
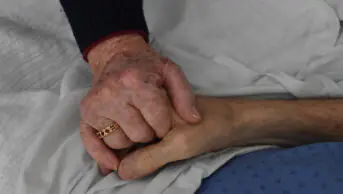
Shutterstock.com
Open access article
The Royal Pharmaceutical Society has made this article free to access in order to help healthcare professionals stay informed about an issue of national importance.
To learn more about coronavirus, please visit: https://www.rpharms.com/resources/pharmacy-guides/wuhan-novel-coronavirus

Source: Shutterstock.com
The changes reported in the survey were attributed to factors such as stock and staffing shortages during the pandemic, a shift towards reduced patient contact and the need for rapid pain relief in people dying from COVID-19
The challenges of the COVID-19 pandemic have led to innovation in anticipatory prescribing (AP) practices within community palliative care, the results of a survey in BMJ Supportive & Palliative Care (16 June 2020) have shown[1]
.
The survey, which enquired about local changes to drug prescription, administration, and support structures for AP during the COVID-19 pandemic, was completed by 261 clinicians in community, hospice and hospital settings in the UK and Ireland in April 2020.
Many clinicians reported changes to route of administration, such as to oral/buccal routes from subcutaneous injections (47%), and the type (38%), total quantities (35%) and dosages of medicines prescribed (29%). Allowing family members or social care workers to administer AP medicines — often by buccal, sublingual or transdermal routes — was reported by 37% of clinicians, and implementing remote telephone or video assessments was reported by 63% of clinicians.
AP involves dispensing medicines in advance of clinical need, so staff can quickly respond to the needs of people at the end of life. The changes reported in the survey were attributed to factors such as stock and staffing shortages during the pandemic, a shift towards reduced patient contact and the need for rapid pain relief in people dying from COVID-19.
“These changes are occurring at pace: it remains to be seen how widely they are implemented, how effective they are and how much they will persist after the pandemic,” the researchers concluded.
References
[1] Antunes B, Bowers B, Winterburn I et al. BMJ Support Palliat Care 2020. doi: 10.1136/bmjspcare-2020-002394
You may also be interested in
Government to ‘strengthen’ out-of-hours support for palliative care services

Support for pharmacies providing palliative care urged as hospices get cash injection
