This content was published in 2005. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
Quality of life and life expectancy for patients with sickle cell disease has improved considerably over the past 25 years. In 1973, their average life-span was 14 years. Now, it is closer to 50 years.1
The birth incidence of haemoglo-binopathies in the UK is approximately 250 per annum. This now exceeds cystic fibrosis and phenylketonuria births. The UK has an estimated 12,500 adults and children with a sickle cell disease.2 This term describes inherited abnormal haemoglobin formation due to the presence of haemoglobin S (HbS). There are three types of sickle cell disease: sickle cell anaemia, haemoglobin sickle cell disease and sickle beta thalassaemia. Of these, sickle cell anaemia is the most common.

An individual’s haemoglobin (Hb) is determined by his or her genetic make up. There are over 300 types of Hb, the most common being HbA, which refers to adult haemoglobin. Usually, one HbA gene is inherited from each parent. A healthy combination of two HbA genes (HbAA) results in the manufacture of HbA in red blood cells. These cells efficiently transport oxygen and maintain their flexible, round shape so they can easily travel through the body’s smallest capillaries.
Individuals who inherit an abnormal Hb gene from one parent and a normal HbA gene from the other have no disease, but are said to have a trait. An estimated 170,000 people in the UK have sickle cell trait.3 Estimates suggest that the sickle cell trait (HbAS) is present in3:
- One in four west Africans
- One in 10 Afro-Caribbeans
- One in 20–50 Asians
- One in 100 northern Greeks
The only time someone with sickle cell trait may be vulnerable is if there is limited oxygen (eg, at high altitudes or if under anaesthesia). A more common concern for people with the trait is if they have a child with another person also with the trait or with a carrier of another significant variant haemoglobin. Their child would have a 1 in 4 risk of being born with a sickle cell disease.
The sickle gene mutation arose in tropical areas. Children with the sickle cell trait are more resistant to falciparum malaria than those with two normal HbA genes (HbAA). However, those with two sickle cell genes (HbSS) will have sickle cell anaemia.
HbSS and sickle cell anaemia
A red blood cell containing only HbS and no normal HbA is capable of carrying oxygen but when the HbS gives up its oxygen to the tissues, the HbS molecules can crystallise. These crystals are sticky and stack up to form long rods, distorting the red cell, making it rigid and sickle shaped.
When the sickle-shaped red blood cells are reoxygenated they regain their original round shape but, with repeated oxygenation and deoxygenation, they become increasingly hard and brittle and, eventually, irreversibly sickled. Once irreversibly sickled, the cells are destroyed by the reticulo-endothelial system.Depending on the severity of the disease, sickle cells live for between five and 30 days, compared with the 120-day life-span of normal red blood cells. The shortened life-span of red cells leads to haemolytic anaemia. It is important to note that this is not the same as iron deficiency anaemia because the iron component of destroyed red blood cells is stored for reuse.
Identify knowledge gaps
- What are the symptoms of sickle cell anaemia?
- What drugs are involved in the management of sickle cell anaemia?
- What support can pharmacists give to patients with sickle cell anaemia?
Before reading on, think about how this article may help you to do your job better. The Royal Pharmaceutical Society’s areas of competence for pharmacists are listed in “Plan and record”, (available at: www.rpsgb.org/education). This article relates to “drug therapies” (see appendix 4 of “Plan and record”).
Symptoms and complications
Despite advances, there is considerable morbidity and mortality associated with sickle cell disease. The many health problems associated with sickle cell anaemia arise because of the red cells’ sickle shape, rigidity, shortened life-span and inefficient oxygen transportation.
Sickle cells tend to clog together, causing occlusion of the smaller blood vessels and intimal hyperplasia of larger vessels, slowing blood flow. If this situation is not rectified, a sickle cell crisis with its associated severe pain, tissue ischaemia and organ damage is the result. A sickle cell crisis can be precipitated by: hypoxia, dehydration, sudden changes in temperature, physical activity (causing tissue anoxia), extreme fatigue, acidosis, infection, stress and anxiety, pregnancy or physical trauma.
Some indicators of severe sickle cell disease include hand-foot syndrome before the age of one year, a haemoglobin level of less than 7g/dL (normal levels are between 12 and 18g/dL) and a raised white cell count in the absence of infection. Symptoms of sickle cell anaemia are described in Panel 1.

Screening
Ideally, people from at-risk ethnic groups who wish to have children should be screened to detect their Hb type. Where both potential parents are identified as having a sickle cell or other trait, they are offered counselling. Where Hb type has not previously been identified, this screening is offered at antenatal clinics. As a result of the NHS Plan, universal antenatal screening now takes place in many parts of the UK. Potential carriers of the sickle gene should also be screened before anaesthesia and surgery.
Today’s multicultural society means that it is increasingly difficult to predict which new-born babies are at risk of sickle cell disease. A phased programme (due to be completed by the end of this year) is currently being rolled out, where all babies in England are screened for sickle cell disease at six days old as part of the neonatal screening tests.3
Symptoms of sickle cell disease do not appear until some three months after birth. This is because fetal haemoglobin (HbF) dilutes any HbS and prevents the sickling mechanism. As the baby grows, the HbF gradually disappears, allowing the sickling mechanism to develop. By adulthood, HbF production has usually stopped completely. Most of the serious complications from sickle cell anaemia occur in the first two years of life. Early diagnosis is vital, allowing treatment to be started immediately and maximising its benefits. This reduces the incidence of later complications.
Management of sickle cell anaemia
Much can now be done to improve patient quality of life and reduce the incidence of crises and complications that arise as a result of infection and vessel occlusion. Regular health maintenance is critical and patients should have frequent health checks. They and their families should be taught to recognise early warning signs of impending crises, infection and organ damage. Although people with sickle cell anaemia should be helped to live as normal a life as possible, they should take practical precautions to reduce the incidence and severity of crises (see Panel 2).

Pharmacological management
The mainstay of pharmacological management of patients with sickle cell anaemia include vaccinations, prophylactic antibiotics and analgesics.
Immunisations
The poorly developed immune system in sickle cell anaemia means that it is vital for babies to receive all the recommended childhood immunisations, plus pneumococcal vaccine (although this does not protect against all strains of pneumococci). A polyvalent pneumococcal polysaccharide conjugated vaccine (Prevenar) has been especially developed for use in children aged between two months and two years of age and who are at special risk of pneumococcal disease. Children over two years of age may be given the unconjugated polyvalent pneumococcal polysaccharide vaccine (Pneumovax II or Pnu-Imune).
Prophylactic antibiotics
At around two months of age, babies with sickle cell anaemia should begin taking phenoxymethy penicillin. This significantly reduces the morbidity and mortality associated with infection in children aged under five years. Twice daily dosing is preferred, but if compliance is an issue, once daily dosing is acceptable. There is some disagreement about the duration of prophylaxis with penicillin and whether it should be for the first five or six years of life or throughout life. Erythromycin tends to be used for patients who are allergic to penicillin.
Folic acid
Folic acid supplements are sometimes recommended for people with sickle cell anaemia if normal dietary levels are not sufficient to keep up with the manufacture of red blood cells. Some centres give 5mg a day to their patients, especially children, but others consider supplementation less critical because the UK diet tends to be folate rich.
Analgesics
Most patients manage their pain at home and only go to hospital if the pain becomes unbearable. Uncontrolled pain accounts for 90 per cent of sickle cell patient hospital admissions. Patients and parents of children with sickle cell anaemia follow ananalgesic ladder of pain management (see Figure 1 for an example).

Self-help measures include rest, keeping warm and increasing fluid intake. Pharmacists should be sensitive to the anxiety and stigma some patients with sickle cell anaemia feel about needing to take analgesics. Patients may be concerned about having inadequate analgesia and having to suffer long periods of pain as a consequence. Some worry that others might think they are addicts.
Complementary therapies, such as massage, aromatherapy and cognitive behavioural therapy, have all proved helpful in dealing with chronic and recurrent pain.
Blood transfusions
Where sickling crises occur frequently, or where there is splenic enlargement or haemolytic anaemia, blood transfusions are given to increase the number of normal red blood cells. It has also been demonstrated that regular transfusions prevent further strokes in children who have suffered at least one stroke. However, regular blood transfusions can lead to iron overload and its subsequent risk of cardiac complications. This problem is treated with an iron chelating drug, such as desferrioxamine or, less frequently, deferiprone.
Patients with severe sickle cell anaemia maybe offered bone marrow transplantation.
Hydroxycarbamide
Hydroxycarbamide has been shown to restimulate fetal haemoglobin production, so reducing organ damage and maintaining splenic function. It is sometimes used for patients with severe and frequent crises. However, its use in sickle cell anaemia is unlicensed.
Hydroxycarbamide is well tolerated in children but regular blood tests are needed to screen for cytopenias, particularly neutropenia. This toxic effect is reversed if treatment is stopped. Hydroxycarbamide capsules can be made into a suspension for once daily administration. Starting doses (15mg/kg/day) may be increased by 5mg/kg/day until crises are controlled or the dose is not tolerated. Both males and females must stop taking hydroxycarbamide at least six months before a planned pregnancy.
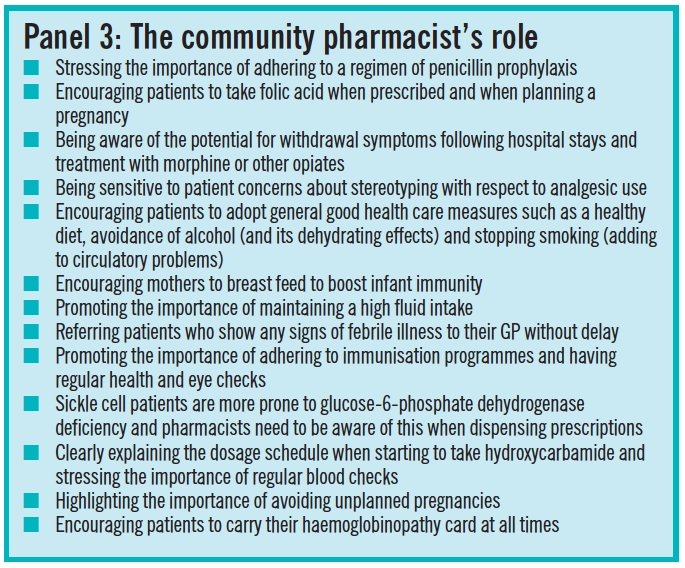
There has been a shift in the care of sickle cell patients from hospitals to the community and there are now 37 sickle cell and thalassaemia centres in cities (15 in London) across the UK, supporting patients and their families. Patients with sickle cell anaemia will be regular visitors to the pharmacy to obtain their prescriptions and for minor ailment guidance. Panel 3 suggests the role pharmacists can play in the care of these patients.
Useful website
- www.sicklecellsociety.org
- www.sickle-thalassaemia.org
- www.blackhealthcare.com/bhc/sicklecell
References
- Claster S, Vichinsky EP. Managing sickle cell disease. Available at: www.studentbmj.com/issues/03/12/education/450.php(accessed 9 June 2005)
- National confidential enquiry into patient outcome and death. Sickle cell and thalassaemia study. Available atwww.ncepod.org.uk/pdf/current/Sickle/protocol.pdf (accessed 28 June 2005)
- Institute of Biomedical Science. Neonatal screening for sickle cell disease. Available at:www.ibms.org/index.cfm?method=science.haematology&subpage=haematology_sickle_cell_disease (accessed 9 June 2005).
Acknowledgement
Thanks to Vanita Jivanji, sickle cell nurse counsellor, at the Leicester Sickle Cell Centre for her advice.
Action: practice points
Reading is only one way to undertake CPD and the Society will expect to see various approaches in a pharmacist’s CPD portfolio.
- Read the section on pneumococcal vaccines in the British National Formulary (section 14.4).
- Find out if there is a sickle cell centre near you and make contact with the nurse counsellor.
- Find out which drugs and foods pose a risk in patients with a glucose-6-phosphate dehydrogenase deficiency (see section 9.1.5 in the BNF).
Evaluate
For your work to be presented as CPD, you need to evaluate your reading and any other activities. Answer the following questions: What have you learnt? How has it added value to your practice? (Have you applied this learning or had any feedback?) What will you do now and how will this be achieved?


