PerPlex
Around one in six patients fails to get a prescription filled the first time it is prescribed for them by a doctor, according to new research.
A team led by Maria Rubio-Valera of the School of Pharmacy, University of Barcelona, Spain, analysed 2.9 million prescriptions written for 1.6 million patients in Catalonia between July 2013 and June 2014. They found that 17.6% of patients failed to get a prescription filled the first time it was prescribed, a behaviour they describe as initial medication non-adherence (IMNA).
Prescriptions for pain relief accounted for the highest rate of IMNA, with 22.6% of patients not getting their first prescription filled by the end of the month following the one in which it was written. The lowest IMNA rate — 7.4% — was found for prescriptions for angiotensin-converting enzyme inhibitors, the researchers reveal in the British Journal of Clinical Pharmacology
[1]
(online, 24 February 2017).
The researchers also discovered that younger age, American origin, having a pain or mental health disorder and being treated by a locum or trainee GP in a GP training practice were all predictors of IMNA.
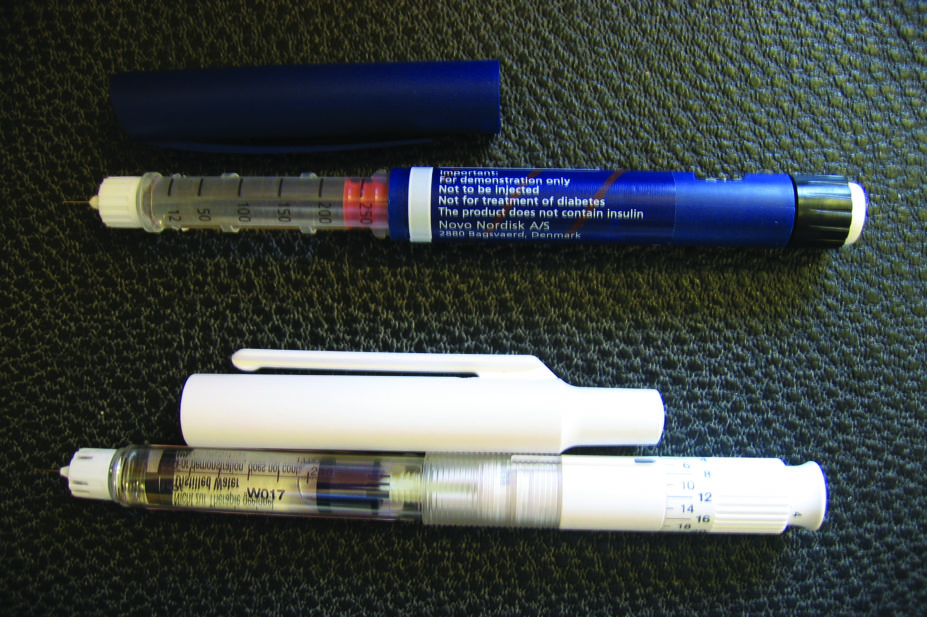
“We are especially concerned about the high rates of initial medication non-adherence in chronic treatments such as insulins, statins, or antidepressants and suspect that it is also related to an increase in costs,” says Rubio-Valera. “These patients had been prescribed these treatments for the first time in a long period. Therefore, it is unlikely that they have the treatment stockpiled and we can be pretty sure that they will not initiate these treatments.”
The researchers suggest that improving trust in trainee GPs, ensuring optimum care for vulnerable immigrants and strengthening the motivation of young people to initiate pharmacological treatment should be addressed in primary care, as well as explaining the importance of not abandoning a newly prescribed medication.
They suspect that non-adherence to treatment is related to an increase in costs but Rubio-Valera says their findings are likely to be applicable to other health systems, such as the NHS in the UK.
“The Catalan and British primary care [systems] have similar structures and funding mechanisms,” says Rubio-Valera, adding that guidelines for the management of diseases in primary care in Catalonia are commonly based on the recommendations of England’s National Institute for Health and Care Excellence (NICE).

Source: Courtesy Dr Prashanth Patel
Prashanth Patel, consultant metabolic physician and chemical pathologist, says the study is a “timely reminder of the extent of non-adherence among patients–one of the biggest unaddressed issues in modern medicine.”
Prashanth Patel, consultant metabolic physician and chemical pathologist at University Hospitals of Leicester NHS Trust, says the study is a “timely reminder of the extent of non-adherence” among patients.
“If lack of persistence to treatment is also added to INMA, it is estimated that 40–50% of patients with chronic disease are non-adherent to their treatment and it is one of the biggest unaddressed issues in modern medicine,” he says.
Patel points out that the issue of non-adherence is not assessed in around 40% of medical consultations, adding that indirect measures of non-adherence, such as pharmacy pick-up rates, may not reflect a patient’s current medication-taking behaviour.
“Simple and objective direct measures such as biochemical screening in urine, in our experience, help provide confidence to the healthcare provider to discuss non-adherence with patients.” Once non-adherence has been established it can then be addressed holistically, taking into account patient beliefs and understanding of their illnesses, Patel adds.
Rubio-Valera’s team is now conducting a qualitative study with initially non-adherent primary care patients to assess their motivations for initial medication non-adherence and to develop interventions to deal with the problem.
“We need to involve primary care professionals — general practitioners and nurse practitioners — [including] community pharmacists so that all health professionals have shared criteria,” says Rubio-Valera. “Patients trust their community pharmacists and pharmacists appear to be a factor that influences the patient decision. The patients need to be reassured about a new treatment and inconsistent recommendations can generate distrust in the treatment and the system.”
References
[1] Aznar-Lou I, Fernández A , Gil-Girbau M et al. Initial medication non-adherence: prevalence and predictive factors in a cohort of 1.6 million primary care patients. Br J Clin Pharmacol doi: 10.1111/bcp.13215


