
Alex Segre / Alamy
A more efficient drug withdrawal process could cut the number of avoidable deaths attributable to drugs, according to an investigation published in BMC Medicine
[1]
on 5 February 2015.
The average time it has taken for a drug to be withdrawn following deaths attributable to it — which applied to virtually a quarter of all withdrawals between 1950 and 2013 — has remained constant at four years since the middle of the last century.
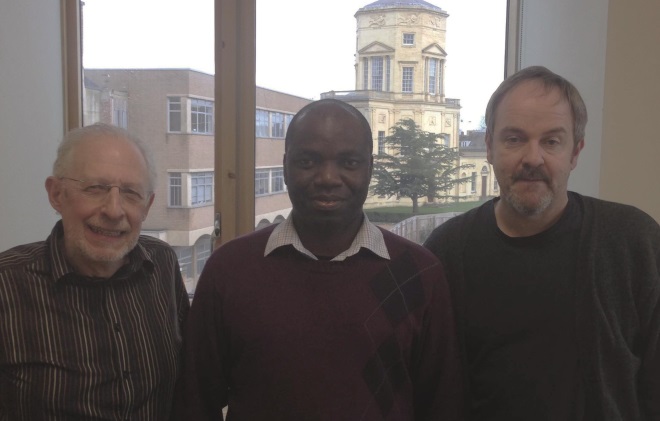
Source: Centre for Evidence-Based Medicine, University of Oxford
From left, Jeffrey Aronson, Igho Onakpoya and Carl Heneghan from the Centre for Evidence-based Medicine at Oxford University
A team of researchers led by Igho Onakpoya at the Centre for Evidence-Based Medicine at University of Oxford argue that regulators should expedite investigations and consider early suspensions whenever deaths are suspected of being due to adverse drug reactions.
The study analysed the delays involved in the decisions to withdraw drugs post-marketing in all cases where a death was involved, and the worldwide patterns of these withdrawals. The data were collated from several databases, including the World Health Organization’s Consolidated List of Medicinal Products, and the relevant data published by the US Food and Drug Administration, the European Medicines Agency, and the UK Medicines and Healthcare products Regulatory Agency, as well as the PubMed, Medline and Google Scholar searchable databases.
Of the 407 medicines withdrawn from the market in at least one country during 1950–2013, 95 drugs were identified for which death was specifically documented as a reason for market withdrawal (all between 1957 and 2011). Most of the drugs were for treating neurological or psychiatric disorders, followed by painkillers and anti-inflammatory drugs.
The key findings were that, over time, deaths have been reported sooner after launch, and that the gap between launch date and withdrawal has shortened — though in 47% of cases, more than two years elapsed between the first report of a death and withdrawal of the drug. All in all, however, “the interval between the first report of a death attributed to a medicinal product and eventual withdrawal of the product has not improved over the last 60 years [since 1957]”, averaging four years, the researchers found.
The data also reveal that 40% of the 95 drugs were withdrawn in more than one country; 16 (17%) remained on the market in at least one country; and only 26 (27%) were withdrawn from all countries they were sold in. Underlining the international discrepancies, significantly fewer withdrawals were recorded in Africa (5.3%) and Asia, than in the United States and Europe.
“Some deaths associated with these products could have been avoided,” the researchers conclude. As well as calling on manufacturers and regulatory authorities to expedite investigations and suspensions when deaths appear to be due to adverse drug reactions, they argue that the system should be supported by greater transparency regarding clinical trials data and better international coordination.


