DRdoubleB / Wikimedia Commons
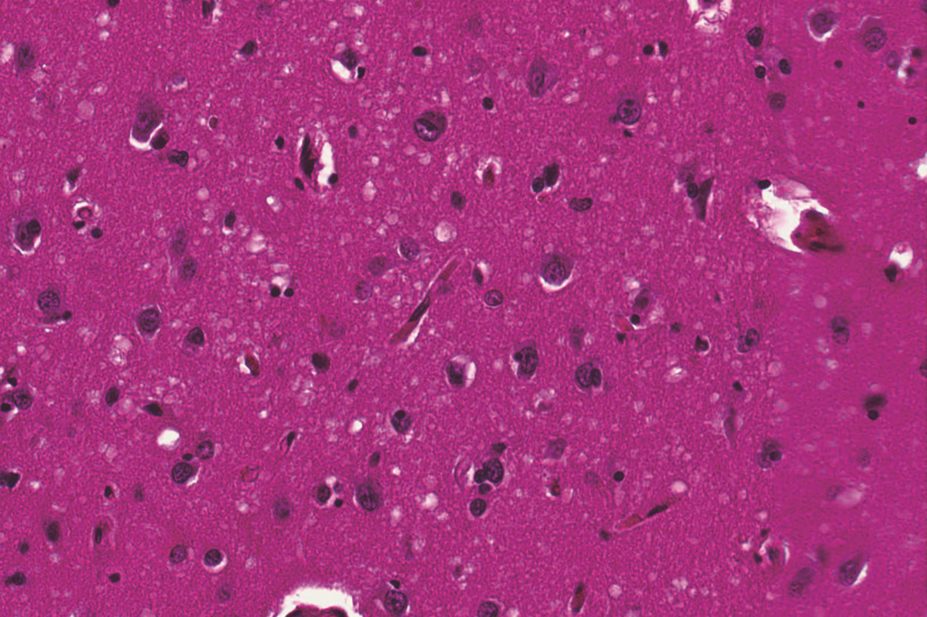
The brains of Creutzfeldt–Jakob disease (CJD) victims show evidence of Alzheimer’s pathology, new research suggests. But neuroscientists have dismissed concerns that people can “catch” Alzheimer’s by becoming infected with the “seeds” of the condition through surgery involving contaminated instruments or blood transfusions.
A study published in Nature
[1]
on 9 September 2015 reported autopsy results from the brains of eight people aged 36–51 years who died of CJD after receiving contaminated growth hormone injections. In four subjects, there was evidence of moderate to severe amyloid-β pathology; amyloid-β is one of the abnormal proteins associated with Alzheimer’s disease.
None of the patients carried genes known to be associated with early-onset Alzheimer’s disease and none had exhibited symptoms of the condition. The researchers also analysed pituitary glands from the individuals with amyloid-β brain pathology and found marked amyloid-β deposition in multiple cases.
Around 450 people around the world have died from CJD after receiving treatment, usually in childhood, with growth hormone harvested from the pituitary glands of human cadavers contaminated with prions – a treatment which ceased in 1985 after the risks of CJD became known.
The researchers behind the Nature paper say their findings suggest that, in addition to CJD, healthy exposed individuals may also be at risk of iatrogenic Alzheimer’s disease. They cite another study, published in Brain
[2]
on 12 August 2015, as evidence that prion disease itself does not appear to predispose an individual to Alzheimer’s disease. The Brain study showed minimal or no amyloid-β pathology at autopsy in 116 patients with other prion diseases, who were of a similar age or a decade older and did not carry the APOE ε4 allele.
But several neuroscientists have questioned the researchers’ conclusion.
Masud Husain, professor of neurology and cognitive sciences at the University of Oxford, says the results do not provide sufficient evidence to support the concept of Alzheimer’s disease being a transmissible illness. “The authors argue that the prion (CJD) pathology and the amyloid (Alzheimer) pathology are effectively independent,” he says. “Stronger evidence would be required to accept such a proposal.”
David Allsop, professor of neuroscience at the University of Lancaster, says the conclusion is an extrapolation: “What the paper shows is that some people treated with human growth hormone who subsequently went on to develop CJD also show evidence of β amyloid deposits, a key feature of Alzheimer’s disease, in their pituitary glands. What the paper does not demonstrate is whether these people would have gone on to develop Alzheimer’s disease had they lived long enough or that their pituitary β amyloid deposits were caused by contamination of growth hormone with a ‘rogue’ form of β amyloid.”
Allsop suggests that a likely explanation is that deposition of the ‘prion protein’ in CJD can result, in some cases, in the co-accumulation of β amyloid.
“It is very well known from other studies that one type of rogue protein — in this case the prion protein — can predispose to accumulation of another [in this case β amyloid],” he says. “There is no evidence that Alzheimer’s disease can be transmitted from one person to another, or through use of contaminated surgical instruments, and these results should be interpreted with a great deal of caution.”
This reassurance has been echoed by chief medical officer, Dame Sally Davies, who says there is no evidence that Alzheimer’s disease can be transmitted in humans or through any medical procedure.
“I can reassure people that the NHS has extremely stringent procedures in place to minimise infection risk from surgical equipment, and patients are very well protected.”
References
[1] Jaunmuktane Z, Mead S, Ellis M et al. Evidence for human transmission of amyloid-β pathology and cerebral amyloid angiopathy. Nature 2015;525:247–250.
[2] Rudge P, Jaumuktane Z, Adlard P et al. Iatrogenic CJD due to pituitary-derived growth hormone with genetically determined incubation times of up to 40 years. Brain 2015. doi:http://dx.doi.org/10.1093/brain/awv235.
You may also be interested in

Headache: recognition and management

Cannabinoids have limited impact on MS symptoms