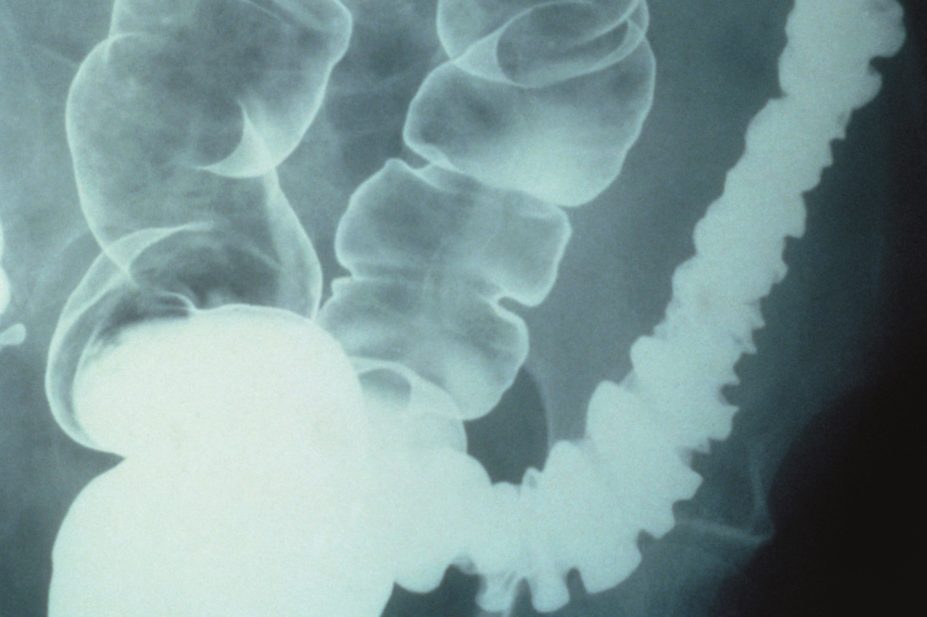
CNRI / Science Photo Library
The US Food and Drug Administration (FDA) has approved two new treatments for patients with irritable bowel syndrome with diarrhoea (IBS-D).
Rifaximin (marketed as Xifaxan by Salix Pharmaceuticals) is an antibiotic, and eluxadoline (marketed as Viberzi by Actavis) is an antagonist and agonist of the δ and µ opioid receptors, respectively. Eluxadoline has been approved as a first-line treatment for the condition. Rifaximin is already available as an antibiotic in Europe for other conditions.
Anton Emmanuel, a gastroenterologist at University College Hospital in London, says rifaximin treatment for IBS-D is based on the theory that some people with the condition have an imbalance of bacteria in the gut. “This is a controversial theory,” he says. Some researchers in the United States believe that all patients with IBS have this imbalance. “In the UK and Sweden we’ve found it to be closer to around 15–20% of patients,” says Emmanuel.
The FDA considered two phase III studies, in which 1,258 patients were given rifaximin or placebo. In the four weeks after treatment, 40.7% of the patients given rifaximin and 31.7% of the placebo patients had relief of IBS symptoms (P<0.001).
Rifaximin is currently used to treat recurring overt hepatic encephalopathy, in which the liver is unable to detoxify blood and which can result from infections in the gut. It is used in this instance because it remains mostly in the digestive tract and is not absorbed into the blood stream, thereby minimising side effects.
But Emmanuel raises the question about how long patients can be treated as “the effect of these antibiotics inevitably starts to wear off”. The recommended treatment course for IBS-D is three tablets daily for two weeks. If there is a recurrence, patients can be retreated up to two times. “It’s quite intrusive for the patient,” adds Emmanuel.
The most common side effects of rifaximin are nausea and an increase in the liver enzyme alanine aminotransferase. Another recognised side effect, as with other antibiotics, is Clostridium difficile infection.
Eluxadoline, the other drug to be licensed by the FDA for IBS-D, has mixed opioid receptor activity and is described by its manufacturer Actavis as a first-in-class drug.
“Antagonism of the δ opioid receptor is supposed to decrease the pain associated with IBS-D. And agonism of the µ opioid receptor slows down contractions of the bowel, working on diarrhoea,” says Emmanuel.
The FDA has granted eluxadoline a first-line licence, even though it has not undergone direct comparison trials with existing treatments, such as loperamide. Emmanuel says he “certainly wouldn’t use it first-line”.
In two phase III trials, involving 2,425 patients, eluxadoline was more effective than placebo at simultaneously reducing abdominal pain and improving stool consistency over 26 weeks of treatment.
The most common side effects in patients treated with eluxadoline include constipation, nausea and abdominal pain. In more serious cases, the drug can cause spasm in the sphincter of Oddi, located in a shared portion of the bile and pancreatic ducts, which can lead to pancreatitis. It is therefore not recommended for patients with a history of bile duct obstruction, pancreatitis, severe liver impairment, or severe constipation and for people who drink more than three alcoholic drinks per day.
In Europe, drug companies must carry out a study in children before gaining a licence from the European Medicines Agency (EMA), unless a waiver has been obtained. Actavis has had a paediatric investigation plan for 6–18 year olds approved by the EMA but has also been granted a deferral, meaning that it does not need to complete the study before applying for a licence in adults. The manufacturer has not yet submitted the medicine for approval.