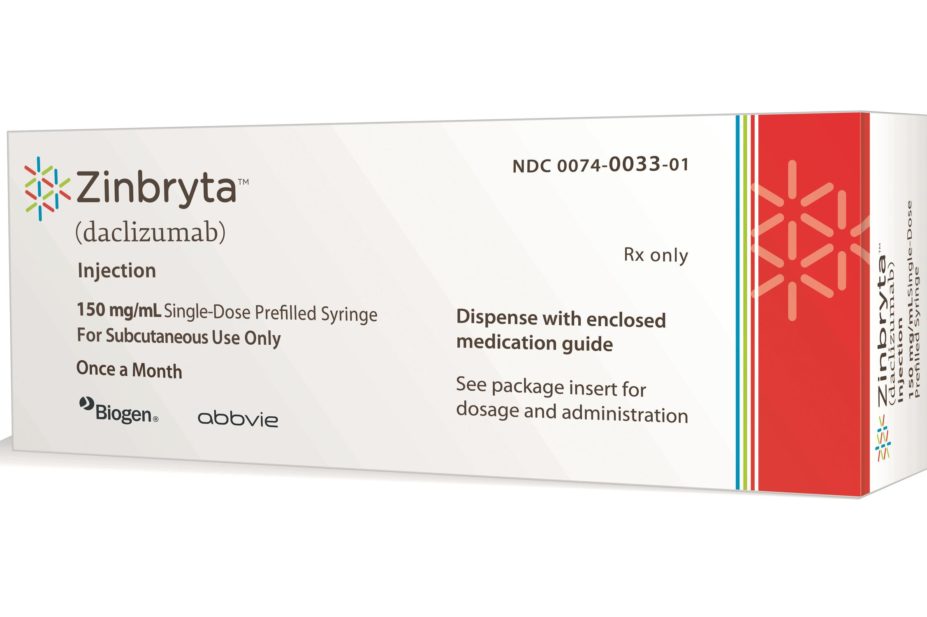
Courtesy of Biogen
Zinbryta (daclizumab), the first once-monthly self-administered injection for multiple sclerosis (MS), has been approved by the US Food and Drug Administration.
The injection can be used in adults with relapsing forms of multiple sclerosis and will be co-marketed by Biogen and AbbVie. However, the FDA, which is responsible for evaluating the safety and efficacy of medicines in the United States, has recommended that the drug is prescribed only to patients who have had an “inadequate response to two or more MS drugs” because of serious safety concerns, including liver injury and immune conditions.
Because of these risks, the drug comes with a boxed warning – the FDA’s most serious warning label – and will be available only through prescribers, pharmacies and patients enrolled in the Zinbryta risk evaluation and mitigation strategy programme.
The boxed warning says daclizumab can cause severe liver injury, including life threatening and fatal events, so blood tests to monitor liver function should be performed prior to starting treatment with it, and then monthly before each dose, and for up to six months after the last dose.
The warning also highlights other important risks of treatment, including immune conditions, such as non-infectious colitis, skin reactions, and enlargement of lymph nodes. Additional risks that have been highlighted include hypersensitivity reactions, increased risk of infections, and symptoms of depression and/or suicidal ideation.
The efficacy of daclizumab was shown in two clinical trials. In the first, said to be the largest and longest head-to-head phase III trial ever conducted in MS, daclizumab significantly reduced the annualised relapse rate (ARR) by 45% compared to interferon beta-1a (Avonex) in 1,841 patients treated for up to 144 weeks. At the end of the study, 67% of patients taking daclizumab were relapse free compared to 51% of the patients taking interferon beta-1a. In the second trial, which involved 412 patients, the ARR was reduced by 54% in patients taking daclizumab compared to placebo.
The most common adverse drug reactions (ADRs) reported by patients receiving the drug in the head-to-head trial were cold symptoms, upper respiratory tract infection, dermatitis, throat pain and eczema, while ADRs reported in the second, placebo-controlled trial included depression, rash and increased levels of alanine aminotransferase.

Courtesy of Biogen
Zinbryta, which can be used in adults with relapsing forms of multiple sclerosis, will be co-marketed by Biogen and AbbVie. Pictured, Biogen’s headquarters in Cambridge, Massachusetts
Although its precise mode of action is unknown, daclizumab is thought to work differently from other disease-modifying therapies by binding to CD25, a sub-unit of the interleukin-2 (IL-2) receptor found on activated lymphocytes, cells believed to underlie the biology of MS.
In April 2016, the European Medicines Agency’s Committee for Medicinal Products for Human Use recommended marketing authorisation be granted for daclizumab in the EU. That opinion has been referred to the European Commission for a final decision.
Sally Hughes, programme director of policy and external relations at the MS Society, said: “More than 100,000 people live with MS in the UK and it’s important they are able to access the right treatment for them at the right time. The National Institute for Health and Care Excellence (NICE) is currently appraising daclizumab for use on the NHS. As part of the MS Society’s ‘Treat Me Right’ campaign, we’ll be submitting evidence into this appraisal. We’re also monitoring further recommendations from the EMA on who may benefit from the treatment.”