
MAG / Shutterstock.com
As humans, we all make errors, both professionally and in our personal lives. We sometimes forget to do things, get distracted and do the wrong thing, and make what turn out to be wrong decisions. Within the UK pharmacy setting, dispensing errors occur in 0.04–9.8% of dispensed items in community pharmacy, and 0.008–0.02% within hospital pharmacy[1],
[2],
[3],
[4],
[5]
. The wide range is at least partly a result of different definitions of error and different methods used to detect them. The most common types of error identified in such studies include the wrong drug, wrong strength, wrong dosage form, wrong quantity and incorrect labelling[6]
. Pharmacists are also involved in identifying and rectifying the prescribing errors that occur in around 5% of prescribed medicines in UK general practice[7]
and 7% of prescribed medicines in hospitals[8]
. Psychological theories of human error can help us understand why these errors occur and identify strategies to prevent them. This article aims to provide pharmacy staff and other healthcare professionals with the background knowledge to understand theoretical models of human error and how they apply in clinical practice.
‘Person-centred’ versus ‘system-focused’ approaches to error
Historically, a person-centred approach to error has been taken, both in healthcare and elsewhere[9],
[10]
. This approach has the underlying philosophy that errors are caused by human weaknesses and that some humans are more prone to error than others. According to this model, error reduction involves identifying variation between individuals and then targeting those who make the most errors. This is, therefore, a blame-oriented approach, one that is likely to create fear and involve disciplinary sanctions, while also holding individuals responsible and liable for errors. It has been suggested that blaming individuals may be more emotionally satisfying than blaming institutions and is potentially more convenient than trying to address the wider system[11]
.
Since the 1990s, a system-focused model has been advocated instead[12]
. In contrast to the person-centred approach, this model’s philosophy is that errors are caused by systems of which humans form only one part. For example, the people who apparently make the most errors may be those carrying out the most high-risk tasks or who work in the most difficult environments. According to the systems model of error, addressing these task and environmental factors is more likely to be effective than disciplinary action aimed at the individuals concerned. Organisations using the systems approach seek to reduce errors by looking at a range of factors, including the organisation itself and its policies. In clinical settings, this would include the use of incident reporting, or other methods, to identify errors and share lessons learnt, make changes to the system, and reduce the chances of errors occurring in the future. For example, if two strengths of the same type of tablet are stored together in similar packaging, dispensing errors are likely to occur[11]
. Identifying this problem could lead to solutions, such as changing the packaging or changing how these products are stored to better aid their differentiation.
The accident causation model
An example of a model of human error based on a systems approach is James Reason’s accident causation model, which was published in 1990[12]
and has been applied in many contexts, including aviation and nuclear power[10]
. It has also been specifically adapted to healthcare[13]
and has been used to understand medication errors[5],
[11],
[14],
[15],
[16]
and patient non-adherence[17]
.
According to the accident causation model, a system has both a ‘sharp end’ and a ‘blunt end’ (see ‘Figure 1: The accident causation model’). At the sharp end, ‘active failures’ can occur on the part of front-line workers. These active failures are unsafe acts that can be classified into slips, lapses, mistakes and violations[12]
. Slips and lapses occur when the correct plan is made but then executed incorrectly. Specifically, a ‘slip’ occurs when a step of the plan is carried out incorrectly, whereas a ‘lapse’ occurs when a step of the plan is omitted or forgotten. Examples of slips that have been identified in clinical practice are selecting the wrong drug from a drop-down menu or intending to dispense one quantity of tablets but dispensing another[11]
. Lapses include a prescriber forgetting to cross a drug off a drug chart[14]
or a patient forgetting to take a dose of their medicine[17]
.
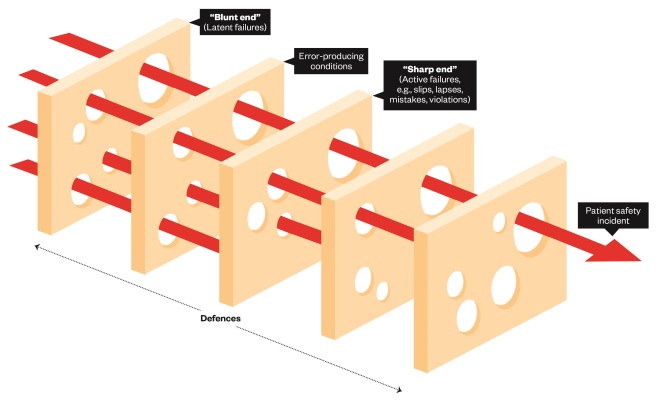
Figure 1: The accident causation model
Source: Adapted from Reason, J. Human Error. 1990. Cambridge: University Press, Cambridge.
According to James Reason’s accident causation model, a system has a ‘sharp end’ and a ‘blunt end’. At the sharp end, active failures or unsafe acts (e.g. slips, lapses, mistakes and violations) can occur on the part of frontline workers. In addition, ‘mistakes’ and ‘violations’ can occur when an incorrect plan is formulated and then followed. Active failures do not occur in isolation, but result from ‘error-producing conditions’ that arise at different levels within the system. A system has a series of defences to prevent an adverse outcome. Rather than being completely intact, each of these defences is seen as having holes in it (giving rise to the name ‘the Swiss cheese model’). These holes can arise as a result of active failures and latent conditions within the system. Even if one of these holes is penetrated, a potentially dangerous situation may be blocked by the next defence. However, a trajectory of ‘accident opportunity’ arises if the whole series of defences is penetrated.
In contrast to slips and lapses, ‘mistakes’ and ‘violations’ occur when an incorrect plan is formulated and then followed. Mistakes occur because of lack of, or misapplication of, the relevant rules or knowledge. Examples of mistakes are prescribing an incorrect dose because of a lack of knowledge of how a particular medicine is dosed[18]
, or a patient not taking their medicine because of an incorrect belief that it is contraindicated when drinking alcohol[17]
. Violations occur when a person knows the rule but makes a decision not to follow it – not with the intention to cause harm, but to save time or achieve a competing priority. An example is leaving a medical student to insert the dose on a paper prescription after it has been signed[14]
. For examples of the different types of active failure, see ‘Table 1: Examples of active failures resulting in failure to achieve the desired outcome’.
| Active failures | Examples based on driving to the airport for an early flight and missing the plane | Examples based on dispensing medicine |
|---|---|---|
| Slip | Started driving to the airport, but fell into mental ‘autopilot’ and took the route to work instead | Intended to dispense flucloxacillin but selected and dispensed amoxicillin instead |
| Lapse | Intended to set an alarm, but forgot to do so and overslept | Intended to dispense second item on prescription but forgot about it and failed to give it to the patient |
| Violation | Drove at 80mph and stopped by the police, resulting in a delay | Dispensed a controlled drug from a prescription that did not meet handwriting requirements before it had been corrected to avoid inconveniencing the patient |
| Mistake | Interpreted the flight time of 8am as the check-in time and arrived at the airport two hours late | A lack of knowledge about the differences between sodium valproate ‘chrono’ and ‘enteric-coated’, leading to the dispensing of the wrong preparation |
According to the accident causation model, these active failures do not occur in isolation, but result from ‘error-producing conditions’ that arise at different levels within the system[10]
. Within healthcare, these may relate to the patient, the task, the individual healthcare professional, the team, or the environment[13]
. Examples include lack of individual knowledge, lack of team communication and no access to a computer[19]
. Some analyses include technology as a separate group of error-producing conditions[15]
. In turn, error-producing conditions result from latent failures at the ‘blunt end’ of the system (i.e. those caused by the organisation or the surrounding culture). Examples include no one taking responsibility for the whole medication system in care homes[5]
, a tight budget to deliver a safe service[5]
, a lack of formal prescribing training in medical schools[19]
, and a lack of a culture of open communication between patients and prescribers[17]
.
The final part of the model is a system’s series of defences to prevent an adverse outcome (see figure 1). Within the medication-use process, these defences may include pharmacists, other healthcare professionals, double-checking systems, and the patient or their carers. However, rather than being completely intact, each of these defences is seen as having holes in it (giving rise to the name ‘the Swiss cheese model’). These holes can arise as a result of active failures and latent conditions within the system. Even if one of these holes is penetrated, a potentially dangerous situation may be blocked by the next defence. However, a trajectory of ‘accident opportunity’ arises if the whole series of defences is penetrated. Defences against prescribing errors have been identified as self-checking and checking by pharmacists and nurses[14]
. However, if an erroneous prescription gets through those defences, an error will reach the patient and may result in patient harm. Dean et al. also found that over-reliance on the pharmacist as a defence may result in compensatory behaviours, such as doctors not looking up doses when prescribing[14]
. Beso et al. identified a series of defences in place in a hospital pharmacy, including the dispenser noticing mistakes on a label in cases where the dispenser and labeller are different people, self-checking, and a stage where a final check on all dispensed items is carried out[11]
. However, pharmacy staff also identified that these defences have weaknesses: the dispenser may not notice an error, the drug may be dispensed from the label rather than the prescription, or dispensers could rely too much on the final checker to identify errors[11]
.
Other models
While Reason’s accident causation model has been the dominant model of human error used in healthcare to date, a more specific model — the Yorkshire contributory factors framework — was published in 2012 (see ‘Figure 2: The Yorkshire contributory factors framework’ and ‘Table 3: Definitions for factors in the Yorkshire contributory factors framework’)[20]
. This is based on a framework of factors contributing to patient safety incidents in hospital settings. In the centre of the framework are active failures, around which are a series of circles representing situational factors, local working conditions, and two layers of latent factors: those relating to the organisation itself and those relating to wider external policies. Advantages of this model are that it is more specific to healthcare and it is also evidence-based, having been developed following a systematic review of relevant literature. Disadvantages are that it is more complex than the accident causation model[20]
and relates to hospital settings only, with no current equivalent for primary care[21]
.
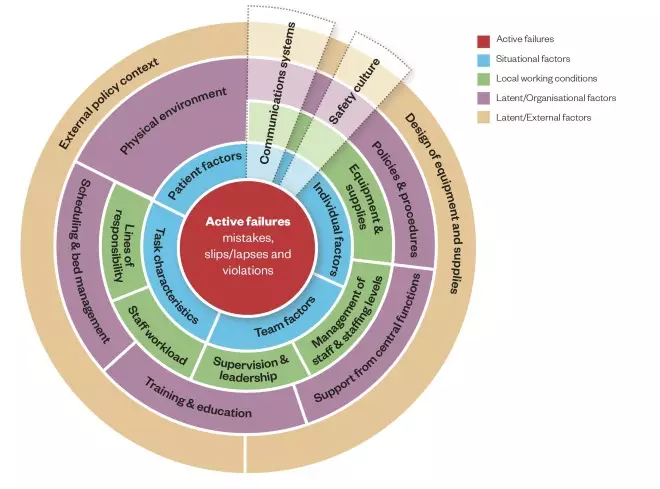
Figure 2: The Yorkshire contributory factors framework
Source: BMJ Qual Saf 2012;21:369–380.
This model is based on a framework of factors contributing to patient safety incidents in hospital settings. Active failures are included in the centre of the framework, around which are a series of circles representing situational factors, local working conditions, and two layers of latent factors: those relating to the organisation itself and those relating to wider external policies.
| Factor | Definition |
|---|---|
| Active failures | Any failure in performance or behaviour (e.g. error, mistake, violation) of the person at the ‘sharp end’ (e.g. the health professional) |
| Communication systems | Effectiveness of the processes and systems in place for the exchange and sharing of information between staff, patients, groups, departments and services. This includes both written (e.g. documentation) and verbal (e.g. handover) communication systems |
| Equipment and supplies | Availability and functioning of equipment and supplies |
| External policy context | Nationally driven policies/directives that impact on the level and quality of resources available to hospitals |
| Design of equipment and supplies | The design of equipment and supplies to overcome physical and performance limitations |
| Individual factors | Characteristics of the person delivering care that may contribute in some way to active failures. Examples of such factors include inexperience, stress, personality, attitudes |
| Lines of responsibility | Existence of clear lines of responsibility clarifying accountability of staff members and delineating the job role |
| Management of staff and staffing levels | The appropriate management and allocation of staff to ensure adequate skill mix and staffing levels for the volume of work |
| Patient factors | The features of the patient that make caring for them more difficult and therefore more prone to error. These might include abnormal physiology, language difficulties, personality characteristics (e.g. aggressive attitude) |
| Physical environment | Features of the physical environment that help or hinder safe practice. This refers to layout of the unit, the fixtures and fittings and the level of noise, lighting, temperature, etc. |
| Policy and procedures | The existence of formal or written guidance for the appropriate conduct of work tasks and processes. This can also include situations where procedures are available but contradictory, incomprehensible and of otherwise poor quality |
| Safety culture | Organisational values, beliefs and practices surrounding the management of safety and learning from error |
| Scheduling and bed management | Adequate scheduling to manage patient throughout, minimising delays and excessive workload |
| Staff workload | Level of activity and pressures on time during a shift |
| Supervision and leadership | The availability and quality of direct and local supervision and leadership |
| Support from central functions | Availability and adequacy of central services in support the functioning of wards/units. This may include support from information technology and human resources, portering services, estates or clinically related services such as radiology, phlebotomy and pharmacy |
| Task characteristics | Factors related to specific patient related tasks that may make individuals vulnerable to error |
| Team factors | Any factor related to the work of different professionals within a group that they may be able to change to improve patient safety |
| Training and education | Access to correct, timely and appropriate training, both specific (e.g. task related) and general (e.g. organisation related) |
Preventing error
According to these models of human error, we can prevent patient harm by stopping active failures from occurring — generally by targeting latent and error-producing conditions — and by creating more effective defences to block errors that do occur from actually reaching the patient. For example, latent failures existing in prescribing knowledge require suitable education and training strategies to resolve. These strategies may range from formal one-to-one sessions and group training, to looking at error monitoring and reporting systems as part of wider improvement programmes[22],
[23],
[24]
. Extra layers of defence can be introduced by information technology, such as clinical decision support[25]
. However, there are also holes in these defences, including alert fatigue, and new types of error-producing conditions can be introduced[26],
[27]
. As noted above, pharmacists often provide an extra layer of defence by reviewing and checking prescriptions and intervening to correct erroneous prescriptions before they can result in patient harm[22]
. The role that patients can play in preventing error is being increasingly recognised and several research groups are currently exploring how best to facilitate this[28],
[29]
. Models of human error illustrate how even the most experienced healthcare professionals can introduce errors, and so all healthcare professionals are potentially defences in the system and have an obligation to speak up if they are concerned. Effective communication between different healthcare professionals, and between healthcare professionals and patients, is often needed to activate these defences.
A series of tools, including flowcharts, fishbone diagrams, chronological mapping diagrams and action grids, have been developed based on Reason’s accident causation model to facilitate the investigation of incidents in clinical practice and to identify educational opportunities at a systems level (see Resources).
Conclusion
In summary, there has been some movement from a person-centred approach to a system-based approach of understanding error production and reduction in many areas, including healthcare. A systems approach focuses on improving the system rather than blaming individuals. Understanding models of human error can be helpful in understanding why errors have occurred in the past, where future vulnerabilities may lie, and how healthcare professionals might take action to make clinical practice safer.
Resources
Imperial College London. Systems analysis of clinical incidents: the London protocol. 1999. Available at: http://www.imperial.ac.uk/patient-safety-translational-research-centre/education/training-materials-for-use-in-research-and-clinical-practice/the-london-protocol/
Sara Garfield is a research pharmacist and Bryony Dean Franklin is director and professor of medication safety, the Centre for Medication Safety and Service Quality, Imperial College Pharmacy Department, Imperial College Healthcare NHS Trust, London & UCL School of Pharmacy, London.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
References
[1] Ashcroft DM, Qunilan P & Blenkinsopp A. Prospective study of the incidence, nature and causes of dispensing errors in community pharmacies. Pharmacoepidemiol Drug Safety 2005;14:327–332. doi: 10.1002/pds.1012
[2] Chua SS, Wong ICK, Edmonson H et al. A feasibility study for recording of dispensing errors and ‘near misses’ in four UK primary care pharmacies. Drug Safety 2003;26:803–813. doi: 10.2165/00002018-200326110-00005
[3] Franklin BD & O’Grady K. Dispensing errors in community pharmacy: frequency, clinical significance and potential impact of authentication at the point of dispensing. Int J Pharm Pract 2007;15:273–281. doi: 10.1211/ijpp.15.4.0004
[4] Franklin BD, Reynolds M, Sadler S et al. The effect of the electronic transmission of prescriptions on dispensing errors and prescription enhancements made in English community pharmacies: a naturalistic stepped wedge study. BMJ Quality & Safety 2014;23:629. doi: 10.1136/bmjqs-2013-002776
[5] Barber N, Alldred DP, Raynor DK et al. Care homes’ use of medicines study: prevalence, causes and potential harm of medication errors in care homes for older people. Qual Saf Health Care 2009;18:341–346. doi: 10.1136/qshc.2009.034231
[6] James KL, Barlow D, McArtney R et al. Incidence, type and causes of dispensing errors: a review of the literature. Int J Pharm Pract 2009;17:9–30 doi: 10.1211/ijpp.17.1.0004
[7] Avery AJ, Ghaleb M, Barber N et al. The prevalence and nature of prescribing and monitoring errors in English general practice – a retrospective case note review. British Journal of General Practice 2013;63:413–414. doi: 10.3399/bjgp13X670679
[8] Lewis PJ, Dornan T, Taylor D et al. Prevalence, incidence and nature of prescribing errors in hospital inpatients: a systematic review. Drug Saf 2009;32:379–389. doi: 10.2165/00002018-200932050-00002
[9] Greenwood M & Woods H. The incidence of industrial accidents upon individuals with special reference to multiple accidents. Her Majesty’s Stationery Office, London: 1919.
[10] Reason J. Human error: models and management The BMJ 2000;320:768–770. doi: 10.1136/bmj.320.7237.768
[11] Beso A, Franklin BD & Barber N. The frequency and potential causes of dispensing errors in a hospital pharmacy. Pharm World Sci 2005;27:182–190. doi: 10.1007/s11096-004-2270-8
[12] Reason J. Human Error. 1990. Cambridge: University Press, Cambridge. doi: 10.1017/CBO9781139062367
[13] Vincent C, Taylor-Adams SE & Stanhope N. Framework for analysing risk and safety in clinical practice. The BMJ 1998;316:1154–1157. doi: 10.1136/bmj.316.7138.1154
[14] Dean B, Schachter M, Vincent C et al. Prescribing errors in hospital inpatients The Lancet 2002;359:1373–1378. doi: 10.1016/S0140-6736(02)08350-2
[15] Slight SP, Howard R, Ghaleb M et al. The causes of prescribing errors in English general practices: a qualitative study. British Journal of General Practice 2013. doi: 10.3399/bjgp13X673739
[16] Taxis K & Barber N. Causes of intravenous medication errors: an ethnographic study. Qual Saf Health Care 2003;12:343–347. doi: 10.1136/qhc.12.5.343
[17] Barber N, Safdar A & Franklin BD. Can human error theory explain non-adherence? Pharm World Sci 2005;27:300–304. doi: 10.1007/s11096-005-0355-7
[18] Lewis P, Ashcroft DM, Dornan T et al. Exploring the causes of junior doctors’ prescribing mistakes: a qualitative study. Br J Clin Pharmacol 2014;78:310–319. doi: 10.1111/bcp.12332
[19] Tully MP, Ashcroft DM, Dornan T et al. The causes of and factors associated with prescribing errors in hospital inpatients: a systematic review. Drug Saf 2009;32:819–836. doi: 10.2165/11316560-000000000-00000
[20] Lawton R, McEachan RRC, Giles SJ et al. Development of an evidence-based framework of factors contributing to patient safety incidents in hospital settings: a systematic review. BMJ Qual Saf 2012;21:369–380. doi: 10.1136/bmjqs-2011-000443
[21] Lawton R & Armitage G. Psychological theories of medication use. In: Safety in medication use. Franklin BD, Tully M (Eds): C & C Press London 2015. doi: 10.1201/b18773-11
[22] The Health Foundation. Evidence scan: Reducing prescribing errors. The Health Foundation. London 2012.
[23] Montesi G & Lechi A. Prevention of medication errors: detection and audit. J Clin Pharmacol 2009;67:651–655. doi: 10.1111/j.1365-2125.2009.03422.x
[24] Reynolds M, Jheeta J, Benn J et al. Improving feedback on junior doctors’ prescribing errors: mixed methods evaluation of a quality improvement project. BMJ Quality and Safety 2016. doi: 10.1136/bmjqs-2015-004717
[25] Agrawal A. Medication errors: prevention using information technology systems. Br J Clin Pharmacol 2009;67:681–686. doi: 10.1111/j.1365-2125.2009.03427.x
[26] Koppel R, Metelay JP, Cohen A et al. Role of computerized physician order entry systems in facilitating medication errors. J Am Med Inform Assoc 2005;293:1197–1203. doi: 10.1001/jama.293.10.1197
[27] Ash JS, Berg M & Coiera E. Some unintended consequences of information technology in health care the nature of patient care information system-related errors. J Am Med Inform Assoc 2004;11:104–112. doi: 10.1197/jamia.M1471
[28] Lawton R & Armitage G. The role of the patient in clinical safety. London: The Health Foundation 2012.
[29] Garfield S, Jheeta S, Husson F et al. The role of hospital inpatients in supporting medication safety: A qualitative study. PLOS One 2016. doi: 10.1371/journal.pone.0153721


