sulphonylureas are not tolerated. NICE suggests that in these cases the risks and benefits should be discussed with each patient[17]
. Thiazolidinediones act via the peroxisome proliferator-activated receptor-γ (PPAR-γ), a nuclear transcription factor to decrease insulin resistance and have been shown to lead to a significant reduction in HbA1C, both as a monotherapy and when used in combination with other oral agents such as metformin and/or sulphonylureas. Thiazolidinediones are associated with an increased fracture risk[5]
and in some patients may have led to heart failure[15]
. In 2010, the European Medicines Agency (EMA) suspended marketing authorisation for rosiglitazone as new evidence suggested that its cardiovascular risks outweighed its benefits[17]
. There is also a possible increased risk of bladder cancer with use of pioglitazone[15]
.
Insulin replacement therapy will eventually be required in the majority of patients with type 2 diabetes. Ideally, this would mimic the normal pattern of insulin secretion, where a background level of insulin is supplemented by higher release of insulin to match the glucose load following a meal. Oral agents are usually continued in patients who are starting insulin, but this may need to be reviewed if hypoglycaemia is a problem. Broadly, there are three strategies of insulin replacement; a basal insulin alone, twice daily biphasic insulin containing a mix of rapid-acting and long-acting insulins and a basal bolus regimen with a long-acting insulin, with additional doses of a short acting insulin given at meal times. Patients with type 2 diabetes who are already taking oral agents may initially only need a long acting basal insulin to improve their glycaemic control. Alternatively, a twice daily premixed insulin can be used to provide both a long-acting and short-acting insulin. This is potentially more convenient, but is less flexible than other regimens and may be better for patients with regimented mealtimes. A basal bolus regimen is more flexible but has the disadvantage of requiring four injections each day. All insulin regimens are associated with an increased risk of hypoglycaemia and can cause weight gain. In addition, fear of injections, perceived complexity of the treatment regimens, and concern about failure to self-manage the disease can form barriers to starting insulin treatment[18]
.
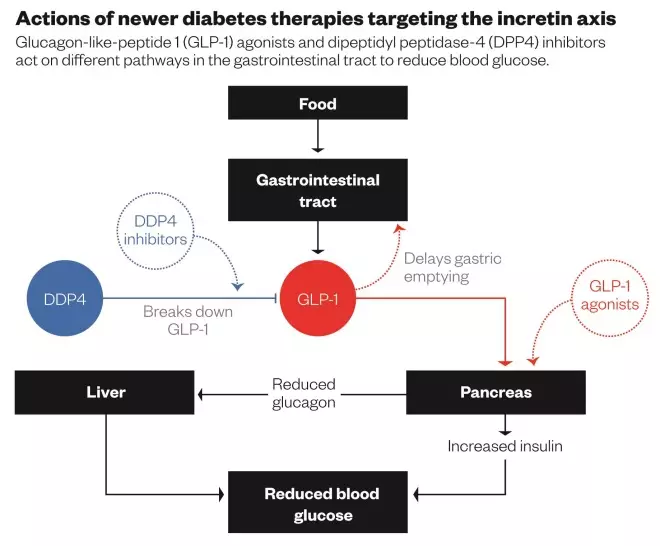
Newer therapies targeting the incretin axis
In recent years, greater understanding of the normal physiology of insulin release and technological advances in drugs and therapeutics has led to new targets to improve glycaemic control. One such target is the incretin axis. In non-diabetic individuals, the insulin response is increased following ingestion of food as a result of the release of incretin hormones including glucagon-like peptide-1 (GLP-1). This response is reduced in patients with diabetes. The incretin hormones lead to glucose dependent insulin release and reduced glucagon release. In vivo the incretin hormones are quickly broken down by the hormone dipeptidyl peptidase-4 (DDP4)[19]
.
In vivo, endogenous GLP-1 has a half-life of a few minutes as it is rapidly degraded by DDP4. GLP-1 receptor agonists (e.g. exenatide, liraglutide, lixisenatide, dulaglutide) target the incretin axis by increasing the action of GLP-1. Exenatide is derived from the saliva of the Gila monster and is structurally similar to GLP-1, leading to longer lasting glucose dependent insulin release[19]
. Liraglutide is another synthetic GLP-1 which resists degradation by DDP4 by fatty acid substitution[19]
. Collectively, GLP-1 receptor agonists increase insulin release, decrease glucagon release and slow gastric emptying[19]
(see ‘Actions of newer diabetes therapies targeting the incretin axis’). In contrast to many diabetes treatments, GLP-1 receptor agonists aid weight loss, and liraglutide was recently licensed for non-diabetic individuals as a weight loss treatment[20]
. A common side effect of GLP-1 receptor agonists is nausea, which is usually temporary and disappears around two weeks after treatment initiation. In addition, GLP-1 receptors also increase satiety and augment weight loss[19]
. At present, GLP-1 receptor agonists are only available in an injectable form[19]
.
DDP4 inhibitors (e.g. sitagliptin, linagliptin, saxagliptin, vildagliptin) are recommended by NICE as an alternative second-line or third-line therapy[17]
. Because of their mechanism of action, DDP4 inhibitors have a low risk of hypoglycaemia and do not lead to weight gain[21]
.
Newer therapies targeting renal glucose handling
Sodium glucose co transporter 2 (SGLT2) inhibitors (e.g. dapagliflozin, canagliflozin, empagliflozin) are more suitably termed as ‘gluco-uretic’ agents and provide a novel target for controlling blood sugar levels via the kidneys. Under normal conditions, glucose is filtered out of the blood by the kidneys via a transporter protein (SGLT-2). By blocking the action of these transporters, more glucose is excreted in the urine. SGLT2 inhibitors lower blood glucose with a low risk of hypoglycaemia[22]
. The increased excretion of glucose can cause osmotic effects that may lead to hypotension and dehydration, particularly in patients taking diuretics[22]
. They also result in modest improvements in weight and blood pressure. The main side effects of SGLT2 inhibitors are an increase in fungal genital infections and urinary tract infections; an effect seen more commonly in women then in men[22]
.
Newer insulins
Longer acting insulins have been developed to provide a more stable basal insulin profile over a 24-hour period. The action of insulin can be delayed by increasing its molecular size and slowing its absorption. Degludec is formed of hexameric chains that slowly separate, releasing the active monomer that can then be absorbed. In clinical trials, in patients with type 2 diabetes, it was non inferior to glargine and had lower levels of hypoglycaemic episodes, particularly at night (nocturnal hypoglycaemia)[23]
. The long half-life of degludec compared with traditional, long-acting insulins means that patients can be much more flexible about the timing of their basal insulin doses, without compromising their glycaemic control. This may be particularly useful for people with erratic lifestyles. Glargine U300 (Toujeo) is a more concentrated form of insulin glargine available as 300 units/ml in a pre-filled pen. U300 also has a longer half-life compared with glargine. In trials, it was associated with fewer nocturnal hypoglycaemic episodes than glargine, with no change in the overall glycaemic control[23]
.
The need to regularly inject insulin can be a barrier for optimal treatment for many patients. Novel delivery routes, such as inhaled insulin, may lead to better compliance and control. Inhaled insulin, now available in many countries as Afrezza, utilises the large and well perfused surface area of the lungs for uptake of microparticles containing short acting insulin[24]
. This does not replace the need for basal insulin injections, but it could replace the meal time insulin requirements. Efficacy and safety data from a trial that included both type 1 and type 2 diabetic patients receiving inhaled insulin has shown equivalent glycaemic control to injected boluses of insulin[24]
. The main side effects of inhaled insulin are hypoglycaemia and throat pain.
New NICE guidelines
Formal guidelines for the management of type 2 diabetes are currently undergoing an update and have not yet been published. However, draft guidance documents do not suggest a paradigm shift in management strategies currently available. Although SGLT-2 inhibitors are mentioned, the place of these drugs and the newer concentrated insulins in the treatment algorithm of type 2 diabetes has not yet been fully elucidated.
Non-glycaemic approaches to type 2 diabetes
Although this article focuses on the pharmacological options for achieving optimal glycaemic control, the importance of patient education and supporting people to look after their own long term condition, through controlling blood pressure, lipids, smoking cessation and other cardiovascular risk factors, cannot be underestimated. There is evidence to suggest that lowering blood pressure significantly reduces diabetes related deaths, strokes, heart failure and microvascular complications[25]
. Angiotensin-converting enzyme inhibitors, such as ramipril, are preferred as first-line drugs because they limit the progression of renal damage[26]
. In comparison to glycaemic control, good blood pressure control does not show a ‘legacy effect’ and control must be maintained to preserve a benefit[11]
. NICE recommends that all patients should be offered a structured education programme to empower them to better understand and manage their condition[26]
.
As the incidence of type 2 diabetes rises along with the rate of diabetes complications, diabetes management must achieve good glycaemic control alongside optimal control of cardiovascular risk factors and empowering people to look after their own chronic condition. Such a multifaceted targeted approach is vital, not just to the individual but to the healthcare system as a whole. Although metformin, sulphonylureas and insulin will remain important drug choices for people with type 2 diabetes, newer drugs such as the GLP-1 agonists, DDP4 inhibitors and SGLT2 inhibitors and the newer insulin analogs provide an unique opportunity to target different underlying pathophysiological defects and are poised to play a larger role in the treatment paradigm of type 2 diabetes. Meanwhile, the expectation is that the new (revised) NICE guidelines can further guide, inform and improve this decision making process.
Mary E Packer, BM BCh, MRCP, is registrar in acute medicine and Winston Crasto is consultant in diabetes & endocrinology at George Eliot Hospital NHS Trust, Nuneaton.
References
[1] Diabetes Facts and Stats: 2014 — Diabetes UK, published 2014. Available at: https://www.diabetes.org.uk/About_us/What-we-say/Statistics/
[2] Kanavos P, van den Aardweg S & Schurer W. LSE Health. Diabetes expenditure, burden of disease and management in 5 EU countries (January 2012). Available at: http://www.lse.ac.uk/LSEHealthAndSocialCare/research/LSEHealth/MTRG/LSEDiabetesReport26Jan2012.pdf
[3] Public Health England. Adult obesity and type 2 diabetes. July 2014. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/338934/Adult_obesity_and_type_2_diabetes_.pdf
[4] Kapiro J, Tuomilehto M, Koskenvuo M et al. Concordance for type 1 (insulin-dependent) and type 2 (non-insulin-dependent) diabetes mellitus in a population-based cohort of twins in Finland. Diabetologia 1992;35:1060–1067. doi:10.1007/bf02221682
[5] Lyssenko V & Laakso M. Genetic Screening for the Risk of Type 2 Diabetes. Diabetes Care 2013;36(2):S120–126. doi:10.2337/dcS13-2009
[6] Tuomilehto J, Lindström J, Eriksson JG et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001;344(18):1343–1350. doi:10.1056/nejm200105033441801
[7] Li G, Zhang P, Wang J et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow- up study. Lancet 2008;371(9626):1783–1789. doi:10.1016/s0140-6736(08)60766-7
[8] Health and Social Care Information Centre, National Diabetes Audit 2012–2013. Report 2: Complications and Mortality. Available at: http://www.hscic.gov.uk/catalogue/PUB16496/nati-diab-audi-12-13-rep2.pdf
[9] King P, Peacock I & Donnelly R. The UK Prospective Diabetes Study (UKPDS): clinical and therapeutic implications for type 2 diabetes. Br J Clin Pharmacol 1999;48(5):643–648. doi:10.1046/j.1365-2125.1999.00092.x
[10] American Diabetes Association. Implications of the United Kingdom Prospective Diabetes Study. Diabetes Care 2000;23(1):S27–31. PMID: 12017673
[11] Campbell IW. The UK Prospective Diabetes Study (UKPDS): Its legacy for type 2 diabetes management. Prim Care Cardiovasc J 2009;2(1):48–49. doi:10.3132/pccj.2009.012
[12] UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 1998;352(9131):854–865. doi:10.1016/s0140-6736(98)07037-8
[13] Metformin hydrochloride. British National Formulary. September 2015. doi:10.18578/bnf_147942626
[14] Salpeter SR, Greyber E, Pasternak GA et al. Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database of Systematic Reviews 2010;14(4):CD002967. doi:10.1002/14651858.CD002967.pub4
[15] Tran L, Zielinski A, Roach AH et al. The pharmacologic treatment of type 2 diabetes: oral medications. Ann Pharmacother 2015;49(5):540–556. doi:10.1177/1060028014558289
[16] Sulphonylureas. British National Formulary. September 2015. doi:10.18578/bnf_147942626
[17] National Institute for Health and Clinical Excellence. Type 2 diabetes: newer agents; NICE short clinical guideline 87, May 2009. Available at: https://www.nice.org.uk/guidance/ta203/documents/nice-recommends-liraglutide-for-type-2-diabetes-mellitus4
[18] Fonseca VA & Haggar MA. Achieving glycaemic targets with basal insulin in T2DM by individualizing treatment. Nat. Rev. Endocrinol 2014;10(5);276–281. doi:10.1038/nrendo.2014.17
[19] Prasad-Reddy L & Isaacs D. A clinical review of GLP-1 receptor agonists: efficacy and safety in diabetes and beyond. Drugs Context. 2015;4:212283. doi:10.7573/dic.212283
[20] Pi-Sunyer X, Astrup A, Fuijoka K et al. A randomized, controlled trial of 3.0 mg of liraglutide in weight management. N. Engl. J. Med. 2015;373(1):11–22. doi:10.1056/nejmoa1411892
[21] Röhrborn D, Wronkowitz N & Eckel J. DPP4 in diabetes. Front Immunol 6:386. doi:10.3389/fimmu.2015.00386
[22] Nauck MA. Update on developments with SGLT2 inhibitors in the management of type 2 diabetes. Drug Design, Development and Therapy 2014:8;1335–1380. doi:10.2147/DDDT.S50773
[23] Woo VC. New Insulins and New Aspects in Insulin Delivery. Can J Diabetes 2015;39(4):335–343. doi:10.1016/j.jcjd.2015.04.006
[24] Khadka A, Anantharamu T, Brashier DBS et al. Inhaled insulin: A “puff” than a “shot” before meals. Pharmacol Pharmacother. 2015;6(3):126–129. doi:10.4103/0976-500x.162013
[25] UK Prospective Diabetes Study (UKPDS) Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703. doi:10.1136/bmj.317.7160.703
[26] NICE Clinical Guidelines. Type 2 Diabetes, National Clinical Guideline for Management in Primary and Secondary Care (updated 2014).


