
Jim Varney / Science Photo Library
Pharmacy and other healthcare professionals involved in delivering NHS and non-NHS services, as well as those involved in research and academia, need to have an understanding of sustainability and transformation plans (STPs). These are the plans by which the NHS will deliver the ‘Five year forward view’[1]
by 2020/21 to drive improvements in health and care, restore and maintain financial balance, and deliver core access and quality standards[2]
.
The purpose of this article is to provide pharmacy and healthcare professionals across all care settings with an overview of STPs, the process and some practical guidance on working with them.
What are STPs?
The NHS ‘Five year forward view’ was published on 23 October 2014 and details a new shared vision for the future of the NHS based around the new models of care[1]
. It was developed by all partner organisations that deliver and oversee health and care services.
To support delivery of the ‘Five year forward view’, STPs were announced in NHS shared planning guidance 2016/2017–2020/2021 in December 2015[3]
, which outlined a new approach to help ensure that health and care services are built around the needs of local populations.
In spring 2016, local health and care systems came together to form 44 areas in England that have been identified as geographical STP ‘footprints’[4]
(‘Table 1: The 44 sustainability and transformation plan footprints’). Each of these geographic footprints will be responsible for the delivery of plans to improve local health and care based on the needs of their local populations. The average population size for a footprint is 1.2 million people[5]
,[6]
.
The scope of STPs is broad. The plans will need to show how local services will evolve and become sustainable over the next five years, with a focus on integrating social care — ultimately delivering the ‘Five year forward view’ by:
- Improving quality;
- Developing new models of care;
- Improving health and wellbeing;
- Improving efficiency of services.
STP leaders
Each STP has a named individual who has agreed to convene the STP process and oversee the development of local plans[7]
. These individuals have been selected following local discussions about who is best placed to deliver this role, together with discussions with national bodies. Most leaders are also current chief executives or chief officers of clinical commissioning groups (CCGs), NHS trusts or foundation trusts. A few leaders are from local government or organisations within their footprint.
NHS England states that “STP footprints are not statutory bodies, but collective discussion forums which aim to bring together health and care leaders to support the delivery of improved health and care based on the needs of local populations. They do not replace existing local bodies, or change local accountabilities”[8]
.
This is a critical point, because it emphasises how important leadership will be for success. Leaders across the profession will need to deploy skills, which require them to draw upon their networks and relationships to influence outside the sphere of their individual organisations. System leaders[9]
have the ability to motivate people and managers across organisational boundaries – and as we move towards delivering the ambition of a truly integrated NHS and pharmacy service, this will be the only way it can be achieved. Pharmacy leaders are also encouraged to develop an inclusive, person-centred, coherent vision. The vision should inspire others to act and build trust across professions and patients to address the local health and care needs.
STP implementation
All 44 STPs were published by 15 December 2016[10]
and are now available on the NHS England website[11]
. The process so far has focused on planning, with published STP footprints falling into different categories depending on how ‘ready’ they are. Progress made on the plans in different areas is highly dependent on local context and the history of collaboration between organisations and leaders.
However, the real challenge will be in turning these plans into a reality. To support this process and help local organisations plan more strategically, NHS England and NHS Improvement have published this year’s operational and contracting planning guidance[2]
three months earlier than usual.
For the first time, the planning guidance covers two financial years, to provide greater stability and support transformation. This is underpinned by a two-year tariff and two-year NHS Standard Contract[12]
. It provides local NHS organisations with an update on the national priorities for 2017/18 and 2018/19, as well as updating longer term financial challenges for local systems. Simply put, this is the mechanism for how STP plans will be implemented.
As of April 2017, each STP will have financial ‘control total’ (a target) that will be a summation of all the individual organisational control totals. All organisations will be responsible for delivering both sets of targets, unless otherwise locally agreed with NHS England and NHS Improvement by application. This is to ensure perverse financial incentives and organisational boundaries do not impede transformation.
Consequently, not implementing STPs will have a wide-ranging impact on health and care services. Ultimately, this would mean the ‘Five year forward view’ will not be delivered as intended, which will negatively impact the safety, quality, patient outcomes and sustainability of services provided by organisations. There is a growing consensus that the NHS is not sustainable in its current state so, for the benefit of patients and the wider health economy, it is important that pharmacists and healthcare professionals all play our part in ensuring STPs are a success.
What does this mean for pharmacists and healthcare professionals?
Over the last 12 months, there have been significant developments and activity from national bodies, with local and regional engagement (see ‘Figure 1: Policy timeline’). This has resulted in a number of key national policies and guidance to help pharmacy professionals and leaders in the system to implement the changes required.
For the purpose of this article, the contents of each of the publications will not be explored. Instead the focus is on the common thread running through the narrative of each publication: a drive to improve the value and outcomes patients receive from their medicines. In order to achieve this, a number of things need to happen:
- Improving productivity and performance in the way pharmacies operate (i.e. looking at individual processes and functions). This could include collaborating across STP footprints with pharmacy providers, to integrate and optimise procurement and distribution pathways;
- Reducing unwarranted variation and improving clinical efficiency (i.e. striving for a certain quality that all patients and healthcare professionals can expect from pharmacy services). Appropriate training and support, promoting research, sharing practice, and using data to drive improvement are some ways that this could be achieved;
- Integrating care across existing organisational boundaries (i.e. developing innovative models across primary and secondary care). This will involve collaborative discussions between all healthcare professionals irrespective of sector of practice;
- Optimising the pharmacy workforce to improve the use of medicines (i.e. developing a workforce with the correct knowledge, skills and behaviours for today’s NHS). This involves the whole workforce, from undergraduate to consultant level practice and beyond. There is also an opportunity to optimise the skill mix, not only across pharmacists and pharmacy technicians, but to wider healthcare professionals. Pharmacists are increasingly taking on roles traditionally performed by medical colleagues, including prescribing;
- A greater emphasis on the population being served (i.e. focussing on what patients in local areas need). NHS RightCare have supplied data to support areas with this[13]
. STPs are a recognition that there is no “one size fits all” model. For example, patient needs in Devon will differ to those in south-east London (see ‘Figure 2: Case study – a healthier south-east London (SEL) sustainability and transformation plan (STP) “plan on a page” ’).
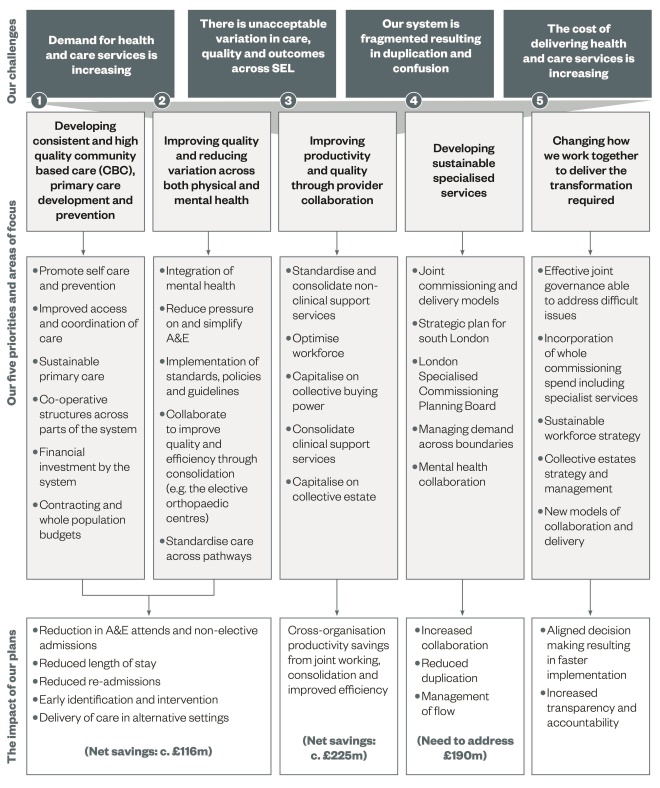
Figure 2: Case study – a healthier south-east London (SEL) sustainability and transformation plan (STP) ‘plan on a page’
The SEL STP focuses on five priority and related areas of focus that will have the greatest impact on challenges and pressures to collectively address the three gaps of health, quality and finance, while increasing value. SEL – which comprises the boroughs of Bexley, Bromley, Greenwich, Lambeth, Lewisham and Southwark, and the providers located within it – is one of 44 geographical ‘footprints’ identified in England.
Source: South-east London sustainability and transformation plan: http://www.ourhealthiersel.nhs.uk/Downloads/Strategy%20documents/South%20East%20London%20STP%20October%202016.pdf
Each pharmacist and healthcare professional will need to respond to the emergence of STPs. It will require a step-change in the way each individual practises as clinicians or managers, as relationships are strengthened across organisational boundaries to integrate care pathways for patients. Strong leadership is equally important for developing the entire pharmacy workforce in order to deliver the integrated service model required because the current trajectory will most likely lead to failure.
Box 1 provides more details on the steps that pharmacists and healthcare professionals can take to be involved in STPs, while box 2 provides information on how individuals already involved in STPs can engage with and involve other colleagues.
Box 1: Ten proactive steps pharmacists and healthcare professionals can take to be involved in sustainability and transformation plan (STPs)
1. Read your local STP and do not be disenfranchised if there is a lack of ‘pharmacy’ or ‘medicines’ mentioned within the narrative. Medicines is cross-cutting and there are few, if any, work streams that will not be influenced by pharmacy services.
2. Understand your local population by listening to patients and gathering intelligence on local information, such as benchmarking data, medicines optimisation dashboards, Atlas of Variation (data collected by the NHS to investigate variation in healthcare delivery in different regions).
3. Collaborate with local pharmacy and healthcare leaders in your footprint. It is important to ensure that this a multi-professional process and pharmacy professionals are aligned to a common vision.
4. Arrange a meeting with a member of the executive team of the STP, senior responsible officer (SRO) of the relevant work stream or programme manager and offer real solutions.
5. Develop a collaborative strategic plan that supports the local STP. Provide clarity on the return on investment in cases for change, because restoring and maintaining financial balance is a priority.
6. Develop an operational delivery plan, with defined work streams and appropriate governance — with clear lines of reporting and accountability for delivery.
7. Make the case for dedicated programme management because the ambition and opportunity within pharmacy and medicines is far too great to be added onto many existing pharmacy leader’s current job roles. This may be a project manager, or clinical lead for the programme of work. Their role would be to provide strategic review; partner engagement; developing a collaborative plan; and ensuring it is on course for delivery.
8. Be clear on the national and local policy context in which you are operating and developing services.
9. Begin to showcase and build on existing success within the organisations of an STP. Spread of practice from areas where they are already operating would support the pace of delivery required.
10. Most importantly, keep in constant communication with patients and staff. If this is done effectively, patients and staff can be empowered to make the necessary improvements in the NHS — improving morale, quality, safety and productivity.
Box 2: Supporting other colleagues involved in sustainability and transformation plans (STPs)
Pharmacy professionals can support other colleagues directly involved in implementing STPs by:
- Sharing best practice through local, regional and national networks;
- Using social media to build strong professional networks and communicate progress and best practice nationally;
- Pharmacy professionals should openly offer support and advice to colleagues, supporting and advising them through any challenges they may face;
- Using national and regional conferences to showcase work (even work in progress), as well as to network and learn from others;
- Publishing service improvement work regularly, through articles and blogs, to support others and invite peer feedback;
- Sharing case studies and business cases with the Hospital Pharmacy and Medicines Optimisation Team at NHS Improvement;
- Sharing practice with the Royal Pharmaceutical Society and other professional networks.
Additional resources:
About the author
Rahul Singal is currently the pharmacy and medicines professional programme lead for South East London STP, employed by King’s College Hospitals NHS Foundation Trust. Former clinical fellow to the chief pharmaceutical officer, NHS England. Contact: rahul.singal@nhs.net
Acknowledgments
Roger Fernandes is the chief pharmacist at King’s College Hospital NHS Foundation Trust and Dr Tim Hanlon is the chief pharmacist and clinical director of medicines optimisation at Guy’s and St Thomas’ NHS Foundation Trust. They are joint SMEs (Subject Matter Experts) for the pharmacy and medicines programme for South-East London’s STP. Ravi Baghirathan is deputy director for the strategy group at NHS England. The author would like to acknowledge their feedback and comments on the article drafts.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
References
[1] NHS England, Care Quality Commission, Health Education England, Monitor, Public Health England, Trust Development Authority (2014). NHS ‘Five year forward view’. Available at: www.england.nhs.uk/ourwork/futurenhs/ (accessed February 2017)
[2] NHS England, NHS Improvement (2016). NHS Operational planning and contracting guidance for 2017–2019. Available at: https://www.england.nhs.uk/ourwork/futurenhs/deliver-forward-view/ (accessed February 2017)
[3] NHS England, NHS Improvement (Monitor and Trust Development Authority), Care Quality Commission, Health Education England, Public Health England (2015). NHS Shared planning guidance 2016/2017–2020/2021. Available at: https://www.england.nhs.uk/wp-content/uploads/2015/12/planning-guid-16-17-20-21.pdf (accessed February 2017)
[4] NHS England. Sustainability and transformation plans [Online]. Available at: https://www.england.nhs.uk/ourwork/futurenhs/deliver-forward-view/stp/ (accessed February 2017)
[5] The King’s Fund. Sustainability and transformation plans (STPs) explained. [Online]. Available at: https://www.kingsfund.org.uk/projects/sustainability-and-transformation-plans (accessed February 2017)
[6] NHS England (2016). Sustainability and transformation plan footprints. Available at: https://www.england.nhs.uk/wp-content/uploads/2016/02/stp-footprints-march-2016.pdf (accessed February 2017)
[7] NHS England (2016). Sustainability and transformation leaders confirmed. [Online]. Available at: https://www.england.nhs.uk/2016/03/leaders-confirmed/ (accessed February 2017)
[8] House of Commons (2016). NHS sustainability and transformation plans. Available at: http://researchbriefings.parliament.uk/ResearchBriefing/Summary/CDP-2016-0161 (accessed February 2017)
[9] Timmins N (2015). The practice of system leadership. Being comfortable with chaos. Available at: https://www.kingsfund.org.uk/publications/practice-system-leadership (accessed February 2017)
[10] Eddie S & West D. Mapped: all STPs published – full coverage. Health Services Journal. Available at: https://www.hsj.co.uk/topics/stps/mapped-all-44-stps-published-full-coverage/7013064.article?blocktitle=News-(grid)&contentID=20682 (accessed February 2017)
[11] NHS England. View sustainability and transformation plans (STPS). Available at: https://www.england.nhs.uk/stps/view-stps/ (accessed February 2017)
[12] NHS England. 2016/2017 NHS standard contract. Available at: https://www.england.nhs.uk/nhs-standard-contract/16-17/ (accessed February 2017)
[13] NHS RightCare. Where-to-look packs for STP footprint areas. Available at: https://www.england.nhs.uk/rightcare/intel/cfv/stp-footprints/ (accessed February 2017)
You might also be interested in…

Tackling the NHS drug budget: why we set up a regional collaboration for medicines value

Lack of joined-up working between pharmacy and general practice is ‘nonsensical’, says former BMA chair
